中国组织工程研究 ›› 2016, Vol. 20 ›› Issue (5): 628-634.doi: 10.3969/j.issn.2095-4344.2016.05.004
• 周围神经损伤动物模型 Animal models of peripheral nerve injury • 上一篇 下一篇
SD大鼠脊髓损伤后微环境的模拟实验
贾叙锋,龙 苗,戢 勇,黄光平,周 玉,张方德,冯大雄
- 1简阳市人民医院骨科,四川省简阳市 641400;2泸州医学院附属医院脊柱外科,四川省泸州市 646000
Simulation of microenviroment after spinal cord injury in Sprague-Dawley rats
Jia Xu-feng1, 2, Long Miao1, Ji Yong1, Huang Guang-ping1, Zhou Yu1, Zhang Fang-de1, Feng Da-xiong2
- 1Department of Orthopedics, People’s Hospital of Jianyang City, Jianyang 641400, Sichuan Province, China; 2Department of Spine Surgery, Affiliated Hospital of Luzhou Medical College, Luzhou 646000, Sichuan Province, China
摘要:
文章快速阅读:
.jpg)
文题释义:
脊髓损伤微环境改变:脊髓损伤后,早期病理变化体征为局部的水肿、结构破坏、神经元坏死以及对附件组织产生压迫加重了脊髓组织缺血损害等。在直接暴力损伤后出现的病理生理变化以及各种因素同样在脊髓损伤中起着极为重要的作用,如肿瘤坏死因子α、白细胞介素6等各种致炎细胞因子、炎性因子、炎性细胞活化等促使胶质细胞的大量增殖,并在病灶处形成致密的瘢痕组织,从而阻挡了神经纤维的延伸。
Allen’s脊髓损伤模型:采用改良Allen’s模型以改变重物下落的高度、致伤力,从而复制出不同类型、不同损伤程度的脊髓损伤后微环境。动物所受的致伤能量常以冲击棒质量(g)乘以坠落高度(cm)即克厘米势能(gcf)表示,致伤势能为20 g×5 cm,20 g×10 cm,20 g×15 cm,可模拟SD大鼠轻、中、重度脊髓损伤模型的微环境。
背景:通过制作SD大鼠的轻、中、重度脊髓损伤模型,使之符合基础实验研究的脊髓损伤类型,可进一步了解SD大鼠脊髓损伤后的微环境变化,为临床治疗提供帮助。
