中国组织工程研究 ›› 2019, Vol. 23 ›› Issue (33): 5404-5412.doi: 10.3969/j.issn.2095-4344.1839
• 干细胞综述 stem cell review • 上一篇
骨形态发生蛋白9诱导成骨机制及其临床应用
朱正清,陈香润,贾方腾,黄岚峰
- 吉林大学第二医院骨科,吉林省长春市 130041
-
修回日期:2019-06-15出版日期:2019-11-28发布日期:2019-11-28 -
通讯作者:黄岚峰,主任医师,教授,硕士生导师,吉林大学第二医院骨科,吉林省长春市 130041 -
作者简介:朱正清,男,1994年生,汉族,吉林大学第二医院骨科在读硕士,主要从事骨组织工程细胞因子及骨缺损的临床治疗研究。 -
基金资助:吉林省财政厅卫生专项项目(201817294302),项目负责人:黄岚峰
Bone morphogenetic protein 9: osteogenic induction mechanism and clinical application
Zhu Zhengqing, Chen Xiangrun, Jia Fangteng, Huang Lanfeng
- Department of Orthopedics, Second Hospital of Jilin University, Changchun 130041, Jilin Province, China
-
Revised:2019-06-15Online:2019-11-28Published:2019-11-28 -
Contact:Huang Lanfeng, Chief physician, Professor, Master’s supervisor, Department of Orthopedics, Second Hospital of Jilin University, Changchun 130041, Jilin Province, China -
About author:Zhu Zhengqing, Master candidate, Department of Orthopedics, Second Hospital of Jilin University, Changchun 130041, Jilin Province, China -
Supported by:the Health Special Project of Jilin Provincial Finance Department, No. 201817294302 (to HLF)
摘要:
文章快速阅读:
.jpg)
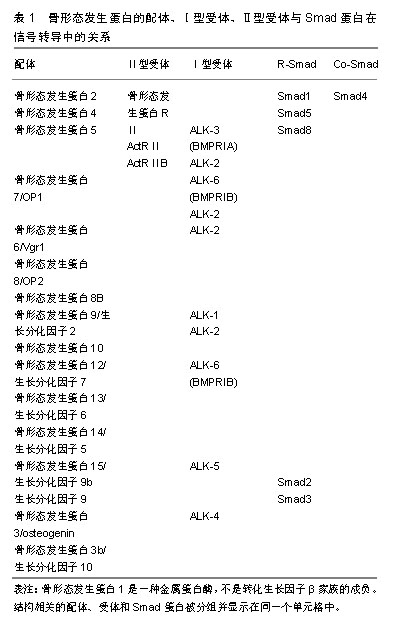
文题释义: 骨形态发生蛋白9(bone morphogenetic protein,BMP9):也被称为生长分化因子2,其基因最初是从胎鼠肝脏cDNA文库中分离出来的。骨形态发生蛋白9参与调节细胞的增殖、分化和凋亡,其不仅能调节细胞内皮功能和促进血管生成,还能诱导成骨,在脊椎动物和无脊椎动物的各种组织的发育和维持中起着关键的作用。研究表明骨形态发生蛋白9与能够诱导成骨的骨形态发生蛋白2和骨形态发生蛋白7相比,具有更强的成骨诱导能力。 WNT通路:在骨骼发育和成骨细胞分化中起着重要作用,是调节骨骼系统发育的另一个重要信号通路。其可能参与调节骨髓间充质干细胞中骨形态发生蛋白9诱导的成骨作用。WNT通路分为经典WNT通路和非经典WNT通路。
中图分类号:
引用本文
朱正清,陈香润,贾方腾,黄岚峰. 骨形态发生蛋白9诱导成骨机制及其临床应用[J]. 中国组织工程研究, 2019, 23(33): 5404-5412.
