[1] 张庆富, 武京国, 张敏,等.经皮椎体后凸成形术后邻近椎体再骨折的病理机制研究[J]. 山东第一医科大学(山东省医学科学院)学报,2021,42(11):811-815.
[2] KLAZEN CAH, LOHLE PNM, DE VRIES J, et al. Vertebroplasty versus conservative treatment in acute osteoporotic vertebral compression fractures (Vertos II): an open-label randomised trial. Lancet. 2010;376(9746):1085-1092.
[3] 中华医学会骨质疏松和骨矿盐疾病分会, 章振林.原发性骨质疏松症诊疗指南(2022)[J]. 中国全科医学,2023,26(14):1671-1691.
[4] ZHANG C, TAN Z. The relationships between population factors and China’s carbon emissions: Does population aging matter? Renew Sustain Energy Rev. 2016;65:1018-1025.
[5] SUN H, LI C. Comparison of unilateral and bilateral percutaneous vertebroplasty for osteoporotic vertebral compression fractures: a systematic review and meta-analysis. J Orthop Surg Res. 2016;11(1):156.
[6] JOHNELL O, KANIS JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006;17(12):1726-1733.
[7] PRATHER H, HUNT D, WATSON JO, et al. Conservative Care for Patients with Osteoporotic Vertebral Compression Fractures. Phys Med Rehabil Clin N Am. 2007;18(3):577-591, xi.
[8] BUCHBINDER R, JOHNSTON R V, RISCHIN K J, et al. Percutaneous vertebroplasty for osteoporotic vertebral compression fracture. Cochrane Database Syst Rev. 2018;4(4): CD006349.
[9] TSOUMAKIDOU G, TOO CW, KOCH G, et al. CIRSE Guidelines on Percutaneous Vertebral Augmentation. Cardiovasc Intervent Radiol. 2017;40(3):331-342.
[10] ZHU S, SU Q, ZHANG Y, et al. Risk factors of cemented vertebral refracture after percutaneous vertebral augmentation: a systematic review and meta-analysis. Neuroradiology. 2020;62(11):1353-1360.
[11] JACOBSON RE, PALEA O, GRANVILLE M. Progression of Vertebral Compression Fractures After Previous Vertebral Augmentation: Technical Reasons for Recurrent Fractures in a Previously Treated Vertebra. Cureus.2017;9(10):e1776.
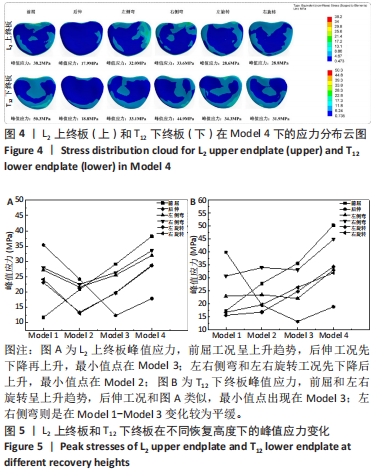
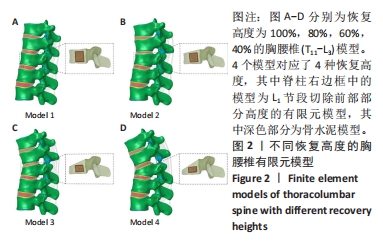
[12] 陈国能, 陈扬, 陈显辉, 等. PKP术后伤椎恢复高度与邻近椎体应力关系的有限元分析 [J]. 中国骨与关节损伤杂志,2019,34(11):1165-1167.
[13] 冯杰荣, 殷海东, 陈伟, 等.T12椎体前缘不同压缩状态下相邻椎体终板应力的有限元分析[J]. 中国组织工程研究,2016,20(22):3263-3271.
[14] 赵文韬, 秦大平, 张晓刚, 等.骨质疏松性椎体压缩骨折椎体强化术后不同椎体高度对相邻椎体应力影响的有限元分析[J]. 中国骨质疏松杂志,2018,24(9):1141-1147.
[15] 钱伟, 陈谷才. 骨质疏松性骨折PVP/PKP术后新发骨折的相关因素分析[J]. 世界最新医学信息文摘,2018,18(94):23-24+26.
[16] LI YA, LIN CL, CHANG MC, et al. Subsequent Vertebral Fracture After Vertebroplasty. Spine. 2012;37(3):179-283.
[17] YANG S, LIU Y, YANG H, et al. Risk factors and correlation of secondary adjacent vertebral compression fracture in percutaneous kyphoplasty. Int J Surg. 2016;36:138-142.
[18] AYTURK UM, GARCIA JJ, PUTTLITZ CM. The Micromechanical Role of the Annulus Fibrosus Components Under Physiological Loading of the Lumbar Spine. J Biomech Eng. 2010;132(6):061007.