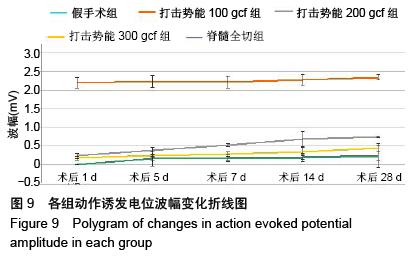
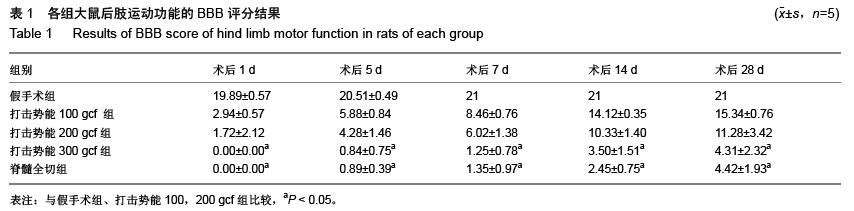
目的:模拟SD大鼠脊髓损伤后微环境,观察不同致伤势能的Allen’s模型和脊髓全切模型SD大鼠脊髓损伤后不同时间点的神经功能、病理以及运动诱发电位的变化。
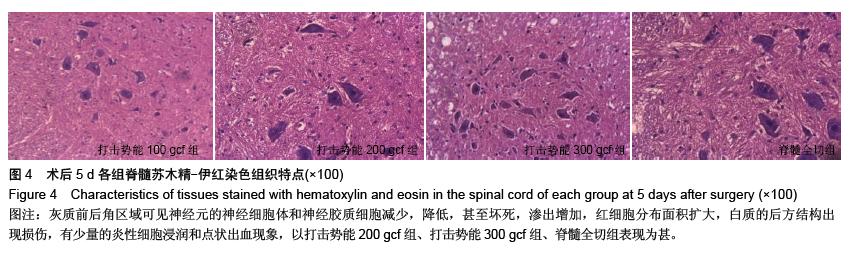
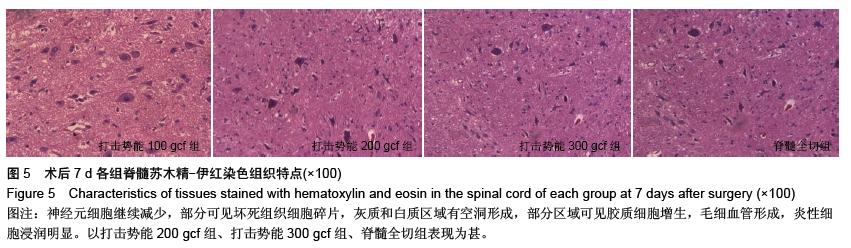
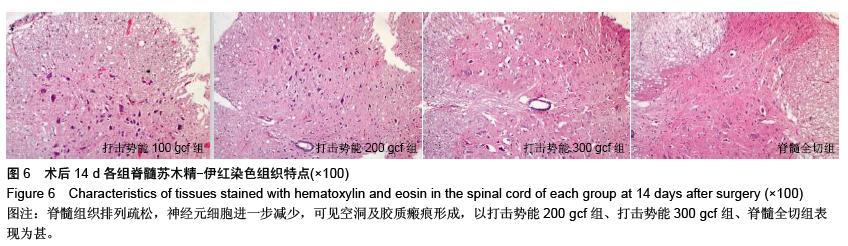
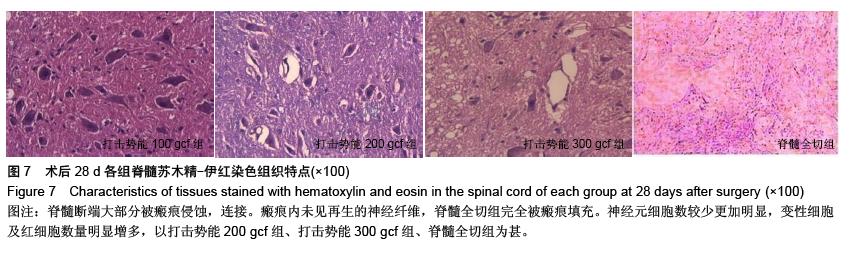
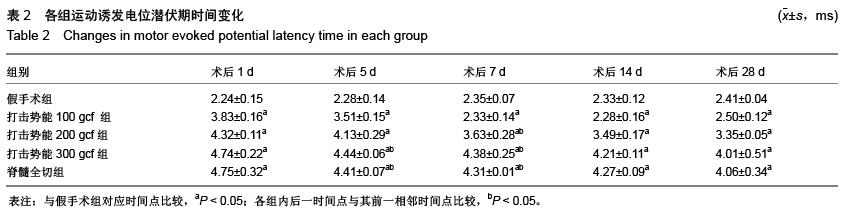
方法:选择125只成年雌性健康SD大鼠,随机分为假手术组、打击势能100 gcf组(20 g×5 cm)、打击势能200 gcf组(20 g×10 cm)、打击势能300 gcf组(20 g×15 cm)、脊髓全切组,每组25只,在制模成功后第1,5,7,14,28天采用BBB后肢运动功能评分、运动诱发电位监测、病理切片鉴定,观察各组大鼠脊髓损伤程度。
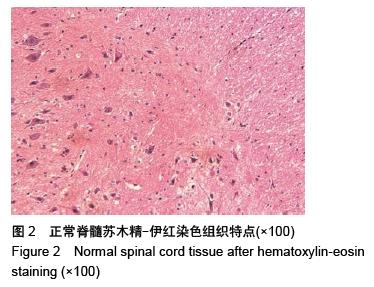
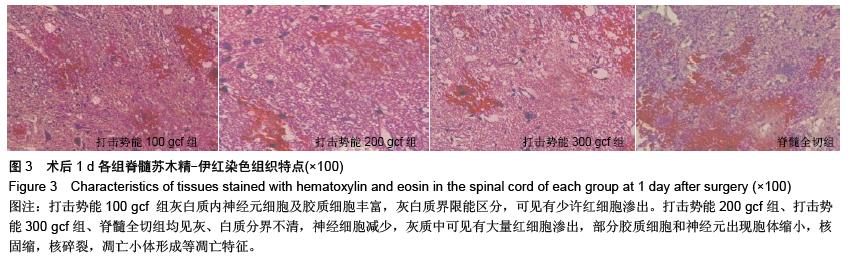
结果与结论:①整个实验中SD大鼠死亡24只,脊髓全切组的死亡率和并发症最高,每组的BBB评分均降低,随着时间延长BBB评分逐渐增高。各手术组与假手术组在对应时间点比较,差异有显著性意义(P < 0.05),打击势能300 gcf组和脊髓全切组在对应时间点比较,差异无显著性意义(P > 0.05)。②各手术组在伤后1 d病灶处出现炎性细胞浸润,神经元细胞肿胀明显,随着时间推移,神经细胞减少;伤后28 d发现大量星形胶质细胞增生,瘢痕及脊髓空洞形成,打击势能300 gcf组、脊髓全切组明显重于打击势能100 gcf 组、打击势能200 gcf组。③各手术组与假手术组的波幅及潜伏期在对应时间点比较,差异有显著性意义(P < 0.05);打击势能300 gcf组和脊髓全切组在对应时间点比较,差异无显著性意义(P > 0.05)。结果表明致伤势能为 20 g×5 cm,20 g×10 cm,20 g×15 cm,可模拟SD大鼠轻、中、重度脊髓损伤模型的微环境;不同势能的改良Allen’s模型较脊髓全切模型并发症低,更符合基础研究。
ORCID:0000-0001-7648-8821(冯大雄)
.jpg)
.jpg)
.jpg)