中国组织工程研究 ›› 2016, Vol. 20 ›› Issue (13): 1970-1976.doi: 10.3969/j.issn.2095-4344.2016.13.020
• 骨与关节循证医学 evidence-based medicine of the bone and joint • 上一篇
短节段与长节段固定融合修复退变性脊柱侧凸的Meta分析
陆海涛,袁 峰,杨宇明,张峻玮,李智多,盛晓磊
- 徐州医学院附属医院骨科,江苏省徐州市 221000
A meta-analysis of short fusion versus long fusion for degenerative scoliosis
Lu Hai-tao, Yuan Feng, Yang Yu-ming, Zhang Jun-wei, Li Zhi-duo, Sheng Xiao-lei
- Department of Orthopedics, Affiliated Hospital of Xuzhou Medical College, Xuzhou 221000, Jiangsu Province, China
摘要:
文章快速阅读:
.jpg) 文题释义:
文题释义:
短节段固定融合:脊柱融合节段仅限于畸形和下端椎,不超过上端椎,这种固定方式可以恢复局部的前凸和稳定性,但对矫正侧凸、侧方滑移、旋转半脱位、脊柱失衡的作用不如长节段手术,但是术后常有残留畸形,加速相邻节段退变加速和畸形进展的可能。
长节段固定融合:为了减少脊柱短节段固定融合的相关缺点,有学者尝试进行长节段固定融合,融合节段除了畸形,还要超过上下端椎,长节段矫形手术难度大,存在创伤大、出血多等并发症。
背景:目前退变性脊柱侧凸治疗的主要目的是解除患者症状,手术矫正侧凸畸形恢复脊柱的平衡及功能,但目前修复方式的选择存在一定的争议。
目的:系统评价短节段与长节段固定融合修复退变性脊柱侧凸的效果及安全性。
