| [1]赵御森,王海波,孟宪勇,等.组织工程骨修复超临界骨缺损研究进展[J].河北北方学院学报,2013,29(1):95.[2]Fishero BA,Kohli N,Das A,et al.Current concepts of bone tissue engineering for craniofacial bone defect repair.Craniomaxillofac Trauma Reconstr.2015;8(1):23-30.[3]Jeong SY, Hong JU, Song JM,et al. Combined effect of recombinant human bone morphogenetic protein-2 and low level laser irradiation on bisphosphonate-treated osteoblasts.J Korean Assoc Oral Maxillofac Surg.2018;44:259-268.[4]Bhujbal R,A Malik N,Kumar N,et al. Comparative evaluation of platelet rich plasma in socket healing and bone regeneration after surgical removal of impacted mandibular third molars. J Dent Res Dent Clin Dent Prospects.2018;12(3):153-158.[5]Cheng ZA,Alba-Perez A,Gonzalez-Garcia C,et al.Nanoscale Coatings for Ultralow Dose BMP-2-Driven Regeneration of Critical-Sized Bone Defects.Adv Sci.2019;6(2):1-12.[6]王腾飞,宋兴华,麦麦提艾力•阿不力克木,等.脂肪干细胞与羟基磷灰石/ β-磷酸三钙复合体修复兔椎体缺损[J].山东医药, 2018, 22(13):2081-2086.[7]Masquelet AC,Kishi T,Benko PE.Very long-term results of post-traumatic bone defect reconstruction by the induced membrane technique.Orthop Traumatol Surg Res. 2019; 105(1):159-166.[8]Masquelet AC.Induced membrane technique:pearls and pitfalls.J Orthop Trauma.2017;31 (Suppl 5):S36-S38.[9]Ronga M,Cherubino M,Corona K,et al.Induced membrane technique for the treatment of severe acute tibial bone loss: preliminary experience at medium-term follow-up.Int Orthop. 2019;43(1):209-215. [10]Akgun U,Canbek U,Aydogan NH,et al.Masquelet technique versus Ilizarov bone transport for reconstruction of lower extremity bone defects following posttraumatic osteomyelitis. Injury.2018; 49(3):738.[11]Christou C,Oliver RA,Yu Y,et al.The Masquelet technique for membrane induction and the healing of ovine critical sized segmental defects.PLoS One.2014;9(12): e114122.[12]McBride-Gagyi S,Toth Z,Kim D,et al.Altering spacer material affects bone regeneration in the Masquelet Technique in a Rat Femoral Defect.J Orthop Res.2018. doi: 10.1002/jor.23866. [Epub ahead of print][13]Gaio N,Martino A,Toth Z,et al.Masquelet technique: The effect of altering implant material and topography on membrane matrix composition, mechanical and barrier properties in a rat defect model. J Biomech.2018;72:53-62.[14]Aurégan JC,Bégué T,Rigoulot G,et al.Success rate and risk factors of failure of the induced membrane technique in children: a systematic review.Injury.2016;6(16):S62-S67.[15]Morelli I,Drago L,George DA,et al.Masquelet technique: myth or reality? A systematic review and meta-analysis. Injury. 2016; 47(6):S68-S76.[16]Ruehle MA,Krishnan L,Vantucci CE,et al.Effects of BMP-2 dose and delivery of microvascular fragments on healing of bone defects with concomitant volumetric muscle loss.J Orthop Res. 2019;37(3):553-561. [17]Kim S,Lee S,Kim K.Bone Tissue Engineering Strategies in Co-Delivery of Bone Morphogenetic Protein-2 and Biochemical Signaling Factors.Adv Exp Med Biol. 2018;1078:233-244.[18]Park J,Kim S,Kim K.Bone morphogenetic protein-2 associated multiple growth factor delivery for bone tissue regeneration.J Pharm Investig.2018;48(2):187-197.[19]Gonzaga MG,Dos Santos Kotake BG,Figueiredo FAT,et al. Effectiveness of rhBMP-2 association to autogenous, allogeneic, and heterologous bone grafts.Microsc Res Tech.2019.doi: 10.1002/jemt.23215. [Epub ahead of print].[20]Ishida W,Ramhmdani S,Xia Y,et al.Use of Recombinant Human Bone Morphogenetic Protein-2 at the C1-C2 Lateral Articulation without Posterior Structural Bone Graft in Posterior Atlantoaxial Fusion in Adult Patients.World Neurosurg. 2019;123:e69-e76.[21]Grey ZJ,Howie RN,Durham EL,et al.Sub-clinical dose of bone morphogenetic protein-2 does not precipitate rampant, sustained inflammatory response in bone wound healing. Wound Repair Regen. 2019. doi: 10.1111/wrr.12710.[Epub ahead of print].[22]Kizilda? A,Çiçek Y,Arabaci T,et al.The effect of leukocyte-platelet-rich fibrin on bone morphogenetic protein-2 and insulin-like growth factor-1 levels in patients with chronic periodontitis: a randomized split mouth clinical trail.Growth Factors.2019;9:239-245.[23]Hu J,Zeng Y,Shen C,et al.Mechanism of platelet-rich plasma in promoting bone defect repair. J Biol Regul Homeost Agents. 2019;33(1):97-103.[24]Yamada Y,Hara K,Nakamura S,et al. Minimally invasive approach with tissue engineering for severe alveolar bone atrophy case.Int J Oral Maxillofac Surg.2013;42:260-263.[25]Li H,Li B.PRP as a new approach to prevent infection: preparation and in vitro antimicrobial properties of PRP.J Vis Exp.2013;(74).doi: 10.3791/50351.[26]郭瑛,贾连顺,黄智.自体富血小板血浆在脊柱外科治疗中的应用[J].中国组织工程研究,2017,21(27):4403-4408.[27]Caplan AI,Sorrell JM.The MSC curtain that stops the immune system.Immunol Lett.2015;168:136-139.[28]Cheng A,Krishnan L,Pradhan P,et al.Impaired bone healing following treatment of established nonunion correlates with serum cytokine expression.J Orthop Res.2018;27:299-307.[29]唐勇,叶记超,胡旭民,等.基因重组人骨形态发生蛋白-2联合自体骨椎间打压植骨在腰椎融合术中的应用研究[J].中华骨与关节外科杂志,2018,9(11):664-667.[30]Cheng A,Krishnan L,Tran L,et al.The Effects of Age and Dose on Gene Expression and Segmental Bone Defect Repair Following BMP-2 Delivery.JBMR Plus.2019;3(2): e10068. |
.jpg)
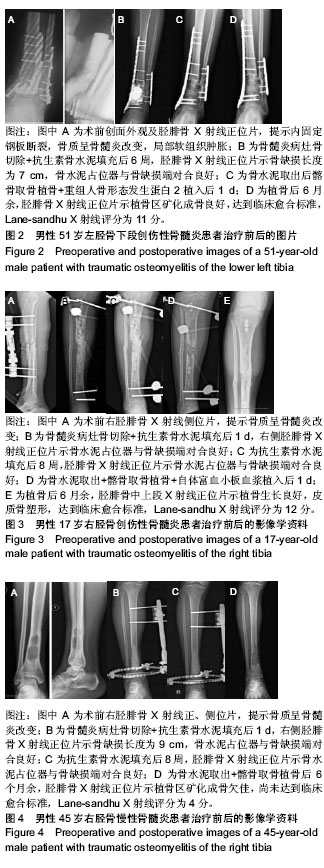
.jpg)
.jpg)