[1] LIU M, WU B, WANG WZ, et al. Stroke in China: epidemiology, prevention, and management strategies. Lancet Neurol. 2007;6(5): 456-464.
[2] FALLENIUS M, SKRIFVARS MB, REINIKAINEN M, et al. Spontaneous Intracerebral Hemorrhage. Stroke. 2019;50(9):2336-2343.
[3] TSAI CF, THOMAS B, SUDLOW CL. Epidemiology of stroke and its subtypes in Chinese vs white populations: a systematic review. Neurology. 2013;81(3):264-272.
[4] GONG YH, HAO SL, WANG BC. Mesenchymal Stem Cells Transplantation in Intracerebral Hemorrhage: Application and Challenges. Front Cell Neurosci. 2021;15:653367.
[5] EL ANDALOUSSI S, MÄGER I, BREAKEFIELD XO, et al. Extracellular vesicles: biology and emerging therapeutic opportunities. Nat Rev Drug Discov. 2013;12(5):347-357.
[6] PHINNEY DG, PITTENGER MF. Concise Review: MSC-Derived Exosomes for Cell-Free Therapy. Stem Cells. 2017;35(4):851-858.
[7] YAGHOUBI Y, MOVASSAGHPOUR A, ZAMANI M, et al. Human umbilical cord mesenchymal stem cells derived-exosomes in diseases treatment. Life Sci. 2019;233:116733.
[8] 刘超,张丽君,陶昊,等.基于细胞生物学方法比较5种不同组织来源间充质干细胞的特征[J].中国组织工程研究,2019,23(33): 5334-5340.
[9] OTERO-ORTEGA L, GÓMEZ DE FRUTOS MC, LASO-GARCÍA F, et al. Exosomes promote restoration after an experimental animal model of intracerebral hemorrhage. J Cereb Blood Flow Metab. 2018;38(5):767-779.
[10] CAI Y, LIU W, LIAN L, et al. Stroke treatment: Is exosome therapy superior to stem cell therapy. Biochimie. 2020;179:190-204.
[11] DUAN S, WANG F, CAO J, et al. Exosomes Derived from MicroRNA-146a-5p-Enriched Bone Marrow Mesenchymal Stem Cells Alleviate Intracerebral Hemorrhage by Inhibiting Neuronal Apoptosis and Microglial M1 Polarization. Drug Des Devel Ther. 2020;14:3143-3158.
[12] LI Q, HAN X, LAN X, et al. Inhibition of neuronal ferroptosis protects hemorrhagic brain. JCI Insight. 2017;2(7):e90777.
[13] SHOAMANESH A, KATSANOS AH. Combatting Secondary Injury From Intracerebral Hemorrhage With Supplemental Antioxidant Therapy. Stroke. 2021;52(4):1182-1184.
[14] CHEN-ROETLING J, LU X, REGAN RF. Targeting heme oxygenase after intracerebral hemorrhage. Ther Targets Neurol Dis. 2015;2(1):474.
[15] YIN XP, WU D, ZHOU J, et al. Heme oxygenase 1 plays role of neuron-protection by regulating Nrf2-ARE signaling post intracerebral hemorrhage. Int J Clin Exp Pathol. 2015;8(9):10156-10163.
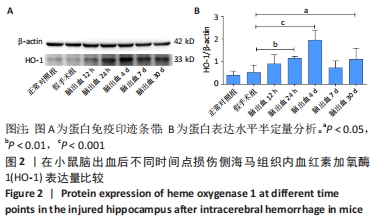
[16] WANG G, YANG Q, LI G, et al. Time course of heme oxygenase-1 and oxidative stress after experimental intracerebral hemorrhage. Acta Neurochir (Wien). 2011;153(2):319-325.
[17] FAN X, MU L. The role of heme oxygenase-1 (HO-1) in the regulation of inflammatory reaction, neuronal cell proliferation and apoptosis in rats after intracerebral hemorrhage (ICH). Neuropsychiatr Dis Treat. 2017; 13:77-85.
[18] XIAN P, HEI Y, WANG R, et al. Mesenchymal stem cell-derived exosomes as a nanotherapeutic agent for amelioration of inflammation-induced astrocyte alterations in mice. Theranostics. 2019;9(20):5956-5975.
[19] 朱东京,鲜盼盼,王甜,等.间充质干细胞外泌体对海马星形胶质细胞活化的抑制作用研究[J].中华细胞与干细胞杂志(电子版), 2021,11(2):99-105.
[20] ZHANG Y, WANG WT, GONG CR, et al. Combination of olfactory ensheathing cells and human umbilical cord mesenchymal stem cell-derived exosomes promotes sciatic nerve regeneration. Neural Regen Res. 2020; 15(10): 1903-1911.
[21] 陈思铭,胡加伟,李丽丽,等. 两种方法提取人脐带间充质干细胞三维培养生物学特性的比较[J].中国组织工程研究,2022,26(19): 2997-3003.
