中国组织工程研究 ›› 2020, Vol. 24 ›› Issue (5): 741-746.doi: 10.3969/j.issn.2095-4344.2401
• 组织构建临床实践 clinical practice in tissue construction • 上一篇 下一篇
合并移行椎腰椎间盘突出症患者腰骶神经根支配区的变化
王 欣,王大巍,孙亦强,赵子豪,窦永峰,胡 鹏,耿晓鹏
- 滨州医学院附属医院,山东省滨州市 256603
Changes of lumbosacral nerve roots innervation in lumbar disc herniation patients with transitional vertebrae
Wang Xin, Wang Dawei, Sun Yiqiang, Zhao Zihao, Dou Yongfeng, Hu Peng, Geng Xiaopeng
- Affiliated Hospital of Binzhou Medical University, Binzhou 256603, Shandong Province, China
摘要:
文题释义:
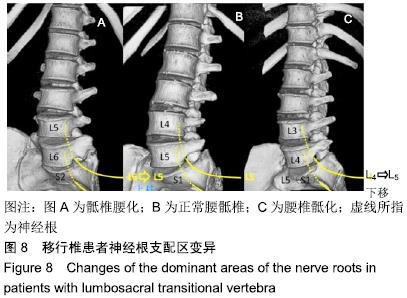
移行椎:移行椎系脊柱先天性发育变异,各段脊柱交界处互有移行现象,出现部分或全部具有邻近脊椎骨的形态结构,整个脊椎骨的总数不变,而各段脊椎骨的数目互有增减,称之为移行椎,多发生于腰骶段。脊柱全长X射线可明确是否存在移行椎。
腰骶移行椎(lumbosacral transitional vertebrae,LSTV):腰骶移行椎分为腰椎骶化(sacralization,SZ)和骶椎腰化(lumbarization,LZ)。目前腰骶移行椎以Castellvi的分类方法最为常用,主要根据横突形态及其与骶骨、髂骨是否融合或形成假关节而分为4型,每型再根据单、双侧分为A、B二个亚型。Santavirta则根据横突与骶骨/髂骨形成假关节或融合分为5个类型。
背景:腰骶移行椎是一种常见的先天脊柱畸形,国内外学者均有报道移行椎患者的腰骶神经根支配区可能会发生改变,但并未系统阐述其支配区的变化以及该种改变对腰椎间盘突出症患者手术的指导意义。
目的:探讨当存在腰骶移行椎时,腰骶神经根的运动和感觉支配区发生改变的可能性。
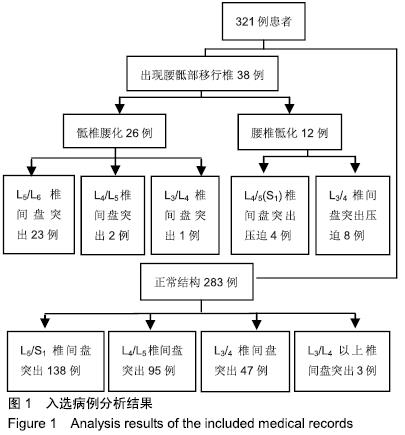
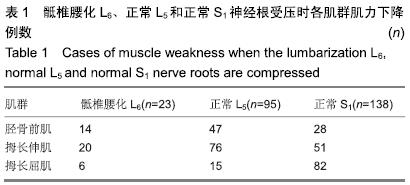
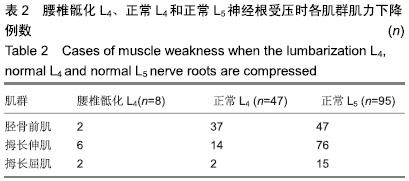
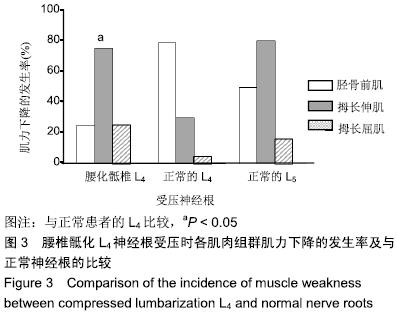
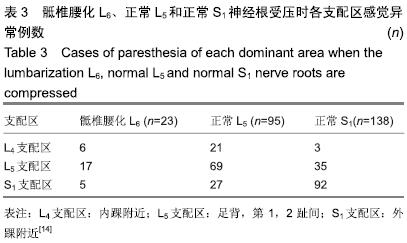