[19] TAN QC, LIU ZX, ZHAO Y, et al. Biomechanical comparison of four types of instrumentation constructs for revision surgery in lumbar adjacent segment disease: A finite element study. Comp Bio Med. 2021;134:104477.
[20] ZHAO G, WANG H, WANG L, et al. The Biomechanical Effects of Different Bag‐Carrying Styles on Lumbar Spine and Paraspinal Muscles: A Combined Musculoskeletal and Finite Element Study. Orthop Surg. 2022;15(1):315-327.
[21] 蔡康健, 王丽珍, 姚杰, 等.腰椎椎体有限元建模的最优单元尺寸和材料属性分布及建模方法[J]. 医用生物力学,2016,31(2):135-141.
[22] WANG H, WAN Y, LIU X, et al. The biomechanical effects of Ti versus PEEK used in the PLIF surgery on lumbar spine: a finite element analysis. Comput Methods Biomech Biomed Engin. 2021;24(10):1115-1124.
[23] ZHANG NZ, XIONG QS, YAO J, et al. Biomechanical changes at the adjacent segments induced by a lordotic porous interbody fusion cage. Comput Biol Med. 2022;143:105320.
[24] KANG KT, KOH YG, SON J, et al. Biomechanical evaluation of pedicle screw fixation system in spinal adjacent levels using polyetheretherketone, carbon-fiber-reinforced polyetheretherketone, and traditional titanium as rod materials. Compos B Eng. 2017; 130:248-256.
[25] KIM HJ, KANG KT, CHUN HJ, et al. The influence of intrinsic disc degeneration of the adjacent segments on its stress distribution after one-level lumbar fusion. Eur Spine J. 2014;24(4):827-837.
[26] POLIKEIT A, NOLTE LP, FERGUSON SJ. The Effect of Cement Augmentation on the Load Transfer in an Osteoporotic Functional Spinal Unit: Finite-Element Analysis. Spine (Phila Pa 1976). 2003;28(10):991-996.
[27] 李家琼, 王冬梅, 孙璟川, 等.骨水泥对椎体成形术治疗胸腰椎骨质疏松压缩性骨折的生物力学影响[J]. 医用生物力学,2018,33(1):6-12.
[28] YAMAN O, DALBAYRAK S. Kyphosis and review of the literature. Turk Neurosurg. 2014; 24(4):455-465.
[29] EL-RICH M, ARNOUX PJ, WAGNAC E, et al. Finite element investigation of the loading rate effect on the spinal load-sharing changes under impact conditions. J Biomech. 2009;42(9):1252-1262.
[30] ZHOU R, HUANG Z, LIU X, et al. Kinematics and load-sharing of an anterior thoracolumbar spinal reconstruction construct with PEEK rods: An in vitro biomechanical study. Clin Biomech. 2016;40:1-7.
[31] LIN WC, CHENG TT, LEE YC, et al. New Vertebral Osteoporotic Compression Fractures after Percutaneous Vertebroplasty: Retrospective Analysis of Risk Factors. J Vasc Int Radiol. 2008;19(2):225-231.
[32] 蒋继乐,肖斌,张贵林,等. 骨水泥强化预防经皮穿刺球囊扩张椎体后凸成形术后高危患者上位节段再骨折的疗效[J]. 中国临床医学,2021,28(3):444-448.
[33] LIN EP, EKHOLM S, HIWATASHI A, et al. Vertebroplasty: cement leakage into the disc increases the risk of new fracture of adjacent vertebral body. AJNR Am J Neuroradiol. 2004;25(2):175-180.
[34] 邢润麟,张顺聪,江晓兵,等.脊柱矢状面失衡对骨质疏松性椎体压缩性骨折椎体成形术疗效的影响[J]. 脊柱外科杂志,2017,15(2):106-110.
[35] MCKIERNAN F, JENSEN R, FACISZEWSKI T. The Dynamic Mobility of Vertebral Compression Fractures. J Bone Miner Res. 2003;18(1):24-29.
[36] 江晓兵, 莫凌, 梁德, 等.骨水泥在椎体骨折线内弥散情况对椎体成形术治疗效果的影响[J]. 中国脊柱脊髓杂志,2014,24(2):144-149.
[37] LIN WC, CHENG TT, LEE YC, et al. New vertebral osteoporotic compression fractures after percutaneous vertebroplasty: Retrospective analysis of risk factors. J Vasc Interv Radiol. 2008;19(2 Pt 1):225-231.
[38] KIM SH, KANG HS, CHOI JA, et al. Risk Factors of New Compression Fractures in Adjacent Vertebrae after Percutaneous Vertebroplasty. Acta Radiologica. 2004;45(4):440-445.
[39] CHEN Z, SONG C, CHEN M, et al. What are risk factors for subsequent fracture after vertebral augmentation in patients with thoracolumbar osteoporotic vertebral fractures. BMC Musculoskelet Disord. 2021;22(1):1040.
|