中国组织工程研究 ›› 2020, Vol. 24 ›› Issue (18): 2848-2854.doi: 10.3969/j.issn.2095-4344.2631
• 人工假体 artificial prosthesis • 上一篇 下一篇
仰卧位直接前入路与后外侧入路全髋关节置换的比较
李永旺1,何荣丽2,张 谦1,安 明1,祁 辉1,马文海1,宋兴建1,孙俊英3
- 1保定市第一中心医院骨三科,河北省保定市 071000;2保定市第二医院消化内科,河北省保定市 071000;3苏州大学附属第一医院骨科,江苏省苏州市 215006
Comparison of direct anterior approach and posterolateral approach in supine position for total hip arthroplasty
Li Yongwang1, He Rongli2, Zhang Qian1, An Ming1, Qi Hui1, Ma Wenhai1, Song Xingjian1, Sun Junying3
- 1Third Department of Orthopedics, Baoding Municipal First Center Hospital, Baoding 071000, Hebei Province, China; 2Department of Gastroenterology, Baoding Municipal Second Hospital, Baoding 071000, Hebei Province, China; 3Department of Orthopedics, First Affiliated Hospital of Soochow University, Suzhou 215006, Jiangsu Province, China
摘要:

文题释义:
直接前入路:改良于Smith-Peterson入路及Heuter前入路,其实是一种改良的单切口Smith-Peterson入路,利用阔筋膜张肌、股直肌及缝匠肌之间的肌间隙直达髋关节,是一种真正从肌间隙进入的微创入路, 有着较好的肌肉保护、不易损伤运动神经、术后脱位率低、 康复快等先天优势。但采用直接前入路行全髋关节置换有较长的学习曲线,与传统入路相比存在术后髋关节脱位、假体松动、神经损伤等发生风险。
加速康复外科:是指采用有询证医学证据的围术期处理一系列优化措施,减少手术患者的生理及心理创伤应激,达到快速康复目的。其核心内容包括:①围术期多模式镇痛;②术后早期下床活动;③术后早期进食水;④避免或减少使用引流管等;⑤控制性输液,避免过多或过少的液体输注。其成效主要体现在:显著提高治疗效果;减少术后并发症;加速患者安全康复;显著缩短住院时间;降低整体医疗费用;减轻社会及家庭负担。
背景:后外侧入路是全髋关节置换的最常用手术入路。近年来直接前入路全髋关节置换的临床应用越来越多,并获得了良好的手术效果。
目的:比较仰卧位直接前入路与后外侧入路全髋关节置换的临床疗效。
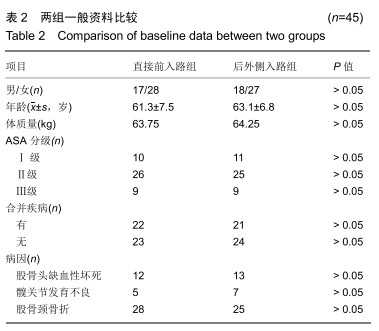
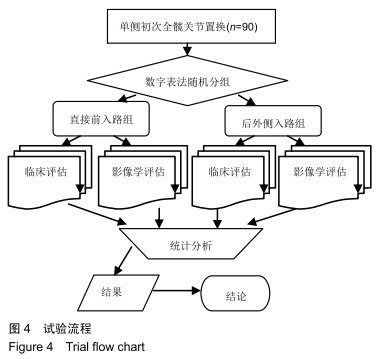
方法:纳入2015年4月至2019年4月保定市第一中心医院拟行单侧初次全髋关节置换的患者90例,其中男35例,女55例,年龄35-70岁,利用随机数字表法分为直接前入路组(n=45)和后外侧入路组(n=45)。术后随访评估髋关节Harris评分、目测类比评分、假体初始固定质量、髋臼杯安全范围。试验干预及治疗方案获保定市第一中心医院伦理委员会批准。
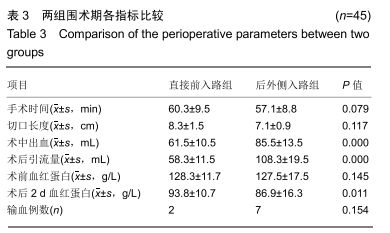
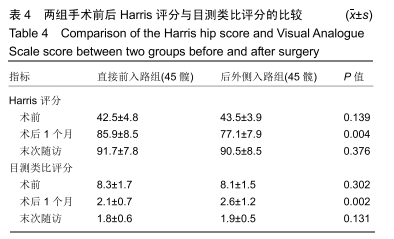
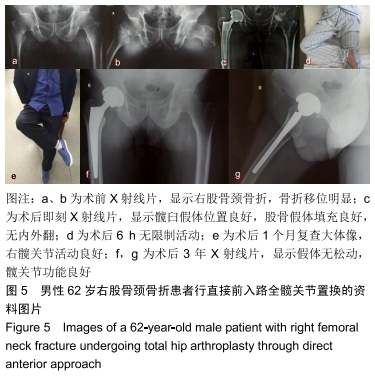
结果与结论:①90例患者均获得术后随访,随访时间3-51个月,平均14个月;直接前入路组发生2例术中股骨大转子骨折、1例股外侧皮神经损伤、4例股神经损伤、20例阔筋膜张肌损伤,后外侧入路组未发生上述并发症;②直接前入路组术后1个月的髋关节Harris评分、目测类比评分均优于后外侧入路组(P < 0.05),末次随访时两组间髋关节Harris评分、目测类比评分比较差异均无显著性意义(P > 0.05);③直接前入路组44髋股骨假体位于中立位,1髋处于内翻位,全部假体初始固定质量优;后外侧入路组43髋股骨假体位于中立位,2髋处于内翻位,全部假体初始固定质量优,两组间比较差异无显著性意义(P > 0.05);④直接前入路组髋臼杯位于Lewinnek安全范围的比率高于后外侧入路组(100%,82%,P < 0.05);⑤结果表明与后外侧入路相比,仰卧位直接前入路全髋关节置换能显著减轻术后疼痛、促进术后早期快速康复,获得更精准的髋臼假体角度,更有利于获得双下肢等长,是一种安全可靠的手术入路;但该技术操作有一定的技术难度,需要经历学习曲线,同时存在一些不同于其他入路的并发症。
ORCID: 0000-0002-6796-6438(李永旺)
中国组织工程研究杂志出版内容重点:人工关节;骨植入物;脊柱;骨折;内固定;数字化骨科;组织工程
中图分类号: