脑性瘫痪指由于出生前、出生时至出生后的婴幼儿脑发育早期,由于多种原因造成的非进行性的脑损伤或发育缺陷所致的中枢性运动障碍及姿势异常症候群,可伴有智能低下及惊厥发作、行为异常、感觉障碍、语言及精神行为怪异及其他异常[5]。中国人口众多,脑性瘫痪患者数量位居全球首位[6]。
脑性瘫痪患儿易出现全身关节的畸形发育。其中髋关节畸形是痉挛型脑性瘫痪患儿常见的肌肉骨骼系统畸形,其发生率仅低于足踝部、膝关节畸形。一项匈牙利流行病学调查显示,严重的脑性瘫痪患儿中髋关节半脱位或者全脱位比例为2.5%-59%[7],脑性瘫痪患儿中尤其以痉挛型双肢瘫、三肢瘫、四肢瘫的儿童更易出现髋关节畸形[8]。脊柱畸形同样是脑性瘫痪患儿常常出现的畸形之一,研究认为其发生率往往随着患儿活动受累程度的增加而增加[9]。幼年患有严重脊柱畸形的脑性瘫痪患儿,其脊柱畸形可能存在更高的进展风险,究其原因,多数学者认为也许由于患儿骨盆倾斜、疼痛等导致行动时的失衡[10]。其次,痉挛型脑性瘫痪患儿痉挛的高张力肌肉对其附着的骨骼有直接的牵拉作用,也可能是导致腰椎及髋等骨关节畸形的直接原因之一。除此以外,由于脑性瘫痪的病因至今仍未达成完全共识,许多研究者也相信先天发育畸形、或先天神经发育直接导致的畸形也可能是其发病的重要因素。
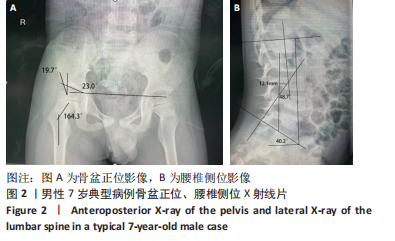
一般认为,儿童的骨骼发育集中在胚胎早期至青春期结束。在国内,医疗机构接诊小年龄幼儿脑性瘫痪患者的情况是较少见的。普通健康儿童3岁时即发育起较成熟的粗大运动功能,如独走、简单跑跳、上下楼梯,由于缺乏相应的早期筛查,患儿往往在两三岁后因发育明显较同龄人迟缓,如无法独站、独走而引起监护人的注意,此后才在求医过程中经医疗机构诊断为脑性瘫痪。徐林[8]认为脑性瘫痪的治疗越早越好,但其外科手术的最佳治疗时间是6岁左右,有些需要关节矫形的患儿治疗期应延长至十二三岁,而成人患者除了单纯的肌肉痉挛、关节畸形外,会逐渐出现一些新问题,如继发的慢性疲劳、骨骼肌肉疼痛、显著的功能退化、神经损伤或衰老,一般难以取得非常良好的治疗效果。此文将入组年龄限定在3-18岁,以求能够能最好地反映痉挛型脑性瘫痪患儿骨骼发育情况,而不受到其他继发问题影响。
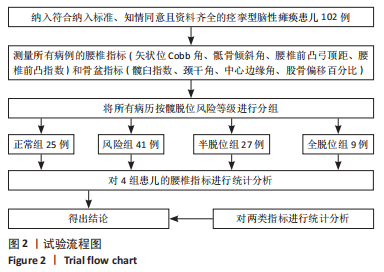
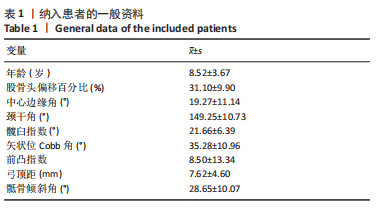
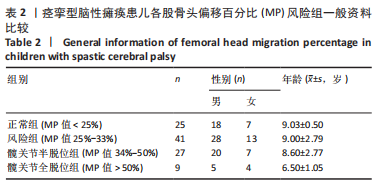
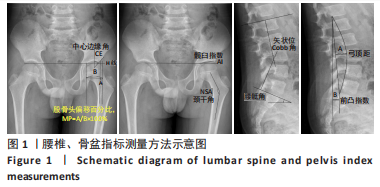
MP最早由BEALS描述,反映股骨头偏离髋臼的程度。1988年EKLÖF等[11]通过一项对500余例儿童的临床观察,确定了股骨偏移百分比在髋关节脱位及半脱位临床诊断及预防上的重要价值。其由于拍摄受体位影响小、易于测量观察、数值稳定,被多数学者认为是临床评估髋关节发育情况的重要指标[12]。如果单纯以MP为标准进行髋关节脱位程度的划分,则以MP < 25%作为髋关节发育正常,以25%-33%评估为髋关节存在脱位风险,以33%-50%评估为髋关节半脱位,而当MP > 50%时,则表明患者已进行至髋关节严重脱位。中心边缘角表示髋臼与股骨头相对的位置关系,间接反映髋臼发育不良的程度,利用中心边缘角判断临床髋关节发育的历史久远,1976年FREDENSBORG[13]对中心边缘角进行测量统计,将正常范围确定为25°-51°,该标准沿用至今。