[1] BEATA Ż, ALEKSANDRA SR, URSZULA L, et al. Structure and Pathologies of Articular Cartilage. In Vivo. 2021;35:1355-1363.
[2] ABHIJIT MB, JAMES BR. Articular cartilage: structure, injuries and review of management. Br Med Bull. 2008;87:77-95.
[3] JOSÉ B, JOSÉ AA, ENRIQUE G, et al. Articular cartilage: structure and regeneration. Tissue Eng Part B Rev. 2010;16:617-627.
[4] MATTHEW JK, JOHN WB, JUSTIN MP, et al. Microfracture Versus Autologous Chondrocyte Implantation for Articular Cartilage Lesions in the Knee: A Systematic Review of 5-Year Outcomes. Am J Sports Med. 2018;46:995-999.
[5] REISSIS D, TANG QO, COOPER NC, et al. Current clinical evidence for the use of mesenchymal stem cells in articular cartilage repair. Expert Opin Biol Ther. 2016; 16(4):535-557.
[6] XIN L, ZHANG C, XU WX, et al. Current advances on surgical treatment for knee articular cartilage injuries. Zhongguo Gu Shang. 2018;31:281-285.
[7] HÖNLE W, JEZUSSEK D, FABIJANI R, et al. Surgical treatment of knee osteoarthritis. MMW Fortschr Med. 2007;149:33-34,36.
[8] CHASE SD, JORGE C, CRUZ RS, et al. Fresh Osteochondral Allograft Transplantation for Treatment of Articular Cartilage Defects of the Knee. Arthrosc Tech. 2016;5: e157-161.
[9] EREN Y, ALI E, EMRE Y, et al. The Effect of Intraarticular Insulin on Chondral Defect Repair. Cartilage. 2021;13:684S-691S.
[10] RIMTAUTAS G, AGNE G, ARNOLDAS P, et al. Ten-year follow-up of a prospective, randomized clinical study of mosaic osteochondral autologous transplantation versus microfracture for the treatment of osteochondral defects in the knee joint of athletes. Am J Sports Med. 2012;40:2499-2508.
[11] SAHAR J, SADRABADI AMIN E, FATEMEH Z, et al. New Insights into Cartilage Tissue Engineering: Improvement of Tissue-Scaffold Integration to Enhance Cartilage Regeneration. Biomed Res Int. 2022;2022:7638245.
[12] 杨东翔,元香南,孔战,等.组织工程软骨的研究现状与进展[J].山东医药, 2011,51(40):113-114.
[13] HOLZAPFEL BM, RUDERT M, HUTMACHER DW. Scaffold-based Bone Tissue Engineering. Orthopade. 2017;46:701-710.
[14] ABIY W, ELENI KT, CAGRI A, et al. Current state of fabrication technologies and materials for bone tissue engineering. Acta Biomater. 2018;80:1-30.
[15] 张佼佼,王冬青,王志强,等.组织工程软骨支架材料的应用选择[J].中国组织工程研究与临床康复,2011,15(29):5467-5470.
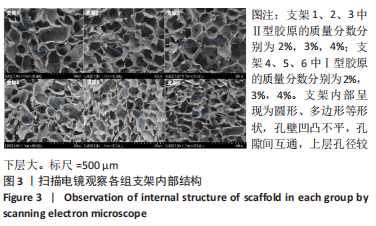
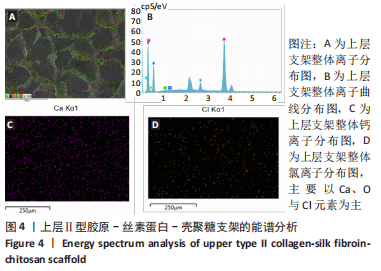
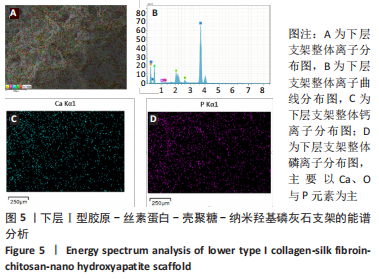
[16] XIAO HL, HUANG WL, XIONG K, et al. Osteochondral repair using scaffolds with gradient pore sizes constructed with silk fibroin, chitosan, and nano-hydroxyapatite. Int J Nanomedicine. 2019;14:2011-2027.
