中国组织工程研究 ›› 2024, Vol. 28 ›› Issue (12): 1937-1943.doi: 10.12307/2024.018
• 骨与关节综述 bone and joint review • 上一篇 下一篇
髋膝关节置换后假体周围感染的治疗
曾子俊1,何 伟2,魏秋实2,何敏聪2
- 1广州中医药大学第三临床医学院,广东省广州市 510405;2广州中医药大学第三附属医院,广东省广州市 510378
-
收稿日期:2022-12-23接受日期:2023-03-02出版日期:2024-04-28发布日期:2023-08-23 -
通讯作者:何伟,博士,主任医师,广州中医药大学第三附属医院,广东省广州市 510378 -
作者简介:曾子俊,男,1998年生,广东省佛山市人,汉族,广州中医药大学在读硕士,主要从事髋膝关节疾病中医药治疗方面的研究。 -
基金资助:国家自然科学基金面上项目(82274544),项目负责人:魏秋实
Treatment of periprosthetic joint infection after hip and knee arthroplasty
Zeng Zijun1, He Wei2, Wei Qiushi2, He Mincong2
- 1Third Clinical Medical College of Guangzhou University of Chinese Medicine, Guangzhou 510405, Guangdong Province, China; 2Third Affiliated Hospital of Guangzhou University of Chinese Medicine, Guangzhou 510378, Guangdong Province, China
-
Received:2022-12-23Accepted:2023-03-02Online:2024-04-28Published:2023-08-23 -
Contact:He Wei, MD, Chief physician, Third Affiliated Hospital of Guangzhou University of Chinese Medicine, Guangzhou 510378, Guangdong Province, China -
About author:Zeng Zijun, Master candidate, Third Clinical Medical College of Guangzhou University of Chinese Medicine, Guangzhou 510405, Guangdong Province, China -
Supported by:National Natural Science Foundation (General Program) of China, No. 82274544 (to WQS)
摘要:
文题释义:
关节置换:采用人工关节替代无法继续使用的关节的一种手术治疗手段。目前,关节置换术是关节疾病终末期最常用的一种治疗手段。假体周围感染:在人工植入物邻近组织发生的一种感染性疾病,此文特指髋、膝关节置换术后假体周围感染,主要表现为人工关节周围的红肿、疼痛、皮温升高、关节活动功能障碍以及关节周围骨质溶解、破坏,形成窦道,少部分可伴有全身性感染症状。
背景:假体周围感染是关节置换后医生及患者最不愿意遇到的并发症之一,其顽固性和难治性一直是让关节科医生头痛的难题。
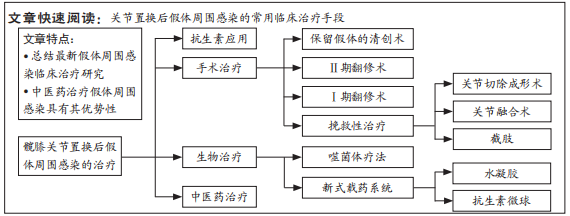
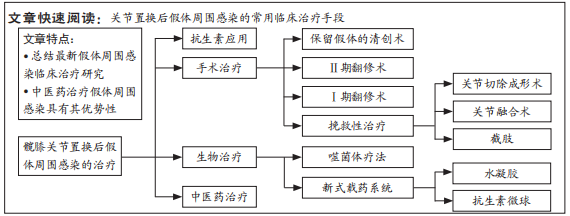
目的:综述国内外近年临床最新治疗髋、膝关节置换后假体周围感染的常用临床治疗手段,包括抗生素治疗、手术治疗、生物治疗、中医药治疗等,以期促进国内治疗假体周围感染的研究进展。方法:第一作者检索中国知网(CNKI)、万方、维普、PubMed等数据库2000年1月至2022年10月的文献,通过阅读题目初筛获得762篇文献,然后通过阅读摘要,排除内容重复、数据可靠性低、观点过时的文献后获得194篇文献,再通过精读原文最终纳入88篇文献。
结果与结论:①治疗假体周围感染过程中,组合型抗生素给药方案或有助于根除感染;②Ⅱ期翻修术仍是治疗假体周围感染的金指标;③Ⅰ期翻修术缺乏大样本的临床研究,需要更多的临床观察;④生物治疗中的噬菌体疗法、新式载药系统已少量应用于临床,在假体周围感染的预防和根除上表现出其优势特点;⑤中医药配合抗生素、手术治疗手段能提高预防、治疗假体周围感染的效果,但缺乏高等级的循证医学证据。
https://orcid.org/0000-0002-9887-9003 (曾子俊)
中国组织工程研究杂志出版内容重点:人工关节;骨植入物;脊柱;骨折;内固定;数字化骨科;组织工程
中图分类号:
引用本文
曾子俊, 何 伟, 魏秋实, 何敏聪. 髋膝关节置换后假体周围感染的治疗[J]. 中国组织工程研究, 2024, 28(12): 1937-1943.
Zeng Zijun, He Wei, Wei Qiushi, He Mincong. Treatment of periprosthetic joint infection after hip and knee arthroplasty[J]. Chinese Journal of Tissue Engineering Research, 2024, 28(12): 1937-1943.
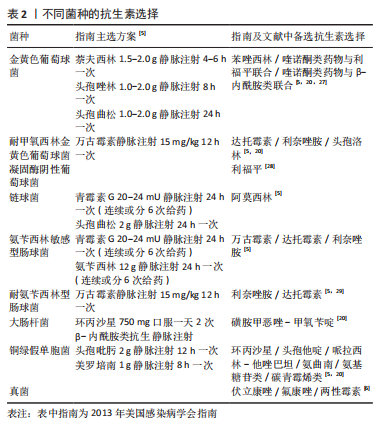
PJI感染菌种大部分为革兰阳性菌,所占比率可高达80%,其中最常见菌种为金黄色葡萄球菌与耐甲氧西林金黄色葡萄球菌,其次为凝固酶阴性葡萄球菌、链球菌以及肠球菌等,小部分为革兰阴性菌,约占13%[10],包括大肠埃希菌、铜绿假单胞菌等,其次为相对罕见的真菌等其他[11]。近年来,以耐药菌为特点的难治性PJI发生数量逐渐上涨,如耐甲氧西林金黄色葡萄球菌感染型的PJI[12-14]。对于链球菌,有研究显示实施DAIR后仍长期(6个月以上)运用抗生素抑制感染可达到更好的疗效[15]。肠球菌可分为氨苄西林敏感型和耐氨苄西林型,其造成的感染较难治愈,宜尽早进行清创或Ⅱ期翻修[16],术后配合抗生素治疗。现阶段,革兰阴性菌感染的PJI比革兰阳性菌的治疗效果差,其手术失败(革兰阴性菌失败率67.9%,革兰阳性菌失败率33.2%),再次感染概率较高[17-18]。对于铜绿假单胞菌既往常采用环丙沙星等喹诺酮类药物,有研究显示环丙沙星近年来耐药率已达20%[19],因此,若出现喹诺酮类耐药菌可换用第4代头孢菌素、哌拉西林-他唑巴坦、氨曲南、氨基糖苷类或碳青霉烯类进行治疗[20]。真菌在PJI感染中的检出率较低,美国的检出率约为2.3%[21]。
仅对革兰阳性菌及革兰阴性菌的耐药试验研究发现,这两类菌对β-内酰胺类和喹诺酮类药物的耐药性超过16%,所以,为了应对高出现率的耐药菌,国外有诸多动物研究采用2种及2种以上的抗生素,结果治疗效果优于仅使用一种抗生素[22-25];临床方面AUNON等[26]对DAIR治疗后患者采用5日静脉给药达托霉素+氯唑西林,然后换予左氧氟沙星-利福平,发现优于传统方案(万古霉素+利福平或左氧氟沙星+利福平)。不同菌种用药可见表2。
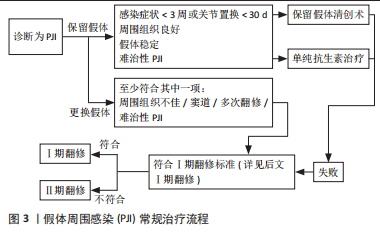
2.2 手术相关 根据国际共识,PJI发生后宜尽早采取手术治疗,手术手段通常包括有保留假体的清创治疗、Ⅰ期翻修术和Ⅱ期翻修术。
2.2.1 DAIR 当感染处于早期或持续时间较短时,DAIR具有对患者经济压力负担低、手术创伤小、术后恢复时间短等优点[30],仅适用于早期感染(感染症状< 3周或关节置换< 30 d)且周围组织良好、假体稳定、非难治性PJI。与PJI治疗金标准的Ⅱ期翻修术相比,单次或2次的DAIR感染根除率达到85%,与Ⅱ期翻修后的89%近似[31]。但是,DAIR失败后的高昂代价也不容忽视,对于有金黄色葡萄球菌感染的患者或血沉 > 107.5 mm/h 的患者,DAIR的治疗手段应慎重考虑,Ⅰ、Ⅱ期翻修术应作为首选治疗手段,以最大限度地提高手术成功率[32]。根据现有指南及部分研究共识[7],符合初次置换后浅表感染、2个月内的早期深部感染或急性血源性感染,且无窦道等高危因素时,可以考虑DAIR治疗[33]。但一份107例病例的研究显示,窦道并不会影响DAIR的成功率,且对于存在窦道的患者来说,更换模块组件的DAIR治疗的手术成功率为75.8%[34]。在术后经验性运用抗生素能提高感染的根除率,可服用万古霉素或替考拉宁,并运用第3代头孢如头孢曲松等[35-36],直到细菌培养结果出来后再进行针对性用药。
2.2.2 Ⅱ期翻修术 Ⅱ期翻修术以其较高的手术成功率和感染根除率,在美国一直被视为PJI治疗手段的金标准[37],其治疗流程是在第一阶段手术中取出所有可更换的部件,再进行彻底的清创,置入载有抗生素的间隔器,留取假体周围组织标本做病理学检查,根据检查结果选择Ⅱ期假体置入手术的时机,手术间隔期和Ⅱ期手术后都要采用抗生素预防或治疗感染。间隔器载入的抗生素可以选择的搭配应具有广谱抗菌的能力,如万古霉素和头孢他啶或妥布霉素或林可霉素等[38-39]。许多医生将Ⅱ期翻修作为面对慢性PJI[40]、耐甲氧西林葡萄球菌感染或真菌感染时的首选治疗手段[41]。而对于造成Ⅱ期翻修失败的危险因素,有研究显示耐药菌、胫骨缺损程度、手术次数都是影响手术成功与否的重要因素[42-43]。近年来,随着对可降解骨水泥、硫酸钙等新式间隔器的深入开发与应用,也使Ⅱ期翻修术更加成熟,手术成功率更高。
2.2.3 Ⅰ期翻修术 相较于Ⅱ期翻修术,Ⅰ期翻修仅在一次手术中便完成了更换关节假体、彻底清创,术后抗生素治疗,其具有手术次数少,经济成本低、患者接受度高等优点,且当存在PJI的情况下,Ⅰ、Ⅱ期翻修的存活率近似[44]。2018年费城假体周围感染国际共识会议中指出Ⅰ期翻修术的适应证:①骨质和软组织缺损度低;②病原菌已知、单一且药敏感性明确;③全身状况良好,免疫无缺陷,无脓毒血症。禁忌证为:①骨质或软组织严重缺损;②无法彻底清创和局部使用抗生素;③假体周围存在窦道;④PJI培养阴性。对于Ⅰ期翻修术来说,手术的成功不仅取决于所有硬件(包括骨水泥和限制器)的移除,还取决于对受感染周围骨组织、软组织的彻底清创,其次术中抗生素的应用与术后全身性抗生素应用也都对手术成功、感染根除起到重要作用。尽管现有指南认为Ⅰ期翻修仅应用于单一感染型的PJI患者,但LI等[45]对多种感染型PJI患者采用Ⅰ期翻修联合术后关节腔内输注合适的抗生素可有效提高感染根除率。中长期(1年以上)手术成功率方面,CASTELLANI等[46]对一组平均随访29.2个月的菌培养阴性的PJI病例进行了回顾,Ⅰ期翻修组(7/7)的成功率为100%,Ⅱ期翻修组(26/27)的成功率为96.3%,两者成功率接近;但其短期(1年内)的Ⅰ期翻修(33/35)成功率为94.2%,Ⅱ期翻修(63/75)成功率为84%。鉴于Ⅰ期翻修相较于Ⅱ期翻修具有疗程短、经济成本低、患者接受度高的优势,优化Ⅰ期翻修方案,扩大Ⅰ期翻修治疗范围或许是未来PJI治疗的重要方向。现有的Ⅰ期翻修术相关研究存在一定的回顾性偏倚,需更多高样本、高价值的临床随机对照试验。
2.2.4 挽救性治疗 尽管现有治疗PJI的手段已经非常成熟,但是当遇到一些危险因素时,如血液透析、肥胖、多次既往手术史、糖尿病、皮质类固醇治疗、低白蛋白血症、免疫抑制、风湿病、凝血障碍以及多重耐药菌或真菌引起的感染等因素,PJI的治疗仍可能以失败为结局[47],这时可以考虑挽救性的治疗措施,包括关节切除成形术、关节融合术和截肢等方式。
(1)关节切除成形术:关节切除成形术即取出关节假体不再置入,自1928年以来一直作为顽固性PJI的挽救性治疗措施。GOLDMAN等[48]对25例膝假体顽固性PJI患者采用了关节切除成形术治疗,平均随访4年后,尽管所有患者都需要支撑和辅助设备,21例患者未复发感染,感染根除率为84%。相较于截肢而言,关节切除成形术在较高的感染根除率的同时给予了患者一次重新置入假体的机会。
(2)关节融合术:关节融合术与关节切除成形术相似,是PJI发生后的补救治疗措施之一。其通过髓内钉内固定、钢板螺钉固定、支架外固定等方式固定关节,将关节面作骨性融合,以此达到根除感染的目的。YEUNG等[49]对51例因膝部PJIⅡ期翻修治疗失败的患者采用了膝关节融合术,随访2年后,48例(94.1%)患者感染得到根除,其中41例患者(85.4%)在关节融合术后仍可以行走,且有9例患者(18.8%)可不使用辅助设备自行行走。有学者认为,Ⅱ期翻修术后仍持续感染的全膝关节置换患者,应考虑采用关节融合术解决感染问题。
(3) 截肢:截肢作为PJI治疗的最终手段,临床医生应慎重考虑,截肢后会给患者带来更大的心理负担和社会生活压力[50]。TROUILLEZ等[51]在一项病例对照研究中,将20例膝关节截肢患者与23膝关节融合患者比较,随访4年以上后发现,截肢患者的感染复发率10%(2例)低于膝关节融合患者的感染复发率21.75%(5例)。
2.3 生物治疗 生物治疗是近年来随着耐药菌出现、抗生素“失灵”等原因而提出的新兴治疗PJI的手段。生物治疗是一项交叉学科的新型治疗技术,涉及化学、物理、生物工程等学科,治疗方式包括有噬菌体疗法、新式载药系统、生物膜裂解剂、免疫疗法、生物靶向疗法、光动力疗法及超声波治疗等手段,此文仅介绍已应用于临床的噬菌体疗法和新式载药系统。
2.3.1 噬菌体疗法 噬菌体疗法是利用了自然界中存在的噬菌体能产生不同的、可破坏细菌细胞壁的蛋白酶——内溶素这一特性来治疗细菌感染性疾病的治疗方法。最早由法国微生物学家费力克斯(Félix d’Hérelle ,1873-1949)在1917年提出并使用,这一疗法距今已有100多年的历史。
在预防PJI方面,可在关节置换术中,将噬菌体的液体或粉末作为传统抗生素的替代物在关节假体周围给药,以预防PJI的发生。可以使用药物缓释系统,如羟丙基甲基纤维素在假体周围潜在感染部位逐步释放、递送噬菌体,以预防细菌生物膜的建立和PJI的发生,不过噬菌体给药至关节假体周围的最佳部位及方式尚未明确[52],需要更多的体外实验以确定最佳使用方法。FERRY等[53]对3例全膝关节置换术后发生金黄色葡萄球菌感染的PJI患者,采用DAIR配合术中噬菌体疗法,经过半年以上的随访,2例患者长期持续排出滑液,再次进行新的DAIR,术中仅显示轻度滑膜炎症,未见细菌感染。面对难治的抗生素耐药菌菌株感染的PJI,噬菌体治疗也不失为一种新的有效替代疗法。在DOUB等[54]的病例报告中,1例72岁男性右膝因慢性耐甲氧西林金黄色葡萄球菌感染引起PJI,在进行DAIR无效后采用了菌种敏感型的噬菌体静脉注射治疗,感染得到根除。而后,同一位作者在另一例70岁女性右膝和右髋合并耐甲氧西林金黄色葡萄球菌感染的PJI中运用了噬菌体疗法,感染同样得到了根除[55]。噬菌体疗法尽管已存在很长时间,但其运用于PJI治疗的过程仍较短,相关病例报告也较少,其在临床中使用的最佳给药部位、方法等仍需要更高等级的试验以明确。
2.3.2 新式载药系统 术后假体周围的抗菌药给药系统与手术治疗一样重要,优良的假体周围载药系统可以增强抗生素抗菌效能,减少关节置换术后假体周围细菌生物膜定植率,降低PJI清创术、翻修术后感染的复发率。现已应用于临床的新式载药系统有水凝胶载药系统和抗菌微球载药系统。
(1) 水凝胶载药系统:是一种防御性抗菌涂层,由共价结合的透明质酸和聚乳酸组成,能够在假体周围释放高浓度的抗生素以形成阻挡细菌形成生物膜的屏障,随后在72 h内逐渐释放其内所含抗生素。DRAGO等[56]已在体外、体内实验证实水凝胶的安全性及有效抑制局部细菌生物膜的形成。DE MEO等[57] 在一项回顾性的病例对照研究中,实验组17例无菌性髋假体翻修术患者在术中使用了负载庆大霉素与万古霉素的水凝胶涂层,术后随访6个月,实验组未报告PJI,对照组17例患者报告了6例PJI,证实抗生素水凝胶涂层可有效降低具有高感染因素患者发生PJI的风险。PELLEGRINI等[58]对10例髋部PJI患者Ⅰ期翻修中,使用了非骨水泥型抗菌水凝胶涂层,平均随访3.1年,感染根除率达100%,影像学检查及HSS评分显示患者恢复良好。FRANCESCHINI等[59]在28例慢性髋部PJI患者Ⅱ期翻修术中将抗生素水凝胶涂层涂抹于髋臼和股骨组件表面,术后平均随访2年,2例在翻修术后3周内出现再感染,26例未见感染复发,治愈率达92.9%。也有研究显示,Ⅰ期翻修术中使用抗生素水凝胶涂层感染复发率与未使用的涂层的Ⅱ期翻修术相近[60]。FERR等[61]报告了1例49岁男性膝部金黄色葡萄球菌感染的PJI病例,采用DAIR清理假体周围感染组织,再将噬菌体与水凝胶混合覆盖于假体周围,术后患者出现心肌梗死导致游离瓣下形成血肿,继发感染后进行了截肢。水凝胶在翻修术后降低PJI的出现或复发已得到小样本的临床试验证实,但在DAIR治疗中其安全性和根除感染的有效性还需要更多研究证实。
(2) 抗生素微球载药系统:现已应用于临床的抗生素微球载药系统是抗生素骨水泥缓释系统的新型替代品,其大部分为可降解的新型材料,在30-60 d内吸收,如硫酸钙等,可以用于术中填充假体与周围组织空隙,其内可加入抗生素,发挥局部缓释的效果。MANDELL等[62]证实,假体周围局部抗生素给药后感染控制效果优于全身给药。GARCíA-GARCíA等[63]在体外实验中发现,将达托霉素和万古霉素混合加入乳酸-乙醇酸微球用于治疗金黄色葡萄球菌感染的兔PJI模型,可达到控制感染同时减轻骨组织结构损坏的效果。在面对碳青霉烯类耐药肠杆菌和万古霉素耐药菌多重耐药的PJI病原菌时,STOODLEY等[64]在体外实验中证实,将利福平联合美罗培南或利福平联合万古霉素加入硫酸钙珠后覆盖于多重耐药菌表面,可有效破坏细菌的生物膜。GHIRARDELLI等[65]认为在早期、急性的血源性PJI采用DAIR联合抗生素硫酸钙珠治疗感染,是较安全保守的治疗方法;但是也有学者在为期2年的队列研究中发现,抗生素硫酸钙珠配合DAIR治疗90 d内的早期PJI并没有降低PJI的复发率,同时增加了治疗成本[66]。
CHANG等[67]发现DAIR配合抗生素微球缓释系统与Ⅱ期翻修相比并不能显著提高关节功能结局和患者满意度。MOHAMED等[68]在96例临床对照试验中发现,实验组在Ⅰ期无菌翻修后假体周围加入抗生素硫酸钙珠,术后感染发生率并未在统计学上发现对照组与实验组的差异,抗生素硫酸钙珠在Ⅰ期翻修中的预防PJI效果值得怀疑。同时,在一项临床研究中发现,可吸收的硫酸钙珠有可能导致血液中钙的含量上升[69];但是也有荟萃分析认为,这种血清钙的上升是一过性的,症状性的高钙血症风险较低[70]。因此,抗生素微球载药系统尤其是硫酸钙型的微球载药系统需要更多的研究以证实其人体使用的安全性以及根除PJI的有效性。
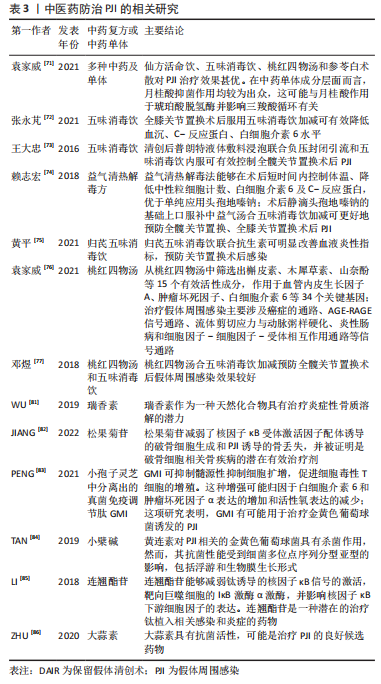
2.4 中医治疗 中医因其作用成分的复杂性,当其面对耐药问题时有着天然的优势。近年来,中医学在防治PJI上亦有建树,据文献报道,中医在临床采用复方汤药防治PJI,其搭配抗生素后的效果略优于单独使用抗生素治疗,且其具有副反应小和促进患者身体功能恢复的特点,这在PJI治疗上具有巨大潜力。
出自清代名医吴谦所著的《医宗金鉴》的五味消毒饮在临床上一直有应用于治疗PJI的相关报道,其原方组成为:金银花、野菊花、蒲公英、紫花地丁、紫背天葵子。现代研究认为五味消毒饮可能通过调节白细胞介素6、白细胞介素1β、肿瘤坏死因子、自然杀伤细胞、脂多糖等,以此来抑制细菌的生物膜形成,调控相关炎症反应[71]。
张永芃[72]在膝关节置换术后给予患者服用五味消毒饮,证实了五味消毒饮可在膝关节置换术后有效降低血沉、C-反应蛋白、白细胞介素6水平。王大忠等[73]在9例髋关节置换患者、3例膝关节置换患者发生PJI后,采取清创和普朗特液体敷料浸泡联合负压封闭引流和五味消毒饮加减内服的手段治疗感染,五味消毒饮组成为金银花、紫花地丁、野菊花、紫背天葵子、蒲公英;肿胀明显、皮温不高者,加茯苓、泽泻、薏苡仁等;肿胀明显、皮温高者,加鲜地黄、黄连、牡丹皮等;肿痛明显者,加穿山甲、红花、桃仁,每日1剂,早晚各1服,连续15 d;结果示:11例患者感染的得到控制。赖志宏等[74]将120例髋、膝关节置换术后患者分成2组,对照组术后单用头孢嗪钠预防感染,实验组予以中西医结合预防感染,西药采用头孢嗪钠,中医口服由五味消毒饮为基础的变方益气清热解毒汤剂:黄芪、党参、金银花、野菊花、蒲公英、紫花地丁、白术、紫背天葵子、甘草,早晚各1服,连续7 d,结果显示,益气清热解毒法协同头孢嗪钠在髋、膝关节置换术后控制患者体温、降低白细胞计数、白细胞介素6和C-反应蛋白水平的效果优于单用头孢嗪钠。黄平等[75]对200例关节置换患者进行研究,实验组口服五味消毒饮加黄芪、当归,并且联合使用抗生素,早晚各1次,连续5 d,结果显示:五味消毒饮加黄芪、当归联合抗生素可有效降低关节置换后白细胞计数、血沉及C-反应蛋白水平。
同样出自于《医宗金鉴》的桃红四物汤,其现代药理学研究表明其具有扩张血管、抗炎、调节免疫功能等作用,其中的活性成分槲皮素及其关键基因可能通过调控血管内皮生长因子A从而抑制破骨细胞活性,减轻PJI带来的骨溶解效应,达到治疗PJI的目的[76]。
邓煜等[77]将100例髋关节置换术后患者分2组,对照组采用头孢呋辛,治疗组加服五味消毒饮合桃红四物汤加减,组成为当归、红花、野菊花、陈皮、生甘草、茯苓、蒲公英、紫花地丁、桃仁、紫背天葵子、三棱、莪术、金银花、黄芪、炮穿山甲、夏枯草、酒川芎,每日1剂,分早中晚3次口服,以7 d为一疗程,共2个疗程,结果显示治疗组切口感染率、C-反应蛋白、血沉和白细胞水平优于对照组。
骨溶解在PJI发生后较常见,其通常给患者带来假体松动等预后不良的结果[78],骨溶解主要为细菌表面的破骨因子及炎症反应后引起的破骨细胞过度活跃所造成的[79]。研究显示桃红四五汤能抑制肿瘤坏死因子α、白细胞介素1、核因子κB受体激活因子配体(receptor activator of nuclear factor-κB ligand,RANKL)等促进破骨细胞成熟的上游因子[80];中药瑞香中提取的瑞香素能抑制小鼠模型的炎症性骨溶解,其机制可能为瑞香素影响了RANKL中的细胞外信号调节激酶、c-fos和NFATc1信号通路来抑制破骨细胞发挥作用[81]。而JIANG等[82]亦在大鼠模型中发现中药肉苁蓉的提取物松果菊苷能影响RANKL中的PI3K、Akt和c-fos通路,从而抑制破骨细胞功能。
此外,GMI是一种从中药灵芝中提取的免疫调节肽,有研究在小鼠模型实验中发现其可以抑制髓源性抑制细胞的扩增来促进T细胞的增殖,从而达到治疗金黄色葡萄球菌相关PJI的目的[83]。近年来,还发现了大蒜素、连翘苷和黄连素等中药提取物具有天然的抑制感染、破坏细菌生物膜、削弱炎症反应的作用[84-86]。
尽管已有大量报道证明了中医药防治PJI的有效性,见表3,但中医在这方面的临床研究仍停留于初步阶段,例如对个体病例的总结缺乏中医的病因病机及证候分型叙述;所选的病例无统一的选择指标;疗效无统一的指标,这些问题都有待解决。此外,中医药对抑制PJI发生后的骨溶解具有巨大潜力,但其研究大多仍停留于体外实验,缺乏临床循证依据,需要更多的前瞻性研究来发掘其实用性。
| [1] MA R, HU X, ZHANG X, et al. Strategies to prevent, curb and eliminate biofilm formation based on the characteristics of various periods in one biofilm life cycle. Front Cell Infect Microbiol. 2022;12:1003033. [2] HALL CW, MAH TF. Molecular mechanisms of biofilm-based antibiotic resistance and tolerance in pathogenic bacteria. FEMS Microbiol Rev. 2017;41(3):276-301. [3] PARVIZI J, GEHRKE T. Definition of periprosthetic joint infection. J Arthroplasty. 2014;29(7):1331. [4] PARVIZI J, TAN TL, GOSWAMI K, et al. The 2018 Definition of Periprosthetic Hip and Knee Infection: An Evidence-Based and Validated Criteria. J Arthroplasty. 2018;33(5):1309-1314. [5] OSMON DR, BERBARI EF, BERENDT AR, et al. Diagnosis and management of prosthetic joint infection: clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis. 2013;56(1):e1-e25. [6] 王相选, 方心俞, 李文波, 等. 假体周围感染全身性抗生素治疗的应用进展[J]. 中华骨与关节外科杂志,2019,12(5):389-395. [7] 中华医学会骨科学分会关节外科学组中国PJI诊断和治疗指南编写委员会. 中国人工关节感染诊断与治疗指南[J]. 中华外科杂志, 2021,59(6):430-442. [8] RAO N, CROSSETT LS, SINHA RK, et al. Long-term suppression of infection in total joint arthroplasty. Clin Orthop Relat Res. 2003;(414):55-60. [9] TOH RX, YEO ZN, LIOW M, et al. Debridement, Antibiotics, and Implant Retention in Periprosthetic Joint Infection: What Predicts Success or Failure? J Arthroplasty. 2021;36(10):3562-3569. [10] 闫开成, 王昆, 胡锦桃, 等. 关节置换术后假体周围感染病原菌分布特点及治疗[J]. 中国感染控制杂志,2022,21(6):546-553. [11] KAPADIA BH, BERG RA, DALEY JA, et al. Periprosthetic joint infection. Lancet. 2016;387(10016):386-394. [12] PULIDO L, GHANEM E, JOSHI A, et al. Periprosthetic joint infection: the incidence, timing, and predisposing factors. Clin Orthop Relat Res. 2008;466(7):1710-1715. [13] MORAN GJ, KRISHNADASAN A, GORWITZ RJ, et al. Methicillin-resistant S. aureus infections among patients in the emergency department. N Engl J Med. 2006;355(7):666-674. [14] BJERKE-KROLL BT, CHRIST AB, MCLAWHORN AS, et al. Periprosthetic joint infections treated with two-stage revision over 14 years: an evolving microbiology profile. J Arthroplasty. 2014;29(5):877-882. [15] RENZ N, RAKOW A, MULLER M, et al. Long-term antimicrobial suppression prevents treatment failure of streptococcal periprosthetic joint infection. J Infect. 2019;79(3):236-244. [16] RASOULI MR, TRIPATHI MS, KENYON R, et al. Low rate of infection control in enterococcal periprosthetic joint infections. Clin Orthop Relat Res. 2012;470(10):2708-2716. [17] KALBIAN IL, GOSWAMI K, TAN TL, et al. Treatment Outcomes and Attrition in Gram-Negative Periprosthetic Joint Infection. J Arthroplasty. 2020;35(3):849-854. [18] ZMISTOWSKI B, FEDORKA CJ, SHEEHAN E, et al. Prosthetic joint infection caused by gram-negative organisms. J Arthroplasty. 2011; 26(6 Suppl):104-108. [19] SHAH NB, OSMON DR, STECKELBERG JM, et al. Pseudomonas Prosthetic Joint Infections: A Review of 102 Episodes. J Bone Jt Infect. 2016;1:25-30. [20] MILLER R, HIGUERA CA, WU J, et al. Periprosthetic Joint Infection: A Review of Antibiotic Treatment. JBJS Rev. 2020;8(7):e1900224. [21] AGGARWAL VK, BAKHSHI H, ECKER NU, et al. Organism profile in periprosthetic joint infection: pathogens differ at two arthroplasty infection referral centers in Europe and in the United States. J Knee Surg. 2014;27(5):399-406. [22] THOMPSON JM, SAINI V, ASHBAUGH AG, et al. Oral-Only Linezolid-Rifampin Is Highly Effective Compared with Other Antibiotics for Periprosthetic Joint Infection: Study of a Mouse Model. J Bone Joint Surg Am. 2017;99(8):656-665. [23] KARAU MJ, SCHMIDT-MALAN SM, ALBANO M, et al. Novel Use of Rifabutin and Rifapentine to Treat Methicillin-Resistant Staphylococcus aureus in a Rat Model of Foreign Body Osteomyelitis. J Infect Dis. 2020; 222(9):1498-1504. [24] GREIMEL F, SCHEUERER C, GESSNER A, et al. Efficacy of antibiotic treatment of implant-associated Staphylococcus aureus infections with moxifloxacin, flucloxacillin, rifampin, and combination therapy: an animal study. Drug Des Devel Ther. 2017;11:1729-1736. [25] GOETZ J, KEYSSNER V, HANSES F, et al. Animal experimental investigation on the efficacy of antibiotic therapy with linezolid, vancomycin, cotrimoxazole, and rifampin in treatment of periprosthetic knee joint infections by MRSA. Bone Joint Res. 2022;11(3):143-151. [26] AUNON A, TOVAR-BAZAGA M, BLANCO-GARCIA A, et al. Does a New Antibiotic Scheme Improve the Outcome of Staphylococcus aureus-Caused Acute Prosthetic Joint Infections (PJI) Treated with Debridement, Antibiotics and Implant Retention (DAIR)? Antibiotics (Basel). 