| [1] 中华医学会骨质疏松和骨矿盐疾病分会.原发性骨质疏松症诊治指南(2011年)[J].中华骨质疏松和骨矿盐疾病杂志,2011,4(1):2-17.
[2] 中华医学会骨质疏松和骨矿盐疾病分会,中华医学会骨科学分会骨质疏松学组.骨质疏松性骨折患者抗骨质疏松治疗与管理专家共识[J]. 中华骨质疏松和骨矿盐疾病杂志,2015,8(3):189-195.
[3] Ford MA, Bass M, Zhao Y, et al. Osteoporosis Knowledge, Self-Efficacy, and Beliefs among College Students in the USA and China. J Osteoporos. 2011; 2011:729219.
[4] Balasubramanian A, Tosi LL, Lane JM, et al. Declining rates of osteoporosis management following fragility fractures in the U.S., 2000 through 2009. J Bone Joint Surg Am. 2014;96(7):e52.
[5] 廖二元,徐苓,朱汉民,等.原发性骨质疏松症干预的疗效监测与评估专家意见[J]. 中华骨质疏松和骨矿盐疾病杂志, 2015,8(1):1-6.
[6] Cosman F, de Beur SJ, LeBoff MS, et al. Clinician's Guide to Prevention and Treatment of Osteoporosis. Osteoporos Int. 2014;25(10):2359-2381.
[7] 李楠,张贵林,何达,等.骨水泥的分布与剂量对椎体成形术疗效影响的研究[J].中国骨与关节损伤杂志,2015,30(1): 66-68.
[8] Wang E, Yi H, Wang M, et al. Treatment of osteoporotic vertebral compression fractures with percutaneous kyphoplasty: a report of 196 cases. Eur J Orthop Surg Traumatol. 2013;23 Suppl 1:S71-75.
[9] 章波,杨波,尹飚,等.经皮穿刺椎体成形术治疗90岁以上老人骨质疏松性椎体压缩性骨折[J].中国微创外科杂志, 2014,14(5):445-449.
[10] 杨波,谢景开,尹飚,等.经皮椎体成形术治疗老年多节段骨质疏松性椎体压缩性骨折[J].中国矫形外科杂志,2012, 20(24): 2212-2216.
[11] 黎双庆,杨波,杨逸禧,等.经皮穿刺椎体成形术治疗骨质疏松性严重椎体压缩性骨折[J].中国微创外科杂志,2015, 15(9):818-821.
[12] 麦合木提江•穆海麦提,祝少博,李景峰,等.两种方法治疗骨质疏松致椎体压缩性骨折:安全与有效性的Meta分析[J].中国组织工程研究,2014,18(22):3551-3559.
[13] 蓝涛,陈扬,杨欣建. 椎体成形术后再骨折研究进展[J]. 中国脊柱脊髓杂志,2015,25(2):179-182.
[14] Klazen CA, Venmans A, de Vries J, et al. Percutaneous vertebroplasty is not a risk factor for new osteoporotic compression fractures: results from VERTOS II. AJNR Am J Neuroradiol. 2010;31(8): 1447-1450.
[15] Lu K, Liang CL, Hsieh CH, et al. Risk factors of subsequent vertebral compression fractures after vertebroplasty. Pain Med. 2012;13(3):376-382.
[16] Yoo CM, Park KB, Hwang SH, et al. The analysis of patterns and risk factors of newly developed vertebral compression fractures after percutaneous vertebroplasty. J Korean Neurosurg Soc. 2012; 52(4): 339-345.
[17] Lin WC, Lee YC, Lee CH, et al. Refractures in cemented vertebrae after percutaneous vertebroplasty: a retrospective analysis. Eur Spine J. 2008;17(4):592-599.
[18] Kim YY, Rhyu KW. Recompression of vertebral body after balloon kyphoplasty for osteoporotic vertebral compression fracture. Eur Spine J. 2010;19(11): 1907-1912.
[19] DePalma MJ, Ketchum JM, Frankel BM, et al. Percutaneous vertebroplasty for osteoporotic vertebral compression fractures in the nonagenarians: a prospective study evaluating pain reduction and new symptomatic fracture rate. Spine (Phila Pa 1976). 2011;36(4):277-282.
[20] Li YA, Lin CL, Chang MC, et al. Subsequent vertebral fracture after vertebroplasty: incidence and analysis of risk factors. Spine (Phila Pa 1976). 2012;37(3): 179-183.
[21] Bawa HS, Weick J, Dirschl DR.Anti-Osteoporotic Therapy After Fragility Fracture Lowers Rate of Subsequent Fracture: Analysis of a Large Population Sample. J Bone Joint Surg Am. 2015;97(19): 1555-1562.
[22] 林婕,沈芸.482例骨质疏松性骨折住院患者再次骨折分析[J].中国老年保健医学, 2015,13(4):47-49.
[23] 邱贵兴,裴福兴,胡侦明,等. 中国骨质疏松性骨折诊疗指南(骨质疏松性骨折诊断及治疗原则)[J].中华骨与关节外科杂志,2015,8(5):371-375.
[24] 印平,马远征,马迅,等.骨质疏松性椎体压缩性骨折的治疗指南[J]. 中国骨质疏松杂志,2015,21(6):643-648.
[25] Oudshoorn C, Hartholt KA, Zillikens MC, et al. Emergency department visits due to vertebral fractures in the Netherlands, 1986-2008: steep increase in the oldest old, strong association with falls. Injury. 2012; 43(4):458-461.
[26] Rad AE, Gray LA, Sinaki M, et al. Role of physical activity in new onset fractures after percutaneous vertebroplasty. Acta Radiol. 2011;52(9):1020-1023.
[27] Zafeiris CP, Lyritis GP, Papaioannou NA, et al. Hypovitaminosis D as a risk factor of subsequent vertebral fractures after kyphoplasty. Spine J. 2012; 12(4):304-312.
[28] Harrop JS, Prpa B, Reinhardt MK, et al. Primary and secondary osteoporosis' incidence of subsequent vertebral compression fractures after kyphoplasty. Spine (Phila Pa 1976). 2004;29(19):2120-2125.
[29] 中华医学会骨质疏松和骨矿盐疾病分会,中华医学会骨科学分会骨质疏松学组.骨质疏松性骨折患者抗骨质疏松治疗与管理专家共识[J]. 中华骨质疏松和骨矿盐疾病杂志,2015,8(3):189-195.
[30] Su CH, Tu PH, Yang TC, et al. Comparison of the therapeutic effect of teriparatide with that of combined vertebroplasty with antiresorptive agents for the treatment of new-onset adjacent vertebral compression fracture after percutaneous vertebroplasty. J Spinal Disord Tech. 2013;26(4):200-206.
[31] 杜艳萍,朱汉民,李慧林,等.绝经后妇女使用抗骨质疏松症药物的依从性及其影响因素分析[J].中国骨质疏松杂志, 2012,18(2): 302-306.
[32] 常青,史相钦. PKP结合抗骨质疏松药物治疗骨质疏松性椎体压缩性骨折疗效观察[J].中国骨与关节损伤杂志, 2015,30(5):522-523.
[33] 陈剑峰,王建伟,杨智杰. 椎体后凸成形术后椎体再发骨折9例分析[J]. 江苏医药,2014,40(24):3073-3074.
[34] 杨刘柱,陈仲,严鑫平,等. 椎体骨水泥注入联合抗骨质疏松药物治疗急性骨质疏松性椎体压缩性骨折[J]. 中国组织工程研究,2014,18(39):6265-6270.
[35] 何晓辉,王明森,汪道清,等.伊班磷酸钠在多发性老年骨质疏松性脊柱骨折术后的应用[J].海南医学,2016,27(2): 213-216.
[36] 王英东,孙永新.鲑鱼降钙素联合维生素D在预防老年骨质疏松患者全髋关节置换术后跌倒中的应用[J].中国医药导刊,2015,17(5):471-472.
[37] 彭鹏,王清.经皮椎体成形术后给予抗骨质疏松药物治疗对再发脊柱椎体压缩骨折的疗效观察[J].中国实用医药, 2015,10(26):145-146.
[38] 唐佩福.抗骨质疏松治疗对骨质疏松性骨折的治疗影响及建议[J].中华老年多器官疾病杂志,2014,13(7): 481-484.
[39] 余舒芳,林建华,李毅中,等.骨质疏松性骨折二级预防的综合管理--骨质疏松性骨折二级预防示范基地福州中心专家共识[J].中华关节外科杂志:电子版,2014,8(6): 808-812.
[40] 袁宏,钟惠琴,陆琳松,等.全髋关节置换术后联合抗骨质疏松治疗的价值[J].中华关节外科杂志:电子版,2014,8(3): 376-379.