方法:通过CNKI、CBM、VIP、万方数据库等中文数据库,Pubmed、EMbase、Cochrane library等外文数据库,收集2015年5月前国内外已公开发表的关于短节段与长节段固定融合修复退变性脊柱侧凸的试验。采用RevMan 5.3.4软件对纳入文献进行统计分析。
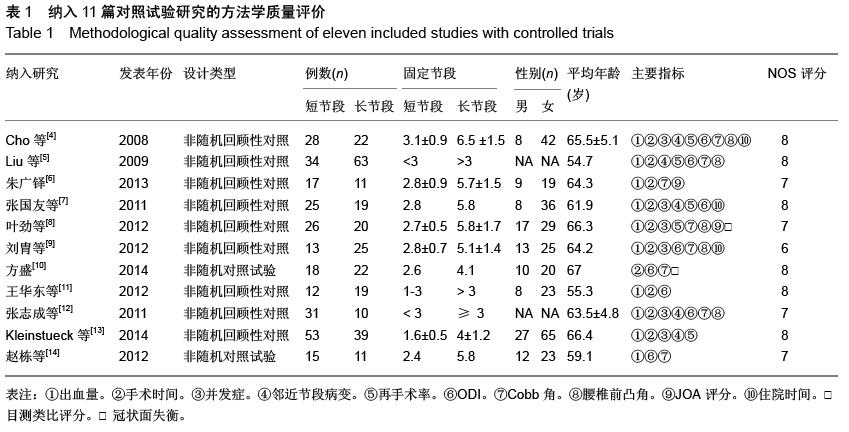
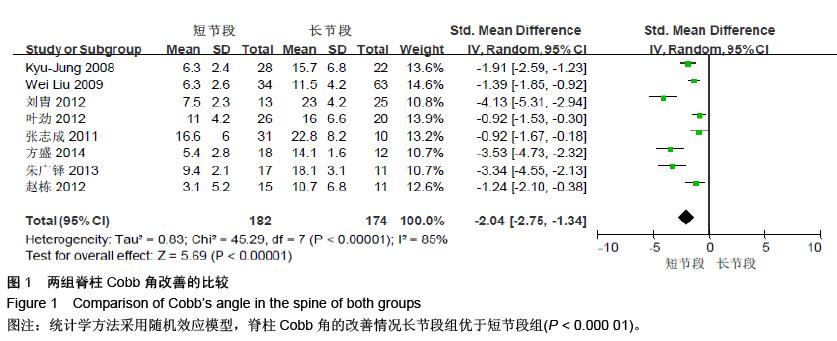
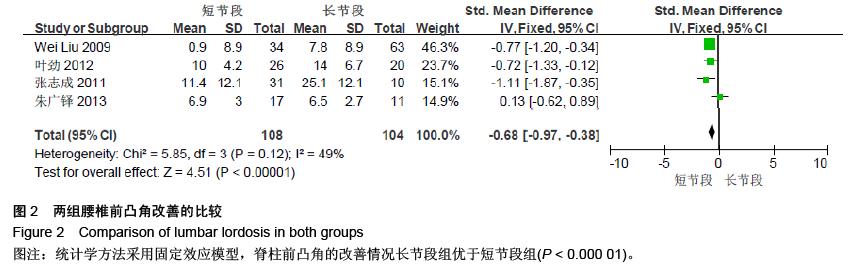
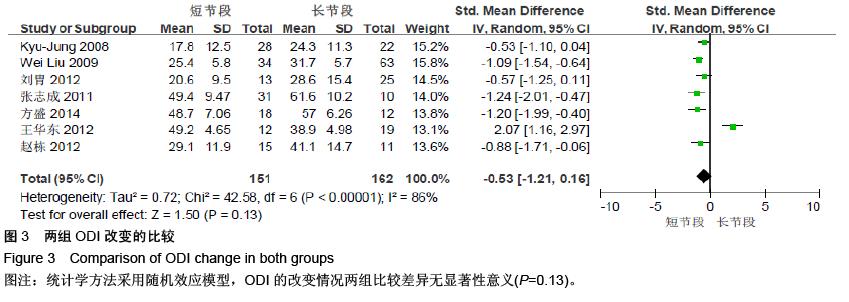
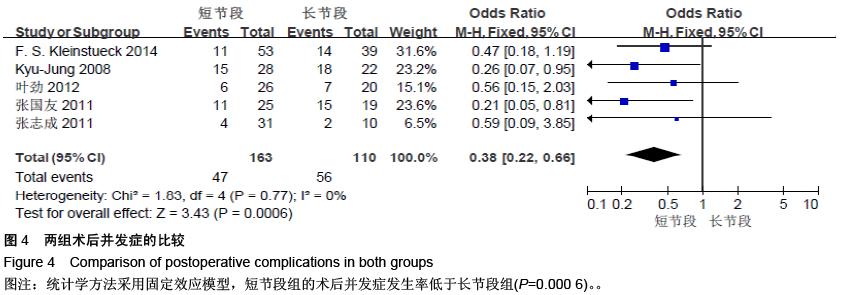
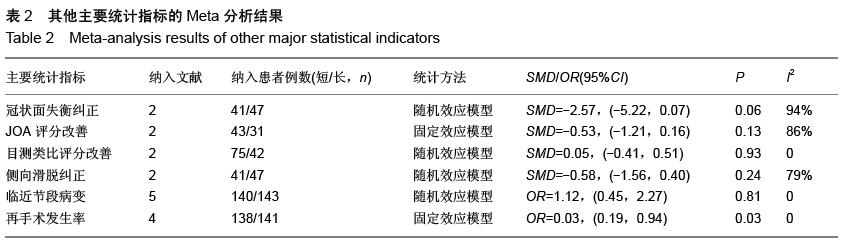
结果与结论:共计纳入11篇文献,共533例患者。其中短节段组272例,长节段261例。Meta分析结果显示:两种固定方法相比,脊柱Cobb角的改善(P < 0.000 01)、脊柱前凸角的改善(P < 0.000 01)方面,长节段组的疗效明显优于短节段组。冠状面失衡的矫正(P=0.06)、侧向滑脱矫正(P=0.24)方面两组差异无显著性意义。在日本骨科协会评分(P=0.93)、目测类比评分(P=0.22)以及Oswestry功能障碍指数(P=0.13)的改善方面,两组差异无显著性意义。在术后并发症(P=0.0006)以及术后再手术率方面(P=0.03),长节段组高于短节段组,两组在临近节段病变的发生率上差异无显著性意义(P=0.81)。提示长节段固定融合在纠正脊柱畸形方面优于短节段固定融合,但修复后并发症及再手术率高于短节段固定融合,在选择固定融合方案时应综合考虑。
ORCID: 0000-0002-2019-1380 (陆海涛)