2022;11(7):922. [27] CORTES-PENFIELD NW, HEWLETT AL, KALIL AC. Adjunctive Rifampin Following Debridement and Implant Retention for Staphylococcal Prosthetic Joint Infection: Is it Effective if not Combined With a Fluoroquinolone? Open Forum Infect Dis. 2022;9(12):c582. [28] LORA-TAMAYO J, MURILLO O, IRIBARREN JA, et al. A large multicenter study of methicillin-susceptible and methicillin-resistant Staphylococcus aureus prosthetic joint infections managed with implant retention. Clin Infect Dis. 2013;56(2):182-194. [29] RENZ N, TREBSE R, AKGUN D, et al. Enterococcal periprosthetic joint infection: clinical and microbiological findings from an 8-year retrospective cohort study. BMC Infect Dis. 2019;19(1):1083. [30] 程永刚, 周胜虎, 刘军, 等. 人工髋膝关节置换术后感染治疗进展. 中华关节外科杂志(电子版),2021,15(3):329-333. [31] GRAMMATOPOULOS G, BOLDUC ME, ATKINS BL, et al. Functional outcome of debridement, antibiotics and implant retention in periprosthetic joint infection involving the hip: a case-control study. Bone Joint J. 2017;99-B(5):614-622. [32] TOH RX, YEO ZN, LIOW M, et al. Debridement, Antibiotics, and Implant Retention in Periprosthetic Joint Infection: What Predicts Success or Failure? J Arthroplasty. 2021;36(10):3562-3569. [33] XU Y, WANG L, XU W. Risk factors affect success rate of debridement, antibiotics and implant retention (DAIR) in periprosthetic joint infection. Arthroplasty. 2020;2(1):37. [34] DENG W, LI R, SHAO H, et al. Comparison of the success rate after debridement, antibiotics and implant retention (DAIR) for periprosthetic joint infection among patients with or without a sinus tract. BMC Musculoskelet Disord. 2021;22(1):895. [35] SCHOLTEN R, KLEIN KP, GISOLF J, et al. Empiric antibiotic therapy in early periprosthetic joint infection: a retrospective cohort study. Eur J Orthop Surg Traumatol. 2021;33(1):29-35. [36] TATARELLI P, ROMANI T, SANTORO V, et al. Debridement, antibiotics and implant retention (DAIR): An effective treatment option for early prosthetic joint infections. J Infect Chemother. 2021;27(8):1162-1168. [37] SCHWARZKOPF R, MIKHAEL B, WRIGHT E, et al. Treatment failure among infected periprosthetic total hip arthroplasty patients. Open Orthop J. 2014;8:118-124. [38] HSU YH, HU CC, HSIEH PH, et al. Vancomycin and Ceftazidime in Bone Cement as a Potentially Effective Treatment for Knee Periprosthetic Joint Infection. J Bone Joint Surg Am. 2017;99(3):223-231. [39] WANG X, ZHANG W. Research progress of two-stage revision for periprosthetic joint infection after hip and knee arthroplasties. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi.2019;33(12):1566-1571. [40] JIANG Q, FU J, CHAI W, et al. Two-stage exchange Arthroplasty is a viable treatment for Periprosthetic joint infection in inflammatory diseases. BMC Musculoskelet Disord. 2020;21(1):681. [41] ZHANG Y, GAO Z, ZHANG T, et al. A comparsion study between debridement, antibiotics, and implant retention and two-stage revision total knee arthroplasty for the management of periprosthetic joint infection occurring within 12 weeks from index total knee arthroplasty. J Orthop Surg Res. 2022;17(1):330. [42] RUSSO A, CAVAGNARO L, CHIARLONE F, et al. Predictors of failure of two-stage revision in periprosthetic knee infection: a retrospective cohort study with a minimum two-year follow-up. Arch Orthop Trauma Surg. 2022;142(3):481-490. [43] RAJGOPAL A, PANDA I, RAO A, et al. Does Prior Failed Debridement Compromise the Outcome of Subsequent Two-Stage Revision Done for Periprosthetic Joint Infection Following Total Knee Arthroplasty?. J Arthroplasty. 2018;33(8):2588-2594. [44] TUECKING LR, SILLIGMANN J, SAVOV P, et al. Detailed Revision Risk Analysis after Single- vs. Two-Stage Revision Total Knee Arthroplasty in Periprosthetic Joint Infection: A Retrospective Tertiary Center Analysis. Antibiotics (Basel). 2021;10(10):1177. [45] LI Y, ZHANG X, GUO X, et al. Effective Treatment of Single-Stage Revision Using Intra-Articular Antibiotic Infusion for Polymicrobial Periprosthetic Joint Infection. J Arthroplasty. 2022;37(1):156-161. [46] CASTELLANI L, DANEMAN N, MUBAREKA S, et al. Factors Associated with Choice and Success of One- Versus Two-Stage Revision Arthroplasty for Infected Hip and Knee Prostheses. HSS J. 2017;13(3): 224-231. [47] FAGOTTI L, TATKA J, SALLES M, et al. Risk Factors and Treatment Options for Failure of a Two-Stage Exchange. Curr Rev Musculoskelet Med. 2018;11(3):420-427. [48] GOLDMAN AH, CLARK NJ, TAUNTON MJ, et al. Definitive Resection Arthroplasty of the Knee: A Surprisingly Viable Treatment to Manage Intractable Infection in Selected Patients. J Arthroplasty. 2020;35(3): 855-858. [49] YEUNG CM, LICHSTEIN PM, VARADY NH, et al. Knee Arthrodesis Is a Durable Option for the Salvage of Infected Total Knee Arthroplasty. J Arthroplasty. 2020;35(11):3261-3268. [50] HAWAMDEH ZM, OTHMAN YS, IBRAHIM AI. Assessment of anxiety and depression after lower limb amputation in Jordanian patients. Neuropsychiatr Dis Treat. 2008;4(3):627-633. [51] TROUILLEZ T, FAURE PA, MARTINOT P, et al. Above-the-knee amputation versus knee arthrodesis for revision of infected total knee arthroplasty: Recurrent infection rates and functional outcomes of 43 patients at a mean follow-up of 6.7 years. Orthop Traumatol Surg Res. 2021;107(4):102914. [52] VAN BELLEGHEM JD, MANASHEROB R, MIEDZYBRODZKI R, et al. The Rationale for Using Bacteriophage to Treat and Prevent Periprosthetic Joint Infections. Front Microbiol. 2020;11:591021. [53] FERRY T, KOLENDA C, BATAILLER C, et al. Phage Therapy as Adjuvant to Conservative Surgery and Antibiotics to Salvage Patients With Relapsing S. aureus Prosthetic Knee Infection. Front Med (Lausanne). 2020;7:570572. [54] DOUB JB, NG VY, JOHNSON AJ, et al. Salvage Bacteriophage Therapy for a Chronic MRSA Prosthetic Joint Infection. Antibiotics (Basel). 2020;9(5):241. [55] DOUB JB, NG VY, LEE M, et al. Salphage: Salvage Bacteriophage Therapy for Recalcitrant MRSA Prosthetic Joint Infection. Antibiotics (Basel). 2022;11(5):616. [56] DRAGO L, BOOT W, DIMAS K, et al. Does implant coating with antibacterial-loaded hydrogel reduce bacterial colonization and biofilm formation in vitro?. Clin Orthop Relat Res. 2014;472(11):3311-3323. [57] DE MEO D, CALOGERO V, ARE L, et al. Antibiotic-Loaded Hydrogel Coating to Reduce Early Postsurgical Infections in Aseptic Hip Revision Surgery: A Retrospective, Matched Case-Control Study. Microorganisms. 2020;8(4):571. [58] PELLEGRINI A, LEGNANI C. High rate of infection eradication following cementless one-stage revision hip arthroplasty with an antibacterial hydrogel coating. Int J Artif Organs. 2022;45(1):113-117. [59] FRANCESCHINI M, SANDIFORD NA, CERBONE V, et al. Defensive antibacterial coating in revision total hip arthroplasty: new concept and early experience. Hip Int. 2020;30(1_suppl):7-11. [60] CAPUANO N, LOGOLUSO N, GALLAZZI E, et al. One-stage exchange with antibacterial hydrogel coated implants provides similar results to two-stage revision, without the coating, for the treatment of peri-prosthetic infection. Knee Surg Sports Traumatol Arthrosc. 2018; 26(11):3362-3367. [61] FERRY T, BATAILLER C, PETITJEAN C, et al. The Potential Innovative Use of Bacteriophages Within the DAC((R)) Hydrogel to Treat Patients With Knee Megaprosthesis Infection Requiring “Debridement Antibiotics and Implant Retention” and Soft Tissue Coverage as Salvage Therapy. Front Med (Lausanne). 