[41] 袁宏,陆琳松,钟惠琴, 等.唑来膦酸对骨质疏松患者全髋关节置换术后假体周围骨密度的影响[J].中华关节外科杂志:电子版,2014,8(3):278-285. |
.jpg) 文题释义:
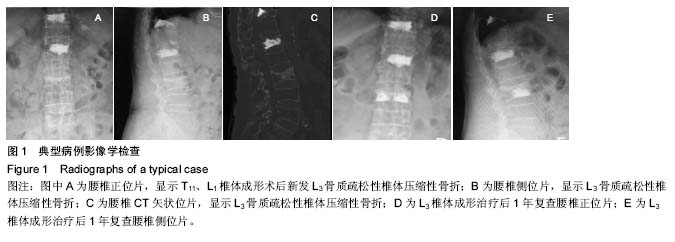
椎体成形技术:是针对确诊骨质疏松性椎体压缩性骨折患者,通过椎弓根或直接向椎体内注射骨水泥的方法,达到增强椎体强度和稳定性、防止塌陷、缓解腰背疼痛的微创治疗方法,目前在骨质疏松性椎体压缩性骨折治疗中已成为“金标准”,但就骨质疏松性椎体压缩性骨折而言,若不重视后期规范抗骨质疏松治疗方案,此类患者再骨折发生率明显增高。
骨质疏松性椎体压缩性骨折:因骨质疏松出现骨量减低、骨强度下降、骨脆性增加,在轻微损伤或日常活动中即可导致的椎体脆性骨折称为骨质疏松性椎体压缩性骨折。骨质疏松性骨折是骨质疏松症的严重后果,目前针对此类骨折多推荐采取椎体成形技术治疗,同时此类骨折规范抗骨质疏松治疗亦不可或缺。
文题释义:
椎体成形技术:是针对确诊骨质疏松性椎体压缩性骨折患者,通过椎弓根或直接向椎体内注射骨水泥的方法,达到增强椎体强度和稳定性、防止塌陷、缓解腰背疼痛的微创治疗方法,目前在骨质疏松性椎体压缩性骨折治疗中已成为“金标准”,但就骨质疏松性椎体压缩性骨折而言,若不重视后期规范抗骨质疏松治疗方案,此类患者再骨折发生率明显增高。
骨质疏松性椎体压缩性骨折:因骨质疏松出现骨量减低、骨强度下降、骨脆性增加,在轻微损伤或日常活动中即可导致的椎体脆性骨折称为骨质疏松性椎体压缩性骨折。骨质疏松性骨折是骨质疏松症的严重后果,目前针对此类骨折多推荐采取椎体成形技术治疗,同时此类骨折规范抗骨质疏松治疗亦不可或缺。.jpg) 文题释义:
椎体成形技术:是针对确诊骨质疏松性椎体压缩性骨折患者,通过椎弓根或直接向椎体内注射骨水泥的方法,达到增强椎体强度和稳定性、防止塌陷、缓解腰背疼痛的微创治疗方法,目前在骨质疏松性椎体压缩性骨折治疗中已成为“金标准”,但就骨质疏松性椎体压缩性骨折而言,若不重视后期规范抗骨质疏松治疗方案,此类患者再骨折发生率明显增高。
骨质疏松性椎体压缩性骨折:因骨质疏松出现骨量减低、骨强度下降、骨脆性增加,在轻微损伤或日常活动中即可导致的椎体脆性骨折称为骨质疏松性椎体压缩性骨折。骨质疏松性骨折是骨质疏松症的严重后果,目前针对此类骨折多推荐采取椎体成形技术治疗,同时此类骨折规范抗骨质疏松治疗亦不可或缺。
文题释义:
椎体成形技术:是针对确诊骨质疏松性椎体压缩性骨折患者,通过椎弓根或直接向椎体内注射骨水泥的方法,达到增强椎体强度和稳定性、防止塌陷、缓解腰背疼痛的微创治疗方法,目前在骨质疏松性椎体压缩性骨折治疗中已成为“金标准”,但就骨质疏松性椎体压缩性骨折而言,若不重视后期规范抗骨质疏松治疗方案,此类患者再骨折发生率明显增高。
骨质疏松性椎体压缩性骨折:因骨质疏松出现骨量减低、骨强度下降、骨脆性增加,在轻微损伤或日常活动中即可导致的椎体脆性骨折称为骨质疏松性椎体压缩性骨折。骨质疏松性骨折是骨质疏松症的严重后果,目前针对此类骨折多推荐采取椎体成形技术治疗,同时此类骨折规范抗骨质疏松治疗亦不可或缺。

.jpg) 文题释义:
椎体成形技术:是针对确诊骨质疏松性椎体压缩性骨折患者,通过椎弓根或直接向椎体内注射骨水泥的方法,达到增强椎体强度和稳定性、防止塌陷、缓解腰背疼痛的微创治疗方法,目前在骨质疏松性椎体压缩性骨折治疗中已成为“金标准”,但就骨质疏松性椎体压缩性骨折而言,若不重视后期规范抗骨质疏松治疗方案,此类患者再骨折发生率明显增高。
骨质疏松性椎体压缩性骨折:因骨质疏松出现骨量减低、骨强度下降、骨脆性增加,在轻微损伤或日常活动中即可导致的椎体脆性骨折称为骨质疏松性椎体压缩性骨折。骨质疏松性骨折是骨质疏松症的严重后果,目前针对此类骨折多推荐采取椎体成形技术治疗,同时此类骨折规范抗骨质疏松治疗亦不可或缺。
文题释义:
椎体成形技术:是针对确诊骨质疏松性椎体压缩性骨折患者,通过椎弓根或直接向椎体内注射骨水泥的方法,达到增强椎体强度和稳定性、防止塌陷、缓解腰背疼痛的微创治疗方法,目前在骨质疏松性椎体压缩性骨折治疗中已成为“金标准”,但就骨质疏松性椎体压缩性骨折而言,若不重视后期规范抗骨质疏松治疗方案,此类患者再骨折发生率明显增高。
骨质疏松性椎体压缩性骨折:因骨质疏松出现骨量减低、骨强度下降、骨脆性增加,在轻微损伤或日常活动中即可导致的椎体脆性骨折称为骨质疏松性椎体压缩性骨折。骨质疏松性骨折是骨质疏松症的严重后果,目前针对此类骨折多推荐采取椎体成形技术治疗,同时此类骨折规范抗骨质疏松治疗亦不可或缺。