[1] CLYNES MA, HARVEY NC, CURTIS EM, et al. The epidemiology of osteoporosis. Br Med Bull. 2020;133(1):105-117.
[2] 邱贵兴, 裴福兴, 胡侦明, 等. 中国骨质疏松性骨折诊疗指南(骨质疏松性骨折诊断及治疗原则) [J]. 中华骨与关节外科杂志,2015, 8(5):371-374.
[3] FONSECA H, MOREIRA-GONçALVES D, CORIOLANO H J, et al. Bone quality: the determinants of bone strength and fragility. Sports Med. 2014;44(1):37-53.
[4] 丁悦, 张嘉, 岳华, 等. 骨质疏松性椎体压缩性骨折诊疗与管理专家共识 [J]. 中华骨质疏松和骨矿盐疾病杂志,2018,11(5):425-437.
[5] FERREIRA ML, MARCH L. Vertebral fragility fractures - How to treat them? Best Pract Res Clin Rheumatol. 2019;33(2):227-235.
[6] 印平, 马远征, 马迅, 等. 骨质疏松性椎体压缩性骨折的治疗指南 [J]. 中国骨质疏松杂志,2015,21(6):643-648.
[7] ESSES S I, MCGUIRE R, JENKINS J, et al. American Academy of Orthopaedic Surgeons clinical practice guideline on: the treatment of osteoporotic spinal compression fractures. J Bone Joint Surg Am. 2011; 93(20):1934-1936.
[8] MCGUIRE R. AAOS Clinical Practice Guideline: the Treatment of Symptomatic Osteoporotic Spinal Compression Fractures. J Am Acad Orthop Surg. 2011;19(3):183-184.
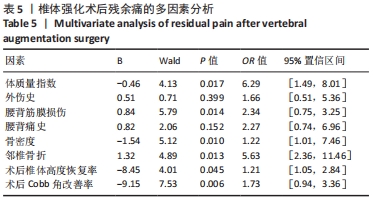
[9] 梁冬波, 李剑峰, 王力平. 经皮穿刺椎体成形术术后残余腰痛的相关因素分析[J]. 微创医学,2017,12(4):479-482.
[10] 杨朝林, 刘日新, 袁国奇, 等. 骨质疏松压缩骨折经皮椎体成形术伤椎高度变化的MSCT与临床疗效的评价[J]. 中国CT和MRI杂志, 2015,13(4):107-110.
[11] YIMIN Y, ZHIWEI R, WEI M, et al. Current status of percutaneous vertebroplasty and percutaneous kyphoplasty--a review. Med Sci Monit. 2013;19:826-836.
[12] WONG W, MATHIS JM. Vertebroplasty and kyphoplasty: techniques for avoiding complications and pitfalls. Neurosurg Focus. 2005;18(3):e2.
[13] DERAMOND H, WRIGHT NT, BELKOFF SM. Temperature elevation caused by bone cement polymerization during vertebroplasty. Bone. 1999;25(2 Suppl):17s-21s.
[14] BAROUD G, BOHNER M. Biomechanical impact of vertebroplasty. Postoperative biomechanics of vertebroplasty. Joint Bone Spine. 2006; 73(2):144-150.
[15] 行勇刚, 张贵林, 田伟, 等. 骨质疏松性椎体压缩骨折患者术后腰背疼痛原因分析[J]. 中华医学杂志,2015,95(29):2342-2345.
[16] YANG JS, LIU JJ, CHU L, et al. Causes of Residual Back Pain at Early Stage After Percutaneous Vertebroplasty: A Retrospective Analysis of 1,316 Cases. Pain Physician. 2019;22(5):E495-e503.
[17] LIU WG, HE SC, DENG G, et al. Risk factors for new vertebral fractures after percutaneous vertebroplasty in patients with osteoporosis: a prospective study. J Vasc Interv Radiol. 2012;23(9):1143-1149.
[18] 包拥政, 祝周兴, 冯云升, 等. 低弹性模量骨水泥对骨质疏松压缩性骨折椎体及邻近椎体应力的影响:三维有限元分析[J]. 中国组织工程研究,2016,20(16):2285-2293.
[19] BOGER A, HEINI P, WINDOLF M, et al. Adjacent vertebral failure after vertebroplasty: a biomechanical study of low-modulus PMMA cement. Eur Spine J. 2007;16(12):2118-2125.
[20] YI X, LU H, TIAN F, et al. Recompression in new levels after percutaneous vertebroplasty and kyphoplasty compared with conservative treatment. Arch Orthop Trauma Surg. 2014;134(1):21-30.
[21] LI H L, SHEN Y, TAN L H, et al. Relationship between bone mineral density and fragility fracture risk: a case-control study in Changsha, China. BMC Musculoskelet Disord. 2021;22(1):728.
[22] 沈煜, 冯明利, 徐军, 等. 老年骨质疏松性椎体压缩性骨折部位和腰椎骨密度对下腰部疼痛的影响 [J]. 中华医学杂志,2016,96(23): 1818-1820.
[23] EIDTMANN H, DE BOER R, BUNDRED N, et al. Efficacy of zoledronic acid in postmenopausal women with early breast cancer receiving adjuvant letrozole: 36-month results of the ZO-FAST Study. Ann Oncol. 2010; 21(11):2188-2194.
[24] LEE DG, PARK CK, PARK CJ, et al. Analysis of Risk Factors Causing New Symptomatic Vertebral Compression Fractures After Percutaneous Vertebroplasty for Painful Osteoporotic Vertebral Compression Fractures: A 4-year Follow-up. J Spinal Disord Tech. 2015;28(10):E578-583.
[25] HAAS AV, CONG E, SIMPSON CA, et al. Associations among circulating colony-stimulating factor-1, estrogen, and bone mineral density in postmenopausal women: results from a randomized placebo-controlled trial. Menopause. 2018;25(2):197-201.
[26] VILLAREAL DT, RUPICH RC, PACIFICI R, et al. Effect of estrogen and calcitonin on vertebral bone density and vertebral height in osteoporotic women. Osteoporos Int. 1992;2(2):70-73.
[27] YAN Y, XU R, ZOU T. Is thoracolumbar fascia injury the cause of residual back pain after percutaneous vertebroplasty? A prospective cohort study. Osteoporos Int. 2015;26(3):1119-1124.
[28] GUO Z, YANG J, ZHENG Y, et al. Thoracolumbar fascia injury associated with residual back pain after percutaneous vertebroplasty: a compelling study. Osteoporos Int. 2015;26(11):2709-2710.
[29] LIEBERMAN IH, DUDENEY S, REINHARDT MK, et al. Initial outcome and efficacy of “kyphoplasty” in the treatment of painful osteoporotic vertebral compression fractures. Spine (Phila Pa 1976). 2001;26(14): 1631-1638.
[30] LINDSAY R, SILVERMAN SL, COOPER C, et al. Risk of new vertebral fracture in the year following a fracture. Jama. 2001;285(3):320-323.
[31] 陈激光. 胸腰椎压缩性骨折患者PKP术后残余痛的危险因素分析[D].上海:中国人民解放军海军军医大学,2021.
[32] 赵龙, 王剑, 韩正才, 等. 椎体成形术后残余后凸畸形的有限元分析[J].中国矫形外科杂志,2020,28(22):2082-2086.
[33] 张相伟, 孙建民, 崔新刚, 等. 骨质疏松椎体压缩性骨折患者脊柱矢状面的失平衡[J]. 中国组织工程研究,2014,18(26):4224-4228.
[34] YANG S, LIU Y, YANG H, et al. Risk factors and correlation of secondary adjacent vertebral compression fracture in percutaneous kyphoplasty. Int J Surg. 2016;36(Pt A):138-142.
[35] LIN WC, CHENG TT, LEE YC, et al. New vertebral osteoporotic compression fractures after percutaneous vertebroplasty: retrospective analysis of risk factors. J Vasc Interv Radiol. 2008;19(2 Pt 1):225-231.
|