Zhu Zhengqing, Chen Xiangrun, Jia Fangteng, Huang Lanfeng. Bone morphogenetic protein 9: osteogenic induction mechanism and clinical application[J]. Chinese Journal of Tissue Engineering Research, 2019, 23(33): 5404-5412.
| [1]Hao Z, Song Z, Huang J, et al. The scaffold microenvironment for stem cell based bone tissue engineering. Biomater Sci.2017;5(8): 1382-1392.[2]汤显能,陈跃平,章晓云.骨与软骨组织工程中骨形态发生蛋白的特征与临床应用[J].中国组织工程研究,2019,23(4):591-596.[3]Siddiqui JA, Partridge NC. Physiological Bone Remodeling: Systemic Regulation and Growth Factor Involvement.Physiology (Bethesda). 2016;31(3):233[4]Thoma DS, Lim HC, Sapata VM, et al. Recombinant bone morphogenetic protein-2 and platelet-derived growth factor-BB for localized bone regeneration. Histologic and radiographic outcomes of a rabbit study.Clin Oral Implants Res. 2017;28(11): e236-e243.[5]Lindsey RC, Mohan S. Skeletal Effects of Growth Hormone and Insulin-like Growth Factor-I Therapy. Mol Cell Endocrinol. 2016; 432:44-55.[6]Lamplot JD, Qin J, Nan G, et al. BMP9 signaling in stem cell differentiation and osteogenesis. Am J Stem Cells.2013;2(1):1-21.[7]Reddi AH, Reddi A. Bone morphogenetic proteins (BMPs): from morphogens to metabologens. Cytokine Growth Factor Rev.2009; 20(5-6):341-342.[8]Fujioka-Kobayashi M, Schaller B, Saulacic N,et al. Absorbable collagen sponges loaded with recombinant bone morphogenetic protein 9 induces greater osteoblast differentiation when compared to bone morphogenetic protein 2. Clin Exp Dent Res. 2017; 3(1): 32-40.[9]Fujioka-Kobayashi M, Abd El Raouf M, Saulacic N, et al. Superior bone-inducing potential of rhBMP9 compared to rhBMP2. J Biomed Mater Res A. 2018;106(6):1561-1574.[10]Kang Q, Song WX, Luo Q, et al. A comprehensive analysis of the dual roles of BMPs in regulating adipogenic and osteogenic differentiation of mesenchymal progenitor cells. Stem Cells Dev. 2009;18(4):545-559.[11]Kang Q, Sun MH, Cheng H, et al. Characterization of the distinct orthotopic bone-forming activity of 14 BMPs using recombinant adenovirus-mediated gene delivery. Gene Ther. 2004; 11(17): 1312.[12]Luu HH, Song WX, Luo X, et al. Distinct roles of bone morphogenetic proteins in osteogenic differentiation of mesenchymal stem cells.J Orthop Res. 2007;25(5):665-677.[13]Luther G, Wagner ER, Zhu G,et al. BMP-9 Induced Osteogenic Differentiation of Mesenchymal Stem Cells: Molecular Mechanism and Therapeutic Potential.Curr Gene Ther. 2011;11(3):229-240.[14]Khorsand B, Elangovan S, Hong L,et al.A Comparative Study of the Bone Regenerative Effect of Chemically Modified RNA Encoding BMP-2 or BMP-9. AAPS J.2017;19(2):438.[15]Olsen OE, Sankar M, Elsaadi S, et al. BMPR2 inhibits activin and BMP signaling via wild-type ALK2. J Cell Sci.2018;131(11).[16]Haimov H, Yosupov N, Pinchasov G, et al. Bone Morphogenetic Protein Coating on Titanium Implant Surface: a Systematic Review. J Oral Maxillofac Res.2017;8(2):e1[17]Zhang J, Li L. BMP signaling and stem cell regulation. Dev Biol. 2005;284(1):1-11.[18]Wang RN, Green J, Wang Z, et al. Bone Morphogenetic Protein (BMP) signaling in development and human diseases. Genes Dis. 2014;1(1): 87-105.[19]Zhang F, Song J, Zhang H, et al. Wnt and BMP Signaling Crosstalk in Regulating Dental Stem Cells: Implications in Dental Tissue Engineering. Genes Dis.2016;3(4):263-276.[20]Lindsley HB, Smith DD. Enhanced prostaglandin E2 secretion by cytokine-stimulated human synoviocytes in the presence of subtherapeutic concentrations of nonsteroidal antiinflammatory drugs. Arthritis Rheum.1990; 33(8): 1162-1169.[21]Canalis E. Growth factor control of bone mass. J Cell Biochem. 2009;108(4):769-777.[22]Milat F, Ng KW. Is Wnt signalling the final common pathway leading to bone formation. Mol Cell Endocrinol.2009; 310(1-2): 52-62.[23]Rosen V. BMP2 signaling in bone development and repair. Cytokine Growth Factor Rev.2009; 20(5-6): 475-480.[24]Komori T. Regulation of bone development and extracellular matrix protein genes by RUNX2. Cell Tissue Res.2010;339(1): 189-195.[25]Lian JB, Stein GS, Javed A, et al. Networks and hubs for the transcriptional control of osteoblastogenesis. Rev Endocr Metab Disord.2006;7(1-2):1-16.[26]Jensen ED, Nair AK, Westendorf JJ. Histone deacetylase co-repressor complex control of Runx2 and bone formation. Crit Rev Eukaryot Gene Expr.2007;17(3):187-196.[27]Stein GS, Zaidi SK, Stein JL, et al. Transcription-factor-mediated epigenetic control of cell fate and lineage commitment. Biochem Cell Biol. 2009;87(1):1-6.[28]Haasemann M, Nawratil P, Mülleresterl W. Rat tyrosine kinase inhibitor shows sequence similarity to human alpha 2-HS glycoprotein and bovine fetuin. Biochem J.1991;274 (Pt 3)(3): 899-902.[29]Senta H, Park H, Bergeron E, et al. Cell responses to bone morphogenetic proteins and peptides derived from them: biomedical applications and limitations.Cytokine Growth Factor Rev.2009;20(3): 213-222[30]Singhatanadgit W,Olsen I.Endogenous BMPR-IB signaling is required for early osteoblast differentiation of human bone cells. Vitro Cellular & Developmental Biology Animal.2011; 47(3): 251-259.[31]Bonilla-Claudio M, Wang J, Bai Y,et al. Bmp signaling regulates a dose-dependent transcriptional program to control facial skeletal development. Development.2012;139(4): 709-719.[32]Xiang L, Liang C, Ke ZY,et al. BMP9-Induced Osteogenetic Differentiation and Bone Formation of Muscle-Derived Stem Cells. Biomed Res Int.2012;2012(1):111-113.[33]Song JJ, Celeste AJ, Kong FM,et al. Bone morphogenetic protein-9 binds to liver cells and stimulates proliferation. Endocrinology. 1995;136(10): 4293-4297.[34]Souza A, Bezerra B, Oliveira FS, et al. Effect of bone morphogenetic protein 9 on osteoblast differentiation of cells grown on titanium with nanotopography. J Cell Biochem. 2018; 119(10): 8441-8449.