[1] BAILEY DK. The normal cervical spine in infants and children. Radiology. 1952;59(5):712-719.
[2] CALVY TM, SEGALL HD, GILLES FH, et al. CT anatomy of the craniovertebral junction in infants and children. AJNR Am J Neuroradiol. 1987;8(3):489-494.
[3] LEE HJ, KIM JT, SHIN MH, et al. The ossification pattern in paediatric occipito-cervical spine: is it possible to estimate real age? Clin Radiol. 2015;70(8):835-843.
[4] 王华伟. 寰椎枕化寰椎侧块形态解剖学研究及有关致病机制的生物力学分析[D].北京:中国人民解放军医学院,2019.
[5] 冯会梅,王星,张少杰,等.有限元法分析0-6岁儿童枕寰枢复合体发育及其生物力学的变化特征[J].中国组织工程研究,2018, 22(23):3710-3715.
[6] 于永涛,张少杰,刘颖,等.学龄期儿童寰枢椎数字化三维形态测量研究[J].中国脊柱脊髓杂志,2017,27(1):69-74.
[7] AVELLINO AM, MANN FA, GRADY MS, et al. The misdiagnosis of acute cervical spine injuries and fractures in infants and children: the 12-year experience of a level I pediatric and adult trauma center. Child’s Nervous System. 2005;21(2):122-112.
[8] 田忠祥,赵永峰,王丹,等.多层螺旋CT图像后处理技术诊断寰枢椎骨折与脱位价值探讨[J].医学影像学杂志,2018,28(6):1039-1040.
[9] JENKINS S, BORDES S, ALY I, et al. Internal Morphology of the Odontoid Process: Anatomic and Imaging Study with Application to C2 Fractures. World Neurosurg. 2019;127:e1120-e1126.
[10] PIATT JH JR, GRISSOM LE. Developmental anatomy of the atlas and axis in childhood by computed tomography. J Neurosurg Pediatr. 2011; 8(3):235-243.
[11] 蓝佐珍,钱雅楠,池金澄,等.CT研究寰椎正常发育与变异[J].中国组织工程研究,2023,27(22):3573-3578.
[12] KARWACKI GM, SCHNEIDER JF. Normal ossification patterns of atlas and axis: a CT study. AJNR Am J Neuroradiol. 2012;33(10):1882-1887.
[13] BAUMGART M, WISNIEWSKI M, GRZONKOWSKA M, et al. Morphometric study of the neural ossification centers of the atlas and axis in the human fetus. Surg Radiol Anat. 2016;38(10):1205-1215.
[14] 曲星月.儿童齿状突基底部骨化中心数字解剖及组织形态学研究[D].呼和浩特:内蒙古医科大学,2022.
[15] 赵慧.正常胎儿脊柱发育的标本磁共振研究[D].济南:山东大学, 2015.
[16] BAUMGART M, WIŚNIEWSKI M, GRZONKOWSKA M, et al. Digital image analysis of ossification centers in the axial dens and body in the human fetus. Surg Radiol Anat. 2016;38(10):1195-1203.
[17] SELB J, OGDEN TM, DUBB J, et al. Comparison of a layered slab and an atlas head model forMonte Carlo fitting of time-domain near-infrared spectroscopy data of the adult head. J Biomed Opt. 2014;19(1):16010.
[18] AKOBO S, RIZK E, LOUKAS M, et al. The odontoid process: a comprehensive review of its anatomy, embryology, and variations. Childs Nerv Syst. 2015;31(11):2025-2034.
[19] JAGANNATHAN J, DUMONT AS, PREVEDELLO DM, et al. Cervicalspine injuries in pediatric athletes: mechanisms and management. Neurosurg Focus. 2006; 21(4): E6.
[20] MCALLISTER AS, NAGARAJ U, RADHAKRISHNAN R. Emergent Imaging of Pediatric Cervical Spine Trauma. Radiographics. 2019;39(4):1126-1142.
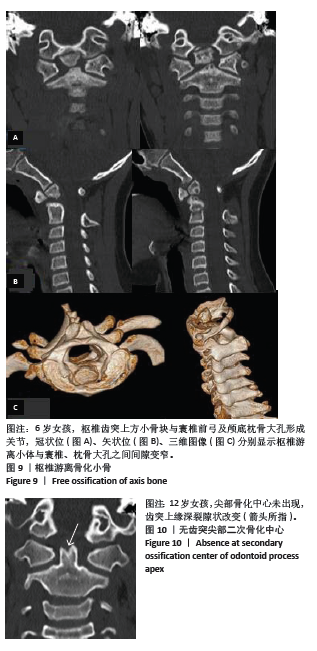
[21] 胡贤铧,胡云地,曹志刚,等.齿突游离小骨MSCT和MRI表现特点和临床诊断(附15例报道)[J].医学影像学杂志,2017,27(12): 2276-2279.
[22] WANG Q, DONG S, WANG F. Os odontoideum: diagnosis and role of imaging. 2020;42(2):155-160.
[23] ABUAMARA S, DACHER JN, LECHEVALLIER J. Posterior arch bifocal fracture of the atlas vertebra: a variant of Jefferson fracture. J Pediatr Orthop B. 2001;10(3):201-204.
[24] WANG S, WANG C. Familial dystopic os odontoideum: a report of three cases. J Bone Joint Surg Am. 2011;93(9):e44.
[25] 张正丰,周跃,王建,等.游离齿突伴寰枢椎不稳引起的进行性脊髓损伤[J].中国矫形外科杂志,2010,18(16):1398-1400.
[26] CHO S, SHLOBIN NA, DAHDALEH NS. Os odontoideum: A comprehensive review. J Craniovertebr Junction Spine. 2022;13(3):256-264.
[27] 王立勋, 姜建元, 吕飞舟, 等.不稳定性齿突游离小骨的诊断及治疗:26例患者临床分析[J].脊柱外科杂志,2014,12(3):152-155.
[28] UTHMAN A, SALMAN B, SHAMS ALDEEN H, et al. Morphometric analysis of odontoid process among Arab population: a retrospective cone beam CT study. Peer J. 2023;23:11:e15411.
[29] 徐雪彬.数字儿童颈部薄层断面与影像解剖对比及其三维可视化应用研究[D].呼和浩特:内蒙古医科大学,2021.
[30] JOHNSON KT, AL-HOLOU WN, ANDERSON RC, et al. Morphometric analysis of the developing pediatric cervical spine. J Neurosurg Pediatr. 2016;18(3):377-389
[31] 丁昌懋. 颅颈交界区畸形综合影像学研究[D].郑州:郑州大学,2016.
[32] 孙岩,谭明生.发育性寰椎管狭窄症的临床研究进展[J].中国矫形外科杂志,2020,28(15):1404-1407
[33] WU L, JIN Y, WANG XY, et al. Two novel parameters to evaluate the influence of the age and gender on the anatomic relationship of the atlas and axis in children no more than 8 years old: imaging study. Neuroradiology. 2019;61(12):1407-1414.
[34] ELLIOTT S. The odontoid process in children--is it hypoplastic? Clin Radiol. 1988;39(4):391-393.
[35] LEE HJ, KIM JT, SHIN MH, et al. Quantification of pediatric cervical spine growth at the cranio-vertebral junctio.J Korean Neurosurg Soc. 2015;57(4):276-282.
[36] HA BJ, WON YD, RYU JI, et al. Relationship between the atlantodental interval and T1 slope after atlantoaxial fusion in patients with rheumatoid arthritis. BMC Surg. 2020;20(1):269.
[37] ÖĞÜT E, ŞEKERCI R, ŞEN H, et al. Anatomo-radiological importance and the incidence of os odontoideum in Turkish subjects: a retrospective study. Surg Radiol Anat. 2020;42(6):701-710.
|