中国组织工程研究 ›› 2018, Vol. 22 ›› Issue (2): 178-182.doi: 10.3969/j.issn.2095-4344.0003
• 组织工程骨及软骨材料 tissue-engineered bone and cartilage materials • 上一篇 下一篇
聚甲基丙烯酸甲酯骨水泥注射治疗跟骨Sanders Ⅲ型骨折的生物力学测试
管志海,王勤业,常小波,宁 波,罗亚平
- 上海市嘉定区南翔医院,上海市 201802
Treatment of Sanders type III fracture of the calcaneus with polymethylmethacrylate bone cement: a biomechanical study
Guan Zhi-hai, Wang Qin-ye, Chang Xiao-bo, Ning Bo, Luo Ya-ping
- Nanxiang Hospital of Jiading District, Shanghai 201802, China
摘要:
文章快速阅读:
.jpg)
文题释义:
聚甲基丙烯酸甲酯骨水泥:是一种用于填充骨与植入物间隙或骨腔并具有自凝特性的生物材料,自从1958年Charney首次应用骨水泥固定股骨假体成功施行全髋关节置换以来,骨水泥已广泛应用于骨科临床,骨水泥固定可保证术后假体的即时稳定,在骨组织-骨水泥-假体界面上无任何微动,允许术后早期负重,疗效肯定。
跟骨骨折Sanders分型:Sanders根据CT 30°半冠状位扫描,最大程度显示距下关节后关节面,将跟骨平均分为3柱,跟骨后关节面由平行于跟骨纵轴的A、B两线分为3 个等大的区域,产生3种潜在的骨折块,外侧、中央、内侧;Ⅰ型,所有无移位的关节内骨折;Ⅱ型,后关节面2片段骨折,根据骨折线的位置分为A、B、C3个亚型;Ⅲ型,后关节面3片段骨折,按照2个骨折线的位置分为AB、AC或BC3个亚型;Ⅳ型,后关节面4片段骨折,为严重的粉碎性关节内骨折,常不止4个骨块。
背景:聚甲基丙烯酸甲酯骨水泥已被广泛应用于骨科临床,可保证术后假体的即刻稳定性,且界面无微动,允许术后早期负重,疗效肯定。
目的:采用生物力学实验验证聚甲基丙烯酸甲酯骨水泥注射治疗跟骨Sanders Ⅲ型骨折的疗效。
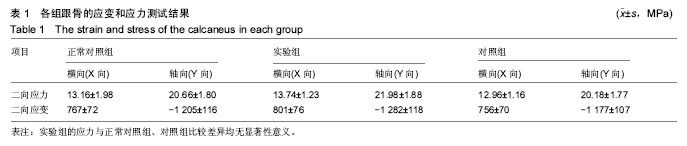
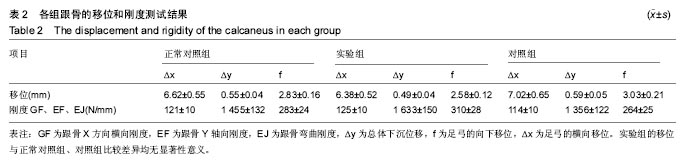
方法:采集8具成人新鲜尸体踝跟骨标本,检测其生物力学性能,作为正常对照组;实验组(n=4)、对照组(n=4)制作根骨Sanders Ⅲ型骨折模型,实验组在骨缺损区植入聚甲基丙烯酸甲酯骨水泥,对照组骨缺损区植入人工骨,对照组以钢板固定外侧壁,检测两组标本的生物力学性能。
结果与结论:①跟骨的应变和应力强度:正常对照组的应力分布与实验组应力分布规律相一致,两组应力比较差异无显著性意义;实验组与对照组的应力相近,组间比较差异无显著性意义;②跟骨的移位与轴向刚度:与正常对照组相比,实验组的跟骨移位略有降低,但差异无显著性意义;与正常对照组相比,对照组的跟骨移位略有提高,但差异无显著性意义;实验组跟骨的轴向压缩应力强度达到(21.98±1.88) MPa,轴向刚度达到(1 633±150) N/mm,与正常对照组相比较差异无显著性意义(P > 0.05);③跟距关节接触力学特性:实验组跟骨聚甲基丙烯酸甲酯骨水泥注射后,Sanders Ⅲ型骨折基本上得到恢复,可见治疗效果不错;④结果表明:应用聚甲基丙烯酸甲酯骨水泥治疗跟骨Sanders Ⅲ型,具有科学有效性和临床实用性。
中图分类号:
.jpg)
.jpg)