[17] LU ZH, LEI DQ, JIANG TM, et al. Nerve growth factor from Chinese cobra venom stimulates chondrogenic differentiation of mesenchymal stem cells. Cell Death Dis. 2017;8:e2801.
[18] ZHAN XT, CAI PA, LEI DQ, et al. Comparative profiling of chondrogenic differentiation of mesenchymal stem cells (MSCs) driven by two different growth factors. Cell Biochem Funct. 2019;37:359-367.
[19] JI L, SONG ZW, ZENG FH, et al. Research progress on controlled release of various growth factors in bone regeneration. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2019;33:750-755.
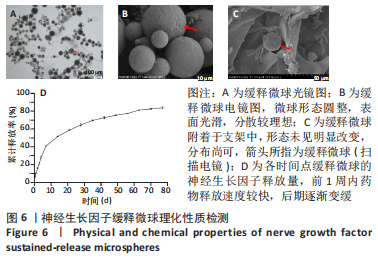
[20] CHEN ZJ, CHENG Q, YU XF, et al. Research progress of growth factor sustained -release microspheres in fat transplantation. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2017;31:1402-1406.
[21] 王富友.组织工程骨软骨仿生设计与初步构建[D].重庆:第三军医大学,2008.
[22] LEVINGSTONE TJ, THOMPSON E, MATSIKO A, et al. Multi-layered collagenbased scaffolds for osteochondral defect repair in rabbits. Acta Biomater. 2016;32:149-160.
[23] LEVINGSTONE TJ, MATSIKO A, DICKSON GR, et al. A biomimetic multilayered collagen-based scaffold for osteochondral repair. Acta Biomater. 2014;10:1996-2004.
[24] FU LW, YANG Z, GAO CJ, et al. Advances and prospects in biomimetic multilayered scaffolds for articular cartilage regeneration. Regen Biomater. 2020;7:527-542.
[25] 康嘉宇,吕建伟,赵志虎,等.骨软骨组织工程分层支架的研究进展[J].中华骨科杂志,2019,39(22):1413-1420.
[26] PEREIRA DR, RUI L REIS RL, OLIVEIRA JM. Layered Scaffolds for Osteochondral Tissue Engineering. Adv Exp Med Biol. 2018;1058:193-218.
[27] IVANA G, GORDAN VN.Challenges in engineering osteochondral tissue grafts with hierarchical structures. Expert Opin Biol Ther. 2015;15:1583-1599.
[28] 朱浩方,毛宏理,顾忠伟.医用组织粘合剂的研究进展[J].中国材料进展,2020, 39(Z1):535-550+557-558.
[29] KAZUNORI S, YU M, CHRISTOPHER DM, et al. Osteochondral tissue engineering with biphasic scaffold: current strategies and techniques. Tissue Eng Part B Rev. 2014; 20:468-476.
[30] PROMITA B, BANANI K, DEBOKI N, et al. Silk scaffolds in bone tissue engineering: An overview. Acta Biomater. 2017;63:1-17.
[31] WALTER B, WEERASAK S, ARAMWIT P, et al. Natural Origin Materials for Osteochondral Tissue Engineering. Adv Exp Med Biol. 2018;1058:3-30.
[32] MIRIAM F, GORDIAN B, MANSOOR C, et al. Natural Polymeric Scaffolds in Bone Regeneration. Front Bioeng Biotechnol. 2020;8:474.
[33] JOANNE R, JOHN R, KEVIN MS, et al. Biomaterials and scaffold design: key to tissue-engineering cartilage. Biotechnol Appl Biochem. 2007;46:73-84.
[34] DEL BAKHSHAYESH AR, ASADI N, ALIHEMMATI A, et al. An overview of advanced biocompatible and biomimetic materials for creation of replacement structures in the musculoskeletal systems: focusing on cartilage tissue engineering. J Biol Eng. 2019;13:85.
[35] NAZANIN A, MARZIYEH F, NOROOZI PN, et al. Bioactive polymeric scaffolds for osteogenic repair and bone regenerative medicine. Med Res Rev. 2020;40:1833-1870.
[36] MANO JF, REIS RL. Osteochondral defects: present situation and tissue engineering approaches. J Tissue Eng Regen Med. 2007;1:261-273.
[37] HUTMACHER DW. Scaffolds in tissue engineering bone and cartilage. Biomaterials. 2000;21:2529-2543.