[35]Vhora I, Lalani R, Bhatt P, et al. Lipid-nucleic acid nanoparticles of novel ionizable lipids for systemic BMP-9 gene delivery to bone-marrow mesenchymal stem cells for osteoinduction. Int J Pharm 2019;563:324-336.[36]Huang X, Wang F, Zhao C, et al. Dentinogenesis and Tooth-Alveolar Bone Complex Defects in BMP9/GDF2 Knockout Mice. Stem Cells Dev 2019;28(10):683-694.[37]Nakamura T, Shirakata Y, Shinohara Y, et al. Comparison of the effects of recombinant human bone morphogenetic protein-2 and -9 on bone formation in rat calvarial critical-size defects. Clin Oral Investig.2017; 21(9): 2671-2679.[38]Peng Y, Kang Q, Cheng H, et al. Transcriptional characterization of Bone morphogenetic proteins (BMPs)-mediated osteogenic signaling. J Cell Biochem.2003;90(6):1149–1165.[39]Luo Q, Kang Q, Si W, et al. Connective tissue growth factor (CTGF) is regulated by Wnt and bone morphogenetic proteins signaling in osteoblast differentiation of mesenchymal stem cells. J Biol Chem.2004;279(53):55958-55968.[40]Si W, Kang Q, Luu HH, et al. CCN1/Cyr61 is regulated by the canonical Wnt signal and plays an important role in Wnt3A-induced osteoblast differentiation of mesenchymal stem cells.Mol Cell Biol. 2006;26(8):2955-2964.[41]Liu H, Zhong L, Yuan T, et al. MicroRNA-155 inhibits the osteogenic differentiation of mesenchymal stem cells induced by BMP9 via downregulation of BMP signaling pathway. Int J Mol Med.2018;41(6): 3379-3393.[42]Yan S, Zhang R, Ke W, et al. Characterization of the essential role of Bone Morphogenetic Protein 9 (BMP9) in osteogenic differentiation of mesenchymal stem cells (MSCs) through RNA interference. Genes Dis 2018;5(2):172-184.[43]Zanotti S, Canalis E. Notch Signaling and the Skeleton. Endocr Rev 2016;37(3):223-253.[44]Bolós V, Grego-Bessa J, Jl DLP. Notch signaling in development and cancer. Endocr Rev.2007; 28(3): 339-363.[45]Lardelli M, Dahlstrand J, Lendahl U. The novel Notch homologue mouse Notch 3 lacks specific epidermal growth factor-repeats and is expressed in proliferating neuroepithelium.Mech Dev. 1994; 46(2): 123-136.[46]Uyttendaele H, Marazzi G, Wu G,et al. Notch4/int-3, a mammary proto-oncogene, is an endothelial cell-specific mammalian Notch gene. Development. 1996.122(7):2251-2259.[47]Shutter JR, Scully S, Fan W, et al. Dll4, a novel Notch ligand expressed in arterial endothelium. Genes Dev.2000;14(11): 1313-1318.[48]Yavropoulou MP, Yovos JG. The role of Notch signaling in bone development and disease. Hormones. 2014;13(1): 24-37.[49]Cui J, Zhang W, Huang E, et al. BMP9-induced osteoblastic differentiation requires functional Notch signaling in mesenchymal stem cells. Lab Invest. 2019;99(1):58-71.[50]Cao J, Wei Y, Lian J, et al. Notch signaling pathway promotes osteogenic differentiation of mesenchymal stem cells by enhancing BMP9/Smad signaling.Int J Mol Med. 2017;40(2): 378-388.[51]Fujiokakobayashi M, Schaler P, Shirakata D,et al. Comparison of Two Porcine Collagen Membranes Combined with rhBMP-2 and rhBMP-9 on Osteoblast Behavior In Vitro. Int J Oral Maxillofac Implants. 2017;32(4):221-230.[52]Liao J, Wei Q, Zou Y, et al. Notch Signaling Augments BMP9-Induced Bone Formation by Promoting the Osteogenesis-Angiogenesis Coupling Process in Mesenchymal Stem Cells (MSCs). Cell Physiol Biochem. 2017;41(5):1905-1923.[53]Wang J, Wynshaw-Boris A.The canonical Wnt pathway in early mammalian embryogenesis and stem cell maintenance/ differentiation. Curr Opin Genet Dev.2004;14(5):533-539.[54]Cadigan KM, Nusse R.Wnt signaling: a common theme in animal?development. Genes Dev. 1997;11(24):3286-3305.[55]Nd GD, Karsenty G. In vivo analysis of Wnt signaling in bone. Endocrinology 2007;148(6):2630-2634.[56]Nd GD, Karsenty G. Molecular bases of the regulation of bone remodeling by the canonical Wnt signaling pathway. Curr Top Dev Biol.2006;73(73):43-84.[57]Liu Y, Liu Y, Zhang R, et al. All-trans retinoic acid modulates bone morphogenic protein 9-induced osteogenesis and adipogenesis of preadipocytes through BMP/Smad and Wnt/β-catenin signaling pathways. Int J Biochem Cell Biol.2014; 47: 47-56.[58]Wang H, He XQ, Jin T, et al. Wnt11 plays an important role in the osteogenesis of human mesenchymal stem cells in a PHA/FN/ALG composite scaffold: possible treatment for infected bone defect. Stem Cell Res Ther.2016;7(1):1-13.[59]Zhu JH, Liao YP, Li FS, et al. Wnt11 promotes BMP9-induced osteogenic differentiation through BMPs/Smads and p38 MAPK in mesenchymal stem cells. J Cell Biochem.2018;119(11): 9462-9473.[60]Liao YP, Du WM, Hu Y, et al. CREB/Wnt10b mediates the effect of COX-2 on promoting BMP9-induced osteogenic differentiation via reducing adipogenic differentiation in mesenchymal stem cells. J Cell Biochem. 2019;120(6):9572-9587.[61]Tang N,Song W,Luo J,et al. BMP‐9‐induced osteogenic differentiation of mesenchymal progenitors requires functional canonical Wnt/β‐catenin signalling.J Cell Mol Med. 2009;13(8B): 2448-2464.[62]Deng ZL, Sharff KA, Tang N, et al.Regulation of osteogenic differentiation during skeletal development. Front Biosci.2008; 13(6):2001-2021.[63]Yuan C, Gou X, Deng J,et al. FAK and BMP-9 synergistically trigger osteogenic differentiation and bone formation of adipose derived stem cells through enhancing Wnt-β-catenin signaling. Biomed Pharmacother. 2018l105 753-757.[64]Zhang H, Wang J, Deng F, et al. Canonical Wnt signaling acts synergistically on BMP9-induced osteo/odontoblastic differentiation of stem cells of dental apical papilla (SCAPs). Biomaterials 2015;39:145-154.[65]Li XL, Liu YB, Ma EG, et al. Synergistic effect of BMP9 and TGF-β in the proliferation and differentiation of osteoblasts.Genet Mol Res. 2015;14(3):7605-7615.[66]Wang P, Wang Y, Tang W, et al. Bone Morphogenetic Protein-9 Enhances Osteogenic Differentiation of Human Periodontal Ligament Stem Cells via the JNK Pathway. PLoS One. 2017;12(1): e0169123.[67]Fietz MJ, Concordet JP, Barbosa R, et al. The hedgehog gene family in Drosophila and vertebrate development. Dev Suppl. 1994:43-51.[68]Mundy GR, Yang X. Hedgehog coordination of postnatal osteoclast and osteoblast activities. Dev Cell. 2008;14(5): 637-638.[69]Ingham PW, Mcmahon AP. Hedgehog signaling in animal development: paradigms and principles.Genes Dev. 2001; 15(23): 3059-3087.[70]Ohba S, Kawaguchi H, F, et al. Patched1 Haploinsufficiency Increases Adult Bone Mass and Modulates Gli3 Repressor Activity. Dev Cell.2008;14(5):674-688.[71]Li L, Dong Q, Wang Y, et al.Hedgehog signaling is involved in the BMP9-induced osteogenic differentiation of mesenchymal stem cells. Int J Mol Med.2015;35(6):1641-1650.[72]Choi JY, Pratap J, Javed A, et al. Subnuclear targeting of Runx/Cbfa/AML factors is essential for tissue-specific differentiation during embryonic development. Proc Natl Acad Sci U S A.2001.98(15):8650-8655.[73]Ji C, Liu X, Xu L, et al.RUNX1 Plays an Important Role in Mediating BMP9-Induced Osteogenic Differentiation of Mesenchymal Stem Cells Line C3H10T1/2, Murine Multi-Lineage Cells Lines C2C12 and MEFs. Int J Mol Sci.2017;18(7):1348.[74]Sharff KA, Song WX, Luo X, et al. Hey1 Basic Helix-Loop-Helix Protein Plays an Important Role in Mediating BMP9-induced Osteogenic Differentiation of Mesenchymal Progenitor Cells. J Biol Chem.2009;284(1): 649-659.[75]Wang Y, Feng Q, Ji C,et al. RUNX3 plays an important role in mediating the BMP9-induced osteogenic differentiation of mesenchymal stem cells.Int J Mol Med. 2017;40(6):1991-1999. [76]Wöltje K, Jabs M, Fischer A. Serum Induces Transcription of Hey1 and Hey2 Genes by Alk1 but Not Notch Signaling in Endothelial Cells. PLoS One.2015;10(3): e0120547.[77]Xiao Y, Zeng Z, Xing J. Hey1 functions as a positive regulator of odontogenic differentiation in odontoblast-lineage cells. Int J Mol Med. 2018;41(1): 331-339.[78]Wang JH, Liu YZ, Yin LJ, et al. BMP9 and COX-2 form an important regulatory loop in BMP9-induced osteogenic differentiation of mesenchymal stem cells. Bone.2013; 57(1): 311-321.[79]Su X, Wei Y, Cao J, et al. CCN3 and DLL1 co-regulate osteogenic differentiation of mouse embryonic fibroblasts in a Hey1-dependent manner. Cell Death Dis. 2018;9(12):1188.[80]Wang Y, Yuan M, Guo QY,et al. Mesenchymal Stem Cells for Treating Articular Cartilage Defects and Osteoarthritis.Cell Transplant. 2015; 24(9): 1661-1678.[81]Liu X, Du M, Wang Y,et al. BMP9 overexpressing adipose-derived mesenchymal stem cells promote cartilage repair in osteoarthritis-affected knee joint via the Notch1/Jagged1 signaling pathway. Exp Ther Med.2018;16(6):4623-4631.[82]van Baardewijk LJ, van der Ende J, Lissenberg-Thunnissen S, et al. Circulating bone morphogenetic protein levels and delayed fracture healing. Int Orthop. 2013;37(3):523-527.[83]Wang X, Huang J, Huang F, et al.Bone morphogenetic protein 9 stimulates callus formation in osteoporotic rats during fracture healing. Mol Med Rep. 2017;15(5):2537-2545.