2020;7:342. [62] MANDELL JB, ORR S, KOCH J, et al. Large variations in clinical antibiotic activity against Staphylococcus aureus biofilms of periprosthetic joint infection isolates. J Orthop Res. 2019;37(7):1604-1609. [63] GARCÍA-GARCÍA J, AZUARA G, FRAILE-MARTINEZ O, et al. Modification of the Polymer of a Bone Cement with Biodegradable Microspheres of PLGA and Loading with Daptomycin and Vancomycin Improve the Response to Bone Tissue Infection. Polymers (Basel). 2022;14(5):888. [64] STOODLEY P, BROOKS J, PETERS CW, et al. Prevention and Killing Efficacy of Carbapenem Resistant Enterobacteriaceae (CRE) and Vancomycin Resistant Enterococci (VRE) Biofilms by Antibiotic-Loaded Calcium Sulfate Beads. Materials (Basel). 2020; 13(15):3258. [65] GHIRARDELLI S, FIDANZA A, PRATI P, et al. Debridement, antibiotic pearls, and retention of the implant in the treatment of infected total hip arthroplasty. Hip Int. 2020;30(1_suppl):34-41. [66] TARITY TD, XIANG W, JONES CW, et al. Do Antibiotic-Loaded Calcium Sulfate Beads Improve Outcomes After Debridement, Antibiotics, and Implant Retention? A Matched Cohort Study. Arthroplast Today. 2022;14:90-95. [67] CHANG MJ, LEE SA, KANG SB, et al. A retrospective comparative study of infection control rate and clinical outcome between open debridement using antibiotic-impregnated cement beads and a two-stage revision in acute periprosthetic knee joint infection. Medicine (Baltimore). 2020.99(4):e18891. [68] MOHAMED NS, DAVILA CI, ETCHESON JI, et al. Utilisation of calcium sulphate beads in one-stage aseptic revision total hip arthroplasty. Hip Int. 2022;32(5):656-660. [69] KALLALA R, HADDAD FS. Hypercalcaemia following the use of antibiotic-eluting absorbable calcium sulphate beads in revision arthroplasty for infection. Bone Joint J. 2015;97-B(9):1237-1241. [70] TARAR MY, TOE K, JAVED K, et al. The Risk of Iatrogenic Hypercalcemia in Patients Undergoing Calcium Sulphate Beads Implantation in Prosthetic Joint Surgery: A Systematic Review. Cureus. 2021;13(10):e18777. [71] 袁家威. 多种中药有效成分对假体周围感染临床分离金黄色葡萄球菌抑菌作用的研究[D].广州: 广州中医药大学,2021. [72] 张永芃. 五味消毒饮加减对全膝关节置换术后炎症指标变化趋势影响的临床研究[D]. 福州:福建中医药大学,2021. [73] 王大忠, 孙永强, 包伟东. 清创后普朗特液体敷料浸泡联合负压封闭引流和五味消毒饮内服治疗人工髋膝关节置换术后假体周围急性感染[J]. 中医正骨,2016,28(9):52-54. [74] 赖志宏, 黄竞威, 桑振飞, 等. 益气清热解毒法预防髋膝关节置换术后假体周围感染的疗效观察[J]. 中医临床研究,2018,10(28):1-4. [75] 黄平, 余南征, 杨林, 等. 归芪五味消毒饮联合抗生素预防关节置换术后感染的临床观察[J]. 宜春学院学报,2021,43(3):63-65. [76] 袁家威, 张海涛, 揭珂, 等. 基于网络药理学研究桃红四物汤治疗假体周围感染的潜在靶点和机制[J]. 中国组织工程研究,2021, 25(9):1428-1433. [77] 邓煜, 曹林虎, 白新文. 桃红四物汤合五味消毒饮加减预防全髋关节置换术后假体周围感染临床研究[J]. 实用中医药杂志,2018, 34(10):1143-1145. [78] JOSSE J, VALOUR F, MAALI Y, et al. Interaction Between Staphylococcal Biofilm and Bone: How Does the Presence of Biofilm Promote Prosthesis Loosening? Front Microbiol. 2019;10:1602. [79] 吐尔洪江·瓦哈甫. 关节假体周围感染的诊治及骨溶解机制研究[D]. 乌鲁木齐:新疆医科大学,2019. [80] 李盼祥, 刘晓峰, 蒋亮, 等. 桃红四物汤对老年骨质疏松性股骨粗隆间骨折患者PFNA术后血清RANKL、骨保护素水平及转化生长因子-β1表达水平的影响[J]. 中国老年学杂志,2018,38(2):408-410. [81] WU Z, WU H, LI C, et al. Daphnetin attenuates LPS-induced osteolysis and RANKL mediated osteoclastogenesis through suppression of ERK and NFATc1 pathways. J Cell Physiol. 2019;234(10):17812-17823. [82] JIANG T, GU H, WEI J. Echinacoside Inhibits Osteoclast Function by Down-Regulating PI3K/Akt/C-Fos to Alleviate Osteolysis Caused by Periprosthetic Joint Infection. Front Pharmacol. 2022;13:930053. [83] PENG KT, CHEN JL, KUO LT, et al. GMI, an Immunomodulatory Peptide from Ganoderma microsporum, Restrains Periprosthetic Joint Infections via Modulating the Functions of Myeloid-Derived Suppressor Cells and Effector T Cells. Int J Mol Sci. 2021;22(13):6854. [84] TAN J, WANG J, YANG C, et al. Antimicrobial characteristics of Berberine against prosthetic joint infection-related Staphylococcus aureus of different multi-locus sequence types. BMC Complement Altern Med. 2019;19(1):218. [85] LI H, TANG D, QI C, et al. Forsythiaside inhibits bacterial adhesion on titanium alloy and attenuates Ti-induced activation of nuclear factor-kappaB signaling-mediated macrophage inflammation. J Orthop Surg Res. 2018;13(1):139. [86] ZHU XY, ZENG YR. Garlic extract in prosthesis-related infections: a literature review. J Int Med Res. 2020;48(4):1220713330. [87] LUM ZC, HOLLAND CT, MEEHAN JP. Systematic review of single stage revision for prosthetic joint infection. World J Orthop. 2020;11(12):559-572. [88] NEUFELD ME, LIECHTI EF, SOTO F, et al. High revision rates following repeat septic revision after failed one-stage exchange for periprosthetic joint infection in total knee arthroplasty. Bone Joint J. 2022;104-B(3):386-393. |