[38] SMITH GD, KNUTSEN G, RICHARDSON JB. A clinical review of cartilage repair techniques. J Bone Joint Surg Br. 2005;87:445-449.
[39] TANYA JL, AMOS M, GLENN RD, et al. A biomimetic multi-layered collagen-based scaffold for osteochondral repair. Acta Biomater. 2014;10:1996-2004.
[40] MASTROGIACOMO M, MURAGLIA A, KOMLEV V, et al. Tissue engineering of bone: search for a better scaffold. Orthod Craniofac Res. 2005;8:277-284.
[41] 高泽,石志良,李锋,等.材料和孔隙率对可降解支架内骨形成的影响[J].医用生物力学,2021,36(4):582-588.
[42] LAMINE C, JÉRÔME C, MARION D, et al. Autologous osteochondral mosaicplasty in osteochondritis dissecans of the patella in adolescents. Int Orthop. 2017;41:197-202.
[43] AARON JK, HEATHER WH, SCOTT AR, et al. Activity levels are higher after osteochondral autograft transfer mosaicplasty than after microfracture for articular cartilage defects of the knee: a retrospective comparative study. J Bone Joint Surg Am. 2012;94:971-978.
[44] MARCUS M, ANDREA B, SYLVIE M, et al. Nasal chondrocyte-based engineered autologous cartilage tissue for repair of articular cartilage defects: an observational first-in-human trial. Lancet. 2016;388:1985-1994.
[45] MAURILIO M, ELIZAVETA K, MARCO D, et al. Arthroscopic autologous osteochondral grafting for cartilage defects of the knee: prospective study results at a minimum 7-year follow-up. Am J Sports Med. 2007;35:2014-2021.
[46] WIDYASRI P, YOSHIHITO N, SILVIA G, et al. Bone ingrowth of various porous titanium scaffolds produced by a moldless and space holder technique: an in vivo study in rabbits. Biomed Mater. 2016;11:015012.
[47] ORTH M, FRITZ T, STUTZ J, et al. Local Application of Mineral-Coated Microparticles Loaded With VEGF and BMP-2 Induces the Healing of Murine Atrophic Non-Unions. Front Bioeng Biotechnol. 2021;9:809397.
[48] MIKAËL MM, PRISCILLA SB, KENTA M, et al. Extracellular matrix-inspired growth factor delivery systems for bone regeneration. Adv Drug Deliv Rev. 2015;94:41-52.
[49] VALENTINA D, ELISA L, GABRIELA C, et al. Growth factors in bone repair. Chir Organi Mov. 2008;92:161-168.
[50] 刘华蔚.壳聚糖导管复合NGF缓释微球修复兔面神经缺损的实验研究[D].北京:中国人民解放军军医进修学院,2011.
[51] ZHANG JX, ZHU KJ, CHEN D. Preparation of bovine serum albumin loaded poly (D, L-lactic -co-glycolic acid) microspheres by a modified phase separation technique. J Microencapsul. 2005;22:117-126.
[52] KEN Y, KATHY T, SHALLEY AR, et al. Osteochondral repair using an acellular dermal matrix-pilot in vivo study in a rabbit osteochondral defect model. J Orthop Res. 2018;36:1919-1928.
[53] TROY DB, ADETOLA BA, NADR MJ, et al. Articular Cartilage Repair with Mesenchymal Stem Cells After Chondrogenic Priming: A Pilot Study. Tissue Eng Part A. 2018;24: 761-774.
[54] HUANG Y, FAN HQ, GONG XY, et al. Scaffold With Natural Calcified Cartilage Zone for Osteochondral Defect Repair in Minipigs .Am J Sports Med. 2021;49:1883-1891.
[55] IRINA AD M, RAFAEL AVB, HAROLD B, et al. Fixation of Hydrogel Constructs for Cartilage Repair in the Equine Model: A Challenging Issue. Tissue Eng Part C Methods. 2017;23:804-814.
[56] FREED LE, GRANDE DA, LINGBIN Z, et al. Joint resurfacing using allograft chondrocytes and synthetic biodegradable polymer scaffolds. J Biomed Mater Res. 1994;28:891-899.
[57] ISABEL RD, CARLOS AV, PEDRO PC. Large Animal Models for Osteochondral Regeneration. Adv Exp Med Biol. 2018;1059:441-501.
|