[22] 王涵,刘卫平,龙乾发,等.脐血间充质干细胞外泌体对APP/PS1小鼠海马神经元的保护作用及其机制[J].临床神经外科杂志,2021, 18(3):299-304.
[23] JIN P, DENG S, SHERCHAN P, et al. Neurokinin Receptor 1 (NK1R) Antagonist Aprepitant Enhances Hematoma Clearance by Regulating Microglial Polarization via PKC/p38MAPK/NFκB Pathway After Experimental Intracerebral Hemorrhage in Mice. Neurotherapeutics. 2021;18(3):1922-1938.
[24] RYNKOWSKI MA, KIM GH, KOMOTAR RJ, et al. A mouse model of intracerebral hemorrhage using autologous blood infusion. Nat Protoc. 2008;3(1):122-128.
[25] KARUPPAGOUNDER SS, ALIM I, KHIM SJ, et al. Therapeutic targeting of oxygen-sensing prolyl hydroxylases abrogates ATF4-dependent neuronal death and improves outcomes after brain hemorrhage in several rodent models. Sci Transl Med. 2016;8(328):328ra29.
[26] REGAN RF, PANTER SS. Neurotoxicity of hemoglobin in cortical cell culture. Neurosci Lett. 1993;153(2):219-222.
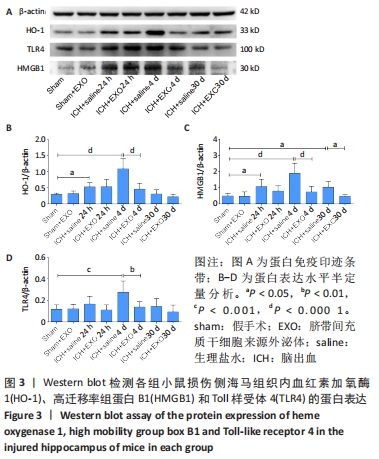
[27] WANG T, JIAN Z, BASKYS A, et al. MSC-derived exosomes protect against oxidative stress-induced skin injury via adaptive regulation of the NRF2 defense system. Biomaterials. 2020;257:120264.
[28] NAKANO M, FUJIMIYA M. Potential effects of mesenchymal stem cell derived extracellular vesicles and exosomal miRNAs in neurological disorders. Neural Regen Res. 2021;16(12):2359-2366.
[29] ZHENG H, ZHANG B, CHHATBAR PY, et al. Mesenchymal Stem Cell Therapy in Stroke: A Systematic Review of Literature in Pre-Clinical and Clinical Research. Cell Transplant. 2018;27(12):1723-1730.
[30] HAN Y, SEYFRIED D, MENG Y, et al. Multipotent mesenchymal stromal cell-derived exosomes improve functional recovery after experimental intracerebral hemorrhage in the rat. J Neurosurg. 2018;131(1):290-300.
[31] LI M, LI X, WANG D, et al. Inhibition of exosome release augments neuroinflammation following intracerebral hemorrhage. FASEB J. 2021; 35(6):e21617.
[32] SCHIPPER HM, SONG W, TAVITIAN A, et al. The sinister face of heme oxygenase-1 in brain aging and disease. Prog Neurobiol. 2019;172:40-70.
[33] KANNO H, OZAWA H, DOHI Y, et al. Genetic ablation of transcription repressor Bach1 reduces neural tissue damage and improves locomotor function after spinal cord injury in mice. J Neurotrauma. 2009;26(1): 31-39.
[34] WEI CC, KONG YY, LI GQ, et al. Nicotinamide mononucleotide attenuates brain injury after intracerebral hemorrhage by activating Nrf2/HO-1 signaling pathway. Sci Rep. 2017;7(1):717.
[35] LIAO YF, ZHU W, LI DP, et al. Heme oxygenase-1 and gut ischemia/reperfusion injury: A short review. World J Gastroenterol. 2013; 19(23): 3555-3561.
[36] ZHANG ZF, LIU SM, XIU BH. Research progression about role of hemeoxygenase-1 during brain injuries. Prog Mod Biomed. 2011;11(5): 961-963.
[37] LIU XH, WANG XL, XIN H, et al. Induction of Heme Oxygenase-1 by Sodium 9-Hydroxyltanshinone IIA Sulfonate Derivative Contributes to Inhibit LPS-Mediated Inflammatory Response in Macrophages. Cell Physiol Biochem. 2015;36(4):1316-1330.
[38] LI Y, JIANG Q, WANG L. Appetite Regulation of TLR4-Induced Inflammatory Signaling. Front Endocrinol (Lausanne). 2021;12:777997.
[39] RANZATO E, MARTINOTTI S, PEDRAZZI M, et al. High mobility group box protein-1 in wound repair. Cells. 2012;1(4):699-710.
[40] XIONG L, SUN L, ZHANG Y, et al. Exosomes from Bone Marrow Mesenchymal Stem Cells Can Alleviate Early Brain Injury After Subarachnoid Hemorrhage Through miRNA129-5p-HMGB1 Pathway. Stem Cells Dev. 2020;29(4):212-221.
|