颈干角提示髋有无内、外翻畸形,研究提出,在脑性瘫痪患儿的临床X射线片相关指标中,颈干角是反映脑性瘫痪患儿髋关节发育异常的有效指标之一[14]。髋臼指数反映髋臼发育程度,其可以较好地反映和预测髋脱位的情况,髋臼指数越大,则股骨头和髋臼之间剪切力越大,则脱位风险越大[15]。腰椎指标方面,Cobb角作为最常用的腰椎畸形指标,通过直接测量角度反映腰椎矢状面的畸形程度。同样的,弓顶距通过直接测量距离反映腰椎前凸或后凸的程度。腰椎前凸指数和骶骨倾斜角取决于骨盆的形态和位置,诸多研究表明,这一对指标间显著相关,前凸指数过大或严重的骶骨倾斜角会导致坐姿困难和软组织压力性损伤,意味着更严重的畸形,此二者可以共同反映腰椎的矢状位形态[16-18]。
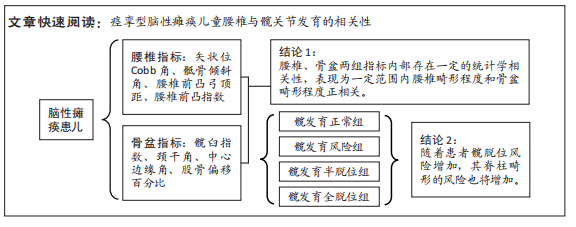
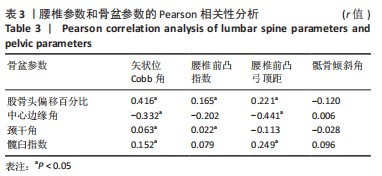
在此次研究中,Pearson卡方检验表明的几组具有相关性的变量组分别为:①正相关:MP与矢状位Cobb角、MP与弓顶距、MP与腰椎前凸指数、髋臼指数与矢状位Cobb角、髋臼指数与弓顶距;②负相关:中心边缘角与矢状位Cobb角、中心边缘角与弓顶距;③不相关或极弱相关:颈干角与矢状位Cobb角、颈干角与前凸指数。可以得出,MP与髋臼指数这一对反映髋脱位及髋臼发育的指标,和矢状位Cobb角与腰椎前凸弓顶距这一对反映腰椎前凸情况的指标,具有较强关联性,并表现为正相关。这意味着痉挛型脑性瘫痪患儿腰椎影像指标与髋关节发育存在一定关系,表现为骨盆畸形程度和腰椎畸形程度具有协同性,但此次研究尚不能确定其因果关系和影响顺序。除此以外,此次试验尚发现颈干角与腰椎部分指标存在显著不相关,这也许意味着髋的内、外翻畸形也许和腰椎矢状位畸形是两个独立因素。但此猜想仍待进一步研究验证。
在以MP为标准分组后的组间分析及两两分析中可以得出,在半脱位及以下风险中,随着髋脱位风险的上升,矢状位Cobb角、前突指数、弓顶距均存在显著增大,即说明腰椎前凸的风险也随之上升。但在全脱位组,即MP > 50%的患者中,虽然矢状位Cobb角仍然保持着显著增大的趋势,但前突指数和弓顶距的增大趋势却不明显了,骶骨倾斜角甚至出现了均值的下降,这意味着腰椎前凸的风险出现不显著上升或轻度下降。研究表明,MP值与脑性瘫痪患儿粗大运动功能分级密切相关,即脱位情况越重,运动功能越差[19]。因此作者猜测,髋脱位严重的患儿可能由于行动受限,运动量减少,从而导致腰椎的代偿性前凸变化也相应减小。此猜想仍待进一步研究验证。
多数研究认为,脑性瘫痪患儿的脊柱畸形多继发于骨盆畸形之后[20-21],患儿由于内收肌、髋屈肌和大腿内侧肌群痉挛,这些肌肉肌力和肌张力的失衡导致继发骨性畸形,如髋臼发育不良,并导致髋关节不稳定进而发生脱位。脊柱-骨盆-下肢为人体力线的重要结构,维持其矢状面和冠状面平衡才能保持正常的人体力线。作为躯干和下肢间至关重要的受力结构[22],髋关节和骨盆的畸形将引起全身的代偿性姿势异常,继而引发多数脊柱畸形。新的畸形需要更严重的异常体态来代偿,反过来再次对髋关节和骨盆的结构造成负面影响。其具体机制分为两个方面来讨论:①髋脱位加重脊柱畸形:髋关节为多个肌肉共同附着点,各组肌肉协助髋关节承重,控制髋关节屈曲和旋转,维持下肢力线稳定。痉挛型脑性瘫痪患儿表现为肌张力高,紧张挛缩的肌群导致髋关节的内收和屈曲,在双下肢痉挛程度相等或不等时,将会使下肢力线向后或向侧移,为维持直立姿势,腰椎发生代偿性前凸或侧凸。②脊柱畸形导致髋关节发育不良,这类临床研究数量不多,具体机制有待进一步研究证实。前凸的脊柱和前倾的骨盆易导致向后方脱位,侧弯的脊柱则会引发骨盆旋转,这也将导致髋关节脱位的发生。