[84]Yu L, Dawson LA, Yan M, et al. BMP9 stimulates joint regeneration at digit amputation wounds in mice. Nat Commun. 2019;10(1): 424.[85]Shui W, Zhang W, Yin L, et al. Characterization of scaffold carriers for BMP9-transduced osteoblastic progenitor cells in bone regeneration.J Biomed Mater Res A.2014; 102(10): 3429-3438.[86]Dumont RJ, Dayoub H, Li JZ, et al. Ex vivo bone morphogenetic protein-9 gene therapy using human mesenchymal stem cells induces spinal fusion in rodents. Neurosurgery.2002; 51(5): 1239-1245.[87]Zhang R, Li X, Liu Y, et al. Acceleration of Bone Regeneration in Critical-Size Defect Using BMP-9-Loaded nHA/ColI/MWCNTs Scaffolds Seeded with Bone Marrow Mesenchymal Stem Cells. Biomed Res Int.2019;2019:7343957. |
| [1] | 蒲 锐, 陈子扬, 袁凌燕. 不同细胞来源外泌体保护心脏的特点与效应[J]. 中国组织工程研究, 2021, 25(在线): 1-. |
| [2] | 林清凡, 解一新, 陈婉清, 叶振忠, 陈幼芳. 人胎盘源间充质干细胞条件培养液可上调缺氧状态下BeWo细胞活力和紧密连接因子的表达[J]. 中国组织工程研究, 2021, 25(在线): 4970-4975. |
| [3] | 侯婧瑛, 于萌蕾, 郭天柱, 龙会宝, 吴 浩. 缺氧预处理激活HIF-1α/MALAT1/VEGFA通路促进骨髓间充质干细胞生存和血管再生[J]. 中国组织工程研究, 2021, 25(7): 985-990. |
| [4] | 史洋洋, 秦英飞, 吴福玲, 何 潇, 张雪静. 胎盘间充质干细胞预处理预防小鼠毛细支气管炎[J]. 中国组织工程研究, 2021, 25(7): 991-995. |
| [5] | 梁学奇, 郭黎姣, 陈贺捷, 武 杰, 孙雅琪, 邢稚坤, 邹海亮, 陈雪玲, 吴向未. 泡状棘球绦虫原头蚴抑制骨髓间充质干细胞向成纤维细胞的分化[J]. 中国组织工程研究, 2021, 25(7): 996-1001. |
| [6] | 樊全宝, 罗惠娜, 王丙云, 陈胜锋, 崔连旭, 江文康, 赵明明, 王静静, 罗冬章, 陈志胜, 白银山, 刘璨颖, 张 晖. 低氧培养犬脂肪间充质干细胞的生物学特性[J]. 中国组织工程研究, 2021, 25(7): 1002-1007. |
| [7] | 耿 瑶, 尹志良, 李兴平, 肖东琴, 侯伟光. hsa-miRNA-223-3p调控人骨髓间充质干细胞成骨分化的作用[J]. 中国组织工程研究, 2021, 25(7): 1008-1013. |
| [8] | 伦志刚, 金 晶, 王添艳, 李爱民. 过氧化物还原酶6干预骨髓间充质干细胞增殖及体外向神经谱系诱导分化[J]. 中国组织工程研究, 2021, 25(7): 1014-1018. |
| [9] | 朱雪芬, 黄 成, 丁 健, 戴永平, 刘元兵, 乐礼祥, 王亮亮, 杨建东. 胶质细胞神经营养因子诱导骨髓间充质干细胞向功能性神经元分化的机制[J]. 中国组织工程研究, 2021, 25(7): 1019-1025. |
| [10] | 段丽芸, 曹晓沧. 人胎盘间充质干细胞来源细胞外囊泡调节肠炎小鼠肠黏膜胶原的沉积[J]. 中国组织工程研究, 2021, 25(7): 1026-1031. |
| [11] | 裴丽丽, 孙贵才, 王 弟. 丹酚酸B抑制骨髓间充质干细胞氧化损伤及促进分化为心肌样细胞[J]. 中国组织工程研究, 2021, 25(7): 1032-1036. |
| [12] | 邹 刚, 徐 志, 刘子铭, 李豫皖, 杨继滨, 金 瑛, 张 骏, 葛 振, 刘 毅. 人脱细胞羊膜支架促进Scleraxis修饰人羊膜间充质干细胞体外成韧带分化[J]. 中国组织工程研究, 2021, 25(7): 1037-1044. |
| [13] | 汪显耀, 关亚琳, 刘忠山. 提高间充质干细胞治疗难愈性创面的策略[J]. 中国组织工程研究, 2021, 25(7): 1081-1087. |
| [14] | 万 然, 史 旭, 刘京松, 王岩松. 间充质干细胞分泌组治疗脊髓损伤的研究进展[J]. 中国组织工程研究, 2021, 25(7): 1088-1095. |
| [15] | 王诗琦, 张金生. 中医药调控缺血缺氧微环境对骨髓间充质干细胞增殖、分化及衰老的影响[J]. 中国组织工程研究, 2021, 25(7): 1129-1134. |
中国组织工程研究杂志出版内容重点:干细胞;骨髓干细胞;造血干细胞;脂肪干细胞;肿瘤干细胞;胚胎干细胞;脐带脐血干细胞;干细胞诱导;干细胞分化;组织工程
.jpg)
中国组织工程研究杂志出版内容重点:干细胞;骨髓干细胞;造血干细胞;脂肪干细胞;肿瘤干细胞;胚胎干细胞;脐带脐血干细胞;干细胞诱导;干细胞分化;组织工程
中国组织工程研究杂志出版内容重点:干细胞;骨髓干细胞;造血干细胞;脂肪干细胞;肿瘤干细胞;胚胎干细胞;脐带脐血干细胞;干细胞诱导;干细胞分化;组织工程
.jpg)
研究骨形态发生蛋白9在成骨过程中的作用机制及其在骨科领域中应用的意义:骨形态发生蛋白9的信号级联关系非常复杂且涉及到了细胞生长、发育、凋亡等生物过程,尤其在成骨分化方面,骨形态发生蛋白2,4,7等传统促进成骨的骨形态发生蛋白蛋白会被骨形态发生蛋白3及Noggin所抑制,但骨形态发生蛋白9不受骨形态发生蛋白3及Noggin所抑制,说明其与传统的骨形态发生蛋白蛋白信号传导机制在成骨诱导方面具有差异。目前研究已经证明,骨形态发生蛋白9能够促进骨愈合及骨量增加,在骨缺损、骨肿瘤、骨质疏松等骨科疾病治疗中具有巨大潜力。因此,深入的了解骨形态发生蛋白9在成骨过程中的作用机制,将为骨科相关疾病的诊疗提供坚实的理论基础。 中国组织工程研究杂志出版内容重点:干细胞;骨髓干细胞;造血干细胞;脂肪干细胞;肿瘤干细胞;胚胎干细胞;脐带脐血干细胞;干细胞诱导;干细胞分化;组织工程
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||