| [1] 王谨.乌梅含漱液对头颈部肿瘤患者放射性口干症的临床应用研究[D].广州中医药大学,2015.[2] 陈小章,王子栋.外分泌生理学基础与临床[M]. 2版. 北京:科学出版社,2011:281.[3] 谢秀荣. 基于酸甘化阴理论乌梅喷雾剂对放射性口干症的研究[D].广州中医药大学,2016.[4] Abedi SM,Yarmand F,Motallebnejad M,et al. Vitamin E protects salivary glands dysfunction induced by ionizing radiation in rats.Arch Oral Biol.2015;60(9):1403-1409.[5] Li Z,Wang Y,Xing H,et al. Protective efficacy of intravenous transplantation of adipose-derived stem cells for the prevention of radiation-induced salivary gland damage.Arch Oral Biol.2015 ;60(10):1488-1496.[6] Kamiya M,Kawase T,Hayama K,et al. X-Ray-Induced Damage to the Submandibular Salivary Glands in Mice: An Analysis of Strain-Specific Responses.Biores Open Access. 2015; 4(1):307-318.[7] Fang D,Hu S,Liu Y,et al. Identification of the active components in Bone Marrow Soup: a mitigator against irradiation-injury to salivary glands.Sci Rep.2015;5:16017.[8] Cakmak Karaer I,Simsek G,Yildiz A,et al. Melatonin's protective effect on the salivary gland against ionized radiation damage in rats.J Oral Pathol Med.2016;45(6):444-449.[9] Marmary Y,Adar R,Gaska S,et al. Radiation-Induced Loss of Salivary Gland Function Is Driven by Cellular Senescence and Prevented by IL-6 Modulation.Cancer Res.2016;76(5):1170-80.[10] Lopez-Jornet P,Gómez-García F,et al. García Carrillo N,Radioprotective effects of lycopene and curcumin during local irradiation of parotid glands in Sprague Dawley rats.Br J Oral Maxillofac Surg.2016;54(3):275-279.[11] Zeidan YH,Xiao N,Cao H,et al. Botulinum Toxin Confers Radioprotection in Murine Salivary Glands.Int J Radiat Oncol Biol Phys.2016;94(5):1190-1197.[12] Teos LY,Zheng CY,Liu X,et al. Adenovirus-mediated hAQP1 expression in irradiated mouse salivary glands causes recovery of saliva secretion by enhancing acinar cell volume decrease.Gene Ther.2016;23(7):572-579.[13] Hai B,Zhao Q,Qin L,et al. Rescue Effects and Underlying Mechanisms of Intragland Shh Gene Delivery on Irradiation-Induced Hyposalivation.Hum Gene Ther.2016; 27(5):390-399[14] Choi JS,An HY,Park IS,et al. Radioprotective Effect of Epigallocatechin-3-Gallate on Salivary Gland Dysfunction After Radioiodine Ablation in a Murine Model.Clin Exp Otorhinolaryngol.2016; 9(3):244-251.[15] Sadiç M,Korkmaz M,Gültekin SS,et al. Alterations in ADAMTS12 gene expression in salivary glands of radioiodine-131-administered rats.Nucl Med Commun. 2016;37(10):1010-1015.[16] Konak M,Cincik H,Erkul E,et al. The protective effects of different treatments on rat salivary glands after radiotherapy.Eur Arch Otorhinolaryngol.2016;273(12):4501-4506.[17] Mizrachi A,Cotrim AP,Katabi N,et al. Radiation-Induced Microvascular Injury as a Mechanism of Salivary Gland Hypofunction and Potential Target for Radioprotectors.Radiat Res.2016 ;186(2):189-195.[18] Xu L,Yang X,Chen J,et al. Simvastatin attenuates radiation-induced salivary gland dysfunction in mice.Drug Des Devel Ther.2016;10:2271-2278.[19] Baum BJ,Afione S,Chiorini JA,et al. Gene Therapy of Salivary Diseases.Methods Mol Biol.2017;1537:107-123.[20] Hu L,Wang Y,Cotrim AP,et al. Effect of Tempol on the prevention of irradiation-induced mucositis in miniature pigs. Oral Dis.2017.[21] Shen J,Xu XQ,Su GY,et al. Intravoxel incoherent motion magnetic resonance imaging of the normal-appearing parotid glands in patients with differentiated thyroid cancer after radioiodine therapy. Acta Radiol. 2017:284185117709037.[22] Vissink A, Gravenmade EJ, Ligeon EE, et al. A functional and chemical study of radiation effects on rat parotid and submandibular/sublingual glands. Radiat Res.1990;124(3): 259-265.[23] Burlage FR, Roesink JM, Faber H, et al.Optimum dose range for the amelioration of long term radiation-induced hyposalivation using prophylactic pilocarpine treatment. Radiother Oncol.2008;86(3):347-353.[24] Zeilstra LJ, Vissink A, Konings AW, et al. Radiation induced cell loss in rat submandibular gland and its relation to gland function.Int J Radiat Biol.2000;76(3):419-429.[25] Timiri Shanmugam PS, Dayton RD, Palaniyandi S,et al.Recombinant AAV9-TLK1B administration ameliorates fractionated radiation-induced xerostomia.Hum Gene Ther. 2013;24(6):604-612.[26] Motallebnejad M, Abedi SM, Seyedmajidi M, et al. Evaluation of protective effect of propolis on parotid salivary glands in gamma-irradiated rats.J Contemp Dent Pract.2014;15(1):8-11.[27] Belzile M, St-Amant M, Mathieu D,et al.Radiation-induced xerostomia: is octreotide the solution.J Otolaryngol Head Neck Surg.2009;38(5):545-551.[28] Konings AW, Coppes RP, Vissink A,et al.On the mechanism of salivary gland radiosensitivity. Int J Radiat Oncol Biol Phys2005 Jul 15;62(4):1187-94. Review. Erratum in: Int J Radiat Oncol Biol Phys.2006;64(1):330.[29] 张艳丽,秦丽萍,王凯丽,等.斛芪浸膏对Wistar大鼠涎腺辐射损伤的保护作用[J].中西医结合学报,2011,9(1):70-76.[30] Phillips RM. X-ray-induced changes in function and structure of the rat parotid gland.J Oral Surg.1970;28(6):432-427.[31] Bodner L.Transport of alpha-aminoisobutyric acid into rat parotid after X-irradiation.Int J Radiat Biol.1989;55(4):653-660.[32] O'Connell AC, Redman RS, Evans RL, et al. Radiation-induced progressive decrease in fluid secretion in rat submandibular glands is related to decreased acinar volume and not impaired calcium signaling.Radiat Res.1999;151(2):150-158.[33] 陈波,唐博,邓玉林,等.放射性脑损伤的动物模型及神经组织放射损伤生物学系统研究[J].世界复合医学,2015,1(3):252-258. |
.jpg) 文题释义:
放射性口干症:指接受放疗的头颈部肿瘤患者因其唾液腺受到照射后发生损伤,发生唾液性质和唾液量的改变,并引起口干、黏膜炎等一系列相关症状,远期反应严重者甚至出现吞咽和交谈困难、味觉丧失、龋齿发生及口腔真菌感染等。
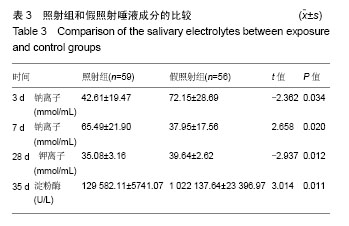
颌下腺指数:又称为颌下腺系数颌下腺指数,能反映腺体的变化情况,指数增大,提示腺体充血、水肿或增生肥大等;指数减小,表示腺体萎缩和其他退行性变产物。
文题释义:
放射性口干症:指接受放疗的头颈部肿瘤患者因其唾液腺受到照射后发生损伤,发生唾液性质和唾液量的改变,并引起口干、黏膜炎等一系列相关症状,远期反应严重者甚至出现吞咽和交谈困难、味觉丧失、龋齿发生及口腔真菌感染等。
颌下腺指数:又称为颌下腺系数颌下腺指数,能反映腺体的变化情况,指数增大,提示腺体充血、水肿或增生肥大等;指数减小,表示腺体萎缩和其他退行性变产物。.jpg) 文题释义:
放射性口干症:指接受放疗的头颈部肿瘤患者因其唾液腺受到照射后发生损伤,发生唾液性质和唾液量的改变,并引起口干、黏膜炎等一系列相关症状,远期反应严重者甚至出现吞咽和交谈困难、味觉丧失、龋齿发生及口腔真菌感染等。
颌下腺指数:又称为颌下腺系数颌下腺指数,能反映腺体的变化情况,指数增大,提示腺体充血、水肿或增生肥大等;指数减小,表示腺体萎缩和其他退行性变产物。
文题释义:
放射性口干症:指接受放疗的头颈部肿瘤患者因其唾液腺受到照射后发生损伤,发生唾液性质和唾液量的改变,并引起口干、黏膜炎等一系列相关症状,远期反应严重者甚至出现吞咽和交谈困难、味觉丧失、龋齿发生及口腔真菌感染等。
颌下腺指数:又称为颌下腺系数颌下腺指数,能反映腺体的变化情况,指数增大,提示腺体充血、水肿或增生肥大等;指数减小,表示腺体萎缩和其他退行性变产物。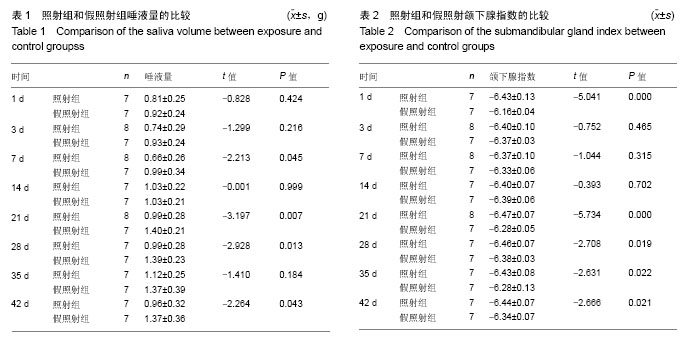

.jpg) 文题释义:
放射性口干症:指接受放疗的头颈部肿瘤患者因其唾液腺受到照射后发生损伤,发生唾液性质和唾液量的改变,并引起口干、黏膜炎等一系列相关症状,远期反应严重者甚至出现吞咽和交谈困难、味觉丧失、龋齿发生及口腔真菌感染等。
颌下腺指数:又称为颌下腺系数颌下腺指数,能反映腺体的变化情况,指数增大,提示腺体充血、水肿或增生肥大等;指数减小,表示腺体萎缩和其他退行性变产物。
文题释义:
放射性口干症:指接受放疗的头颈部肿瘤患者因其唾液腺受到照射后发生损伤,发生唾液性质和唾液量的改变,并引起口干、黏膜炎等一系列相关症状,远期反应严重者甚至出现吞咽和交谈困难、味觉丧失、龋齿发生及口腔真菌感染等。
颌下腺指数:又称为颌下腺系数颌下腺指数,能反映腺体的变化情况,指数增大,提示腺体充血、水肿或增生肥大等;指数减小,表示腺体萎缩和其他退行性变产物。