由于严重的髋关节脱位情况下,髋臼对股骨头的覆盖程度越低,股骨头位于髋臼外部的面积越大,则患儿在日常行动时躯干的质量越难以垂直传递到双侧股骨,从而导致股骨头在重力和较浅髋臼的作用下,向后外侧移位更加严重,表现为MP值倾向于继续升高。在一定范围内,MP值的继续升高很可能导致脊柱畸形的恶化,数种代偿互相促进,从而可能使整个病情加快进展速度。因此也提示了脑性瘫痪患儿肢体畸形和异常体态进行尽早治疗、矫正的重要性。
在此次研究中,骶骨倾斜角作为反映腰椎矢状位形态的一项参数,并未表现出较大的特异性。不过这并不说明骶骨倾斜角与髋脱位畸形情况没有联系,这仍有待更大样本量的试验或更全面的试验设计进行一步探索。
目前国内外学者在患儿腰椎和髋关节发育之间的关系虽然在一定范围内达成共识,但由于缺乏大样本的临床试验,该病的罕见程度及不同国家地区儿童发育的情况不一,世界范围内关于此主题仍存在较多不同的声音。HODGKINSON等[1]将234例15岁以上脑性瘫痪患者分为单侧髋脱位组和正常组,探索各组脊柱侧弯的进展率,发现两组进展速度无明显差异。PORTER等[23]通过一个纳入747例参与者的全年龄患者的研究观察到,单侧髋脱位确实对脊柱畸形的发生进展有显著影响。此次研究在前人的基础上取舍后,确定了更严格的入组标准,包括更窄的年龄区间和治疗方式,以求获得尽量纯粹的结果。但同时此次研究以单纯的客观影像学资料为依据,仍然存在不够全面的问题。
此次研究存在以下局限性:第一,纳入病例以学龄期患儿为主,也存在学龄前和青春期儿童。儿童的骨骼发育与成人不同,不同年龄段的健康儿童腰椎与骨盆的发育尚有规律可循,但骨骼系统的发育不仅仅与生物年龄相关,也与儿童的活动量、日常姿态密不可分。脑性瘫痪患儿本身活动受限者数量较大,受限程度、模式都有不同,必然会对骨骼发育造成不同的影响。结合生物年龄和活动能力双重因素,为了得到更平稳的基线数据,则要求更大的样本量。这可能对此次研究的结果产生影响。第二,患儿存在肌肉痉挛、运动障碍等,在拍摄X射线片时存在姿势不标准的情况,这可能对结果产生影响。
在实际的临床治疗中,患儿常常因为监护人甚至临床医生的拖延或对治疗方式的不当选择而延误治疗,这是人们对疾病的认识不足导致的。四肢的高张力和痉挛状态已经对患儿行动能力造成较大的影响,其继发或先天的髋关节畸形和腰椎畸形再次对患儿的日常生活带来更多不便,二者相互影响,促进病情快速发展。徐林[8]认为,如果患儿5岁前即采取系统疗法进行积极治疗,多数患儿可以取得良好效果而免于手术。因而,此次研究提示,在临床工作中,对于年龄小的患儿,应当重视关节和肢体的畸形情况,对痉挛型脑性瘫痪患儿的肢体畸形和姿势异常应采取早发现、早治疗、早矫正的方式,以延缓腰椎和骨盆畸形的后续发展。
此次研究通过对脑性瘫痪患儿腰椎和骨盆的影像学资料的研究,发现脑性瘫痪患儿腰椎发育与骨盆髋关节发育有密切关联,尤其是腰椎前凸畸形和髋关节脱位畸形的关系最明显。髋关节发育异常会导致脊柱畸形,因此要提前预防髋脱位,佩戴矫形器或者进行早期手术干预,预防脊柱畸形。
中国组织工程研究杂志出版内容重点:组织构建;骨细胞;软骨细胞;细胞培养;成纤维细胞;血管内皮细胞;骨质疏松;组织工程