| [1] | 闵美鹏, 吴 进, URBA RAFI, 张文杰, 高 嘉, 王云华, 何 斌, 范 磊. 全髋关节置换前人工智能(AI)规划的作用与意义[J]. 中国组织工程研究, 2024, 28(9): 1372-1377. |
| [2] | 单嘉欣, 张一龙, 吴鸿涛, 张家媛, 李安安, 刘文刚, 许学猛, 赵传喜. 全膝关节置换后服用健脾益气活血方患者肌力及疼痛的变化[J]. 中国组织工程研究, 2024, 28(9): 1378-1382. |
| [3] | 齐浩东, 鲁 超, 徐韩博, 王孟飞, 郝阳泉. 糖尿病对初次全膝关节置换围术期失血量和疼痛的影响[J]. 中国组织工程研究, 2024, 28(9): 1383-1387. |
| [4] | 李孝强, 陈 唯, 李明樾, 单天驰, 申 文. 全膝关节置换前股四头肌超声定量分析对置换后慢性疼痛的预测价值[J]. 中国组织工程研究, 2024, 28(9): 1388-1393. |
| [5] | 钟 俊, 王 文. 不同解剖修复策略改善慢性踝关节外侧不稳的网状Meta分析[J]. 中国组织工程研究, 2024, 28(9): 1470-1476. |
| [6] | 章晓云, 刘 桦, 柴 源, 陈 锋, 曾 浩, 高振罡, 黄有荣. 益肾固疏方干预老年性骨质疏松症患者骨代谢标志物的变化及临床疗效[J]. 中国组织工程研究, 2024, 28(8): 1155-1160. |
| [7] | 王体惠, 王 旭, 吴锦清, 陈继良, 王晓露, 缪 娟. 股骨远端三维模拟截骨在膝关节置换中的应用[J]. 中国组织工程研究, 2024, 28(6): 905-910. |
| [8] | 郑加法, 宋秀锋, 李宏志, 周锦明, 关盛溢, 于 鹤. 经跟腱旁入路切开复位内固定治疗后踝夹心形骨折[J]. 中国组织工程研究, 2024, 28(6): 934-938. |
| [9] | 杨毅峰, 黄 健, 叶 楠, 王 琳. 全膝关节置换中的缺血再灌注损伤[J]. 中国组织工程研究, 2024, 28(6): 955-960. |
| [10] | 毕玉杰, 马笃军, 彭力平, 周紫琼, 赵 静, 朱厚均, 钟秋辉, 杨玉鑫. 中医药联合医用水凝胶治疗疾病的策略及意义[J]. 中国组织工程研究, 2024, 28(3): 419-425. |
| [11] | 柴 爽, 马江涛, 杨岩冰, 苏晓川, 谢 艳, 滕军燕, 秦 娜. 雌激素受体在骨疏康治疗绝经后骨质疏松症中的作用与机制[J]. 中国组织工程研究, 2024, 28(16): 2574-2578. |
| [12] | 高振罡, 章晓云, 蒋 文. 铁死亡在骨关节炎中的作用机制及其中医药干预研究进展[J]. 中国组织工程研究, 2024, 28(14): 2242-2247. |
| [13] | 范志鸿, 张 贤, 李 超. 椎间盘退变中的Wnt信号通路[J]. 中国组织工程研究, 2024, 28(12): 1950-1955. |
| [14] | 李 亭, 廖文鳌, 钟文杰, 刘希麟, 王 飞, 胡 豇. 机器人辅助微创腰椎后路融合治疗腰椎退行性疾病[J]. 中国组织工程研究, 2024, 28(12): 1855-1862. |
| [15] | 张 凯, 郭卓涛, 马桥桥, 查国春, 郭开今. 人工智能三维规划系统在全髋关节置换中的准确性及其影响因素[J]. 中国组织工程研究, 2024, 28(12): 1863-1868. |
1.1.1 检索人及检索时间 第一作者于2022年10月进行文献检索。
1.1.2 检索数据库 中文数据库:中国知网(CNKI)、万方、维普;英文数据库:PubMed。
1.1.3 检索文献时限 2000年1月至2022年10月。
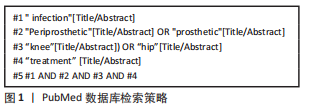
1.1.4 检索词 中文数据库分别以主题、摘要、题目,全文进行检索,检索词包括“假体,感染”“临床,治疗”“关节置换术,髋,膝”;英文数据库分别以Title、Abstract进行检索,检索词包括“periprosthetic,prosthetic”“knee,hip”“infection”“treatment”。1.1.5 检索文献类型 随机对照研究、队列研究、病例对照研究、病例报告、综述、荟萃分析、临床实践指南。
1.1.6 检索路径 中文数据库检索策略:以知网为例:(SU=假体 AND SU=感染) AND (SU=髋 OR SU=膝 OR SU=关节置换术)AND (SU=治疗 OR SU=临床)。英文数据库检索策略:PubMed数据库检索策略见图1。
1.3 排除标准 与此文主旨不相符、内容重复、数据可靠性低、观点过时的文献。
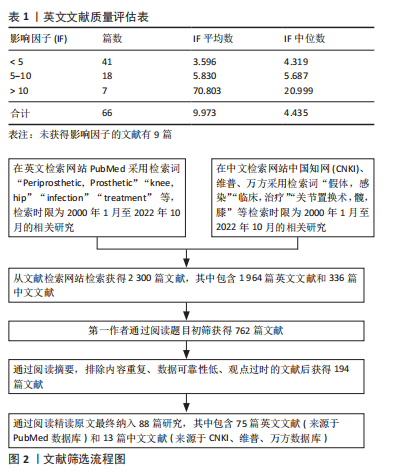
1.4 质量评估及数据提取 检索并排除重复文献后获得2 300篇文献(1 964篇英文文献+336篇中文文献),第一作者通过阅读题目初筛获得762篇文献,然后通过阅读摘要,排除内容重复、数据可靠性低、观点过时的文献后获得194篇文献,再通过精读原文最终纳入88篇文献,其中包含75篇英文文献(质量评估见表1)和13篇中文文献。文献检索流程见图2。
抗生素方面,耐药菌发生率的增加致使传统抗生素“失灵”,解决耐药问题仍是抗生素治疗方面的研究重点,组合型抗生素给药方案或有助于根除感染,最佳搭配方案待挖掘,安全性需要更进一步验证;通过应用更高效率的载药系统,靶向针对生物膜治疗的抗生素给药方案是治疗PJI的新兴热门治疗策略。
手术方面,在可见的短期未来里,Ⅱ期翻修术作为PJI最重要的治疗手段的地位不会改变,但对于DAIR和Ⅰ期翻修术来说,术后中长期感染的根除率和假体存活率在一些时候也不弱于Ⅱ期翻修术,手术成功率的增长或与更为优化的抗菌药给药方式、组合方案有关,且其更低的经济成本和更短的疗程对于患者来说更易接受。不过也存在一些问题,DAIR在PJI发生后抗生素应用时间的范围尚未明确,其在血源性或晚期急性PJI中的应用也存在着争议;对于Ⅰ期翻修,尽管文献中报告其与Ⅱ期翻修成功率接近,但是样本量较小,存在偏倚风险[87],且Ⅰ期翻修后失败的病例再翻修失败风险可能更高[88]。
生物治疗是PJI治疗中的新兴手段,在少量的临床样本中,噬菌体疗法表现出对耐药菌PJI治疗的优势;新式的抗生素载药系统在部分欧洲国家已开始应用,水凝胶载药系统在预防、治疗PJI方面可能优于传统抗生素载药系统;但抗生素硫酸钙珠载药系统在DAIR、翻修术中根除感染效果表现不佳,且其溶解后可能使血钙浓度上升,破坏了内环境电解质的稳态,安全性有待进一步验证。
中医药治疗手段在关节置换术后能有效减轻炎症反应、降低感染概率,PJI发生后配合抗生素治疗效果优于单纯使用抗生素,近年来,也有部分研究发现中医药在治疗假体周围感染发生后的骨溶解具有潜在价值,但缺乏更高级的循证医学证据,需要更多前瞻性研究来验证其有效性。 中国组织工程研究杂志出版内容重点:人工关节;骨植入物;脊柱;骨折;内固定;数字化骨科;组织工程
 #br#
#br#
文题释义:
关节置换:采用人工关节替代无法继续使用的关节的一种手术治疗手段。目前,关节置换术是关节疾病终末期最常用的一种治疗手段。假体周围感染:在人工植入物邻近组织发生的一种感染性疾病,此文特指髋、膝关节置换术后假体周围感染,主要表现为人工关节周围的红肿、疼痛、皮温升高、关节活动功能障碍以及关节周围骨质溶解、破坏,形成窦道,少部分可伴有全身性感染症状。
假体周围感染治疗的难点在于细菌常附着于人工关节表面后形成寻常抗生素治疗方案难以消灭的生物膜。当这些生物膜产生以后,关节假体表面便成了细菌的容器,造成持续性的慢性感染,生物膜为细菌提供了庇护,免受来自宿主免疫效应和抗菌药物的打击。假体周围感染的临床治疗研究目的在于提高各治疗方法的感染根除率,提高患者的生存率,缩短住院时间,减少医疗费用,改善患者的生活质量。本文总结了近年来已应用于假体周围感染的治疗方法,阐明了各治疗方法的现有的部分问题,对未来的研究方向进行了展望,并创新性总结了中医药在假体周围感染的预防、治疗中的应用,挖掘了中医药对假体周围感染的应用潜力。
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||