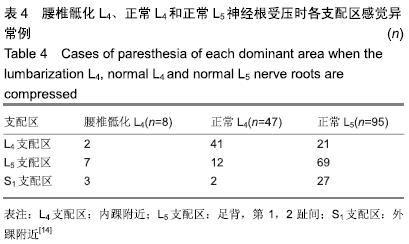
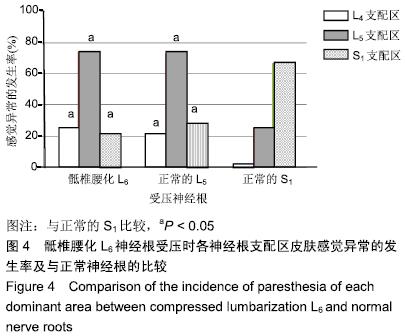
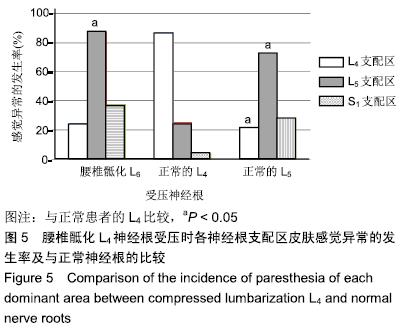
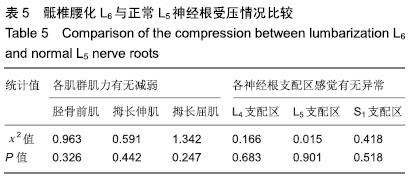
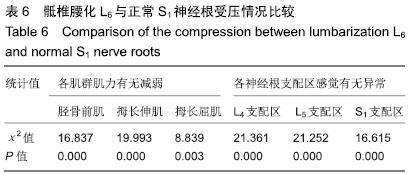
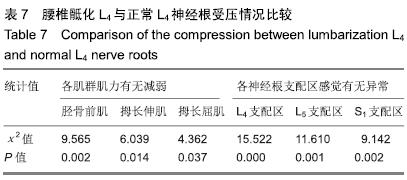
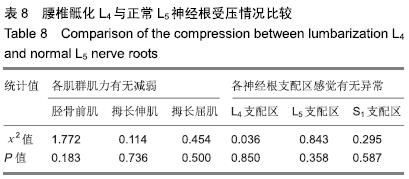
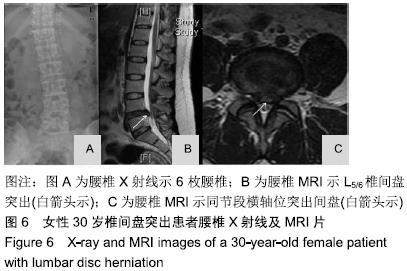
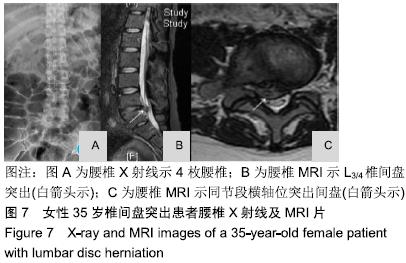
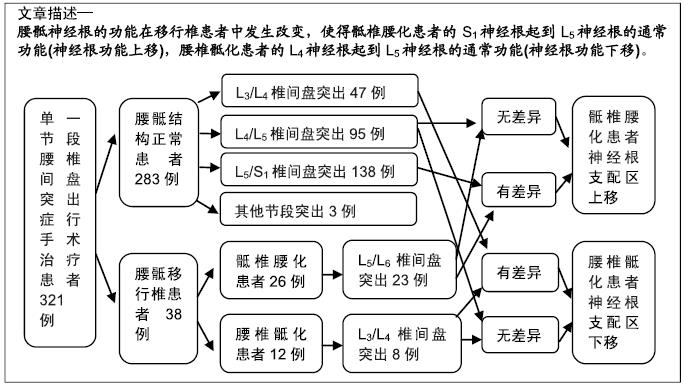
方法:研究方案的实施符合滨州医学院附属医院对研究的相关伦理要求,参与试验的患病个体及其家属对试验过程完全知情同意。回顾分析321例单一节段腰椎间盘突出症行手术治疗患者的病历资料。其中38例(11.8%)存在腰骶移行椎,包括骶椎腰化26例、腰椎骶化12例。26例骶椎腰化患者中,23例为L5/S1(L6)椎间盘突出,压迫S1(L6)神经根。12例腰椎骶化患者中,8例为L3/4椎间盘突出,压迫L4神经根。在283例正常结构的患者中,138例患者L5/S1椎间盘突出压迫S1神经根,95例患者L4/L5椎间盘突出压迫L5神经根,47例患者L3/L4椎间盘突出压迫L4神经根。比较术前骶椎腰化患者S1神经根受压的症状、腰椎骶化患者L4神经根受压的症状与正常腰骶椎患者L4、L5或S1神经根受压的症状。
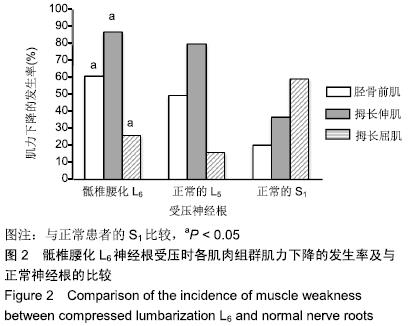
结果与结论:①S1神经根受压所致运动功能减退的分布在骶椎腰化患者组和正常组之间差异有显著性意义 (P < 0.05);②L4神经根受压所致运动功能减退的分布在腰椎骶化患者组和正常组之间差异有显著性意义(P < 0.05);③骶椎腰化患者S1神经根受压所致的运动功能减退与正常状态下L5神经根受压所致的运动功能减退相似;而腰椎骶化患者L4神经根受压所致的运动功能减退与正常状态下L5神经根受压所致的运动功能减退相似;皮肤感觉异常的分析也显示了相似的结果;④结果说明,腰骶神经根的功能在移行椎患者中发生改变,使得骶椎腰化患者的S1神经根起到L5神经根的通常功能(神经根功能上移),腰椎骶化患者的L4神经根起到L5神经根的通常功能(神经根功能下移)。
ORCID: 0000-0001-5041-2060(王欣)
中国组织工程研究杂志出版内容重点:组织构建;骨细胞;软骨细胞;细胞培养;成纤维细胞;血管内皮细胞;骨质疏松;组织工程
中图分类号: