1.1 设计 前瞻性随机对照试验,计量资料组内比较采用配对t检验,多组比较采用单因素方差分析,事后多重比较采用Bonferroni法;计数资料采用卡方检验或 Fisher 精确概率检验进行分析。
1.2 时间及地点 试验于2017 年3月至2021年4月在西南医科大学附属医院脊柱外科完成。
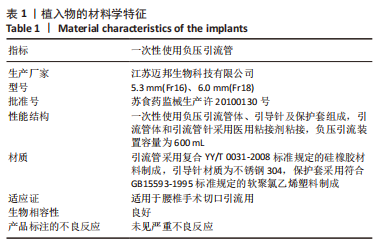
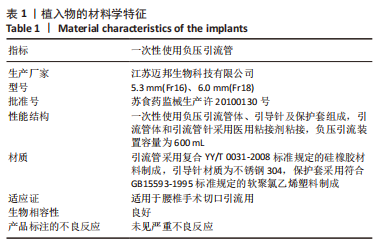
1.3 材料 一次性负压实验负压引流管介绍见表1。
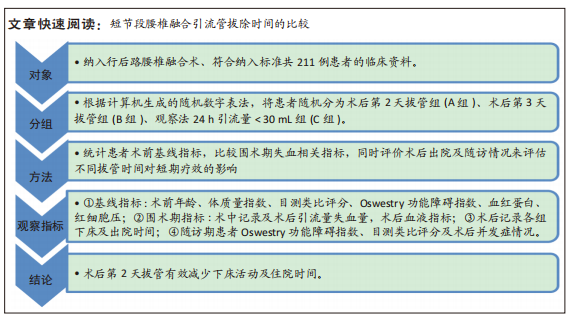
1.4 对象
纳入标准:①经病史、影像学、体格检查诊断为腰椎退行性疾病,包括腰椎间盘突出症、腰椎椎管狭窄症、腰椎不稳症等,且经保守治疗无效,需行手术治疗;②手术为经后路减压融合术,≤3个融合节段;③既往无腰椎手术史;④年龄18-80岁。
排除标准:①术前存在严重心、肺、肝、肾、血液等系统疾病;②存在凝血或出血异常,术前抗血小板和抗凝药物治疗史;③术中出现脑脊液漏或不可预知的血管、神经损伤;④长期吸烟史、类固醇使用> 6个月、糖尿病、营养不良等可能增加术后切口感染风险的疾病及因素。
剔除标准:①研究数据记载不完整,未严格执行试验方案患者;②自行退出或随访时间< 12个月患者。
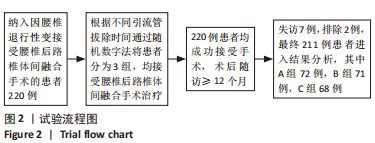
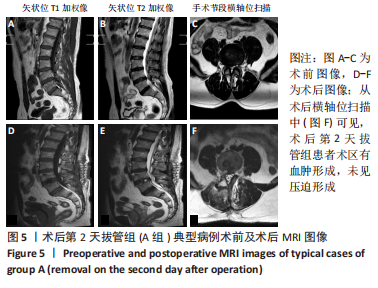
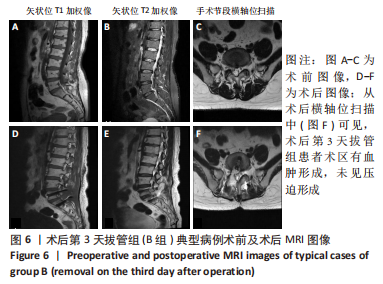
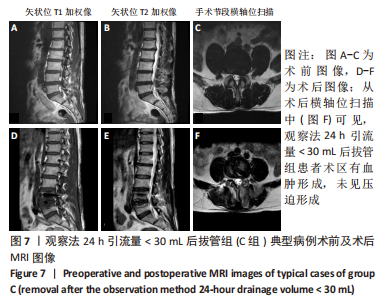
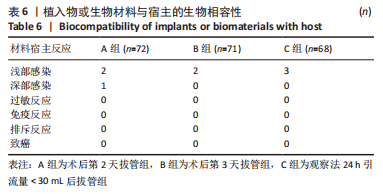
以 2017 年3月至2021年4月西南医科大学附属医院收治因腰椎退变性疾病行PLIF的患者为研究对象。220例符合选择标准纳入研究,采用计算机生成的随机数字表将患者分为术后第2天拔管组(A组)、术后第3天拔管组(B组)、观察法24 h引流量< 30 mL后拔管组(C组)。文中术后第2天为术后即刻起至第2个24 h,为了更加科学严谨,选择在间隔时间的相近时间段拔除引流管,以此类推。选择常用的一次性使用负压引流装置,为了避免不同规格的负压引流装置在初始负压值、容积之间的差异,均选择同一生产厂家,且在引流> 600 mL后由观察人员及时清倒后再进行记录。所有患者病史、影像学资料和手术方案均由同一小组高年资医生讨论完成,接受相同术后处理方案。此次研究为随机、前瞻性研究,得到了西南医科大学附属医院伦理委员会批准(批准号:KY2022143),所有患者均获得书面知情同意。
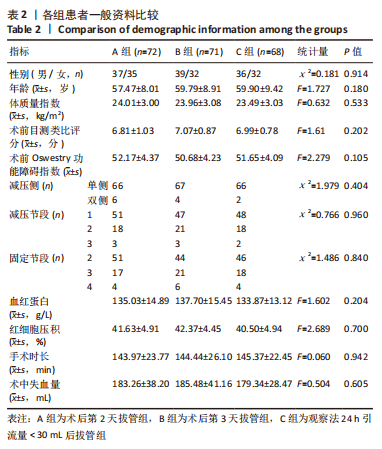
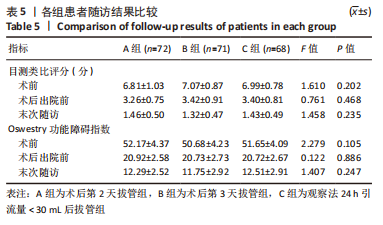
3组患者年龄、性别、体质量指数、术前下肢疼痛目测类比评分、Oswestry功能障碍指数(Oswestry disability index,ODI)、减压节段、融合节段、术前血液指标(红细胞压积、血红蛋白)、手术时长、术中失血量比较差异均无显著性意义(P > 0.05),具有可比性。
在进行该研究前对于3组干预措施分别进行了预试验,以估算样本量及观察试验可行性。分别各5例,同时根据现有的纳入标准进行,为控制偏倚均选择接受单节段PLIF。对于不同分组下疗效指标的评价,主要根据术后失血量、围术期恢复时间、并发症方面进行判断。根据3组计算得到结果效应值=0.213,在power=0.8,α=0.05的情况下,计算得出样本量为216。由于考虑到试验中不排除患者存在失访以及需要破盲的情况,调整最终样本量为220例。
经过样本量估算后,最终拟纳入220例患者,对分组进行分配隐藏。采用双盲试验方法,由发起者进行试验设计,此次试验干预人员及患者均不知情;发起者事先拟定220个研究对象序号,生成220个随机数字,在规范好入组要求后随机入组。由试验人员进行干预操作,同时记录好患者数据及信息,在规定时间内对患者进行随访。如试验过程中患者出现突发情况则需紧急揭盲,并通知试验发起者,采取积极治疗措施。
1.5 方法
1.5.1 手术方法 3组患者手术均由同一组高年资脊柱外科手术医生完成,均进行PLIF手术。气管插管全身麻醉后,将患者置于俯卧位。通过中线皮肤切开,从受累水平上方的棘突延伸至下方的棘突,然后进行剥离至筋膜。以骨膜下的方式剥离椎旁肌、椎板,上入内固定及连接装置,然后行椎板切除术,椎管和神经根管充分减压彻底。椎间植骨并放置融合器,术中C臂透视见螺钉及融合器位置满意。反复冲洗手术切口,均采用临时压迫和双极充分止血。在确认硬脑膜无撕裂、无活动性出现后,在硬膜外腔内放入封闭式负压引流管1根。逐层缝合切口,手术顺利返回病房。
1.5.2 围术期处理 术前1 h内预防性使用一代头孢抗生素至术后24 h停用。术后第1天行下肢主、被动功能锻炼预防静脉血栓,伤口常规消毒且清洁敷料覆盖至术后第10天。根据患者自身情况佩戴支具进行早期下床活动。综合评估患者术后影像学及血液指标复查、功能恢复情况、手术切口情况等均满意后安排出院。出院后1,3,6,12个月门诊复查影像学、手术切口情况。
同种异体输血适应证:输血指征未设定血红蛋白浓度或红细胞压积水平的特定值。每次输血的决定都根据患者的心血管病史、当前状态、血红蛋白水平下降、失血量和年龄判断。根据经验,血红蛋白浓度低于70-90 g/L时考虑接受同种异体输血治疗。
1.6 主要观察指标
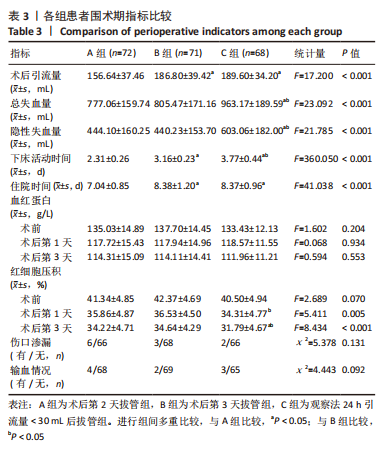
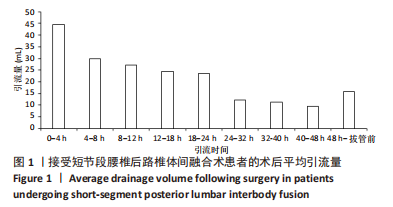
(1)失血相关指标:观察记录3组患者术后引流量(该引流量指拔管前引流装置内血液容积)。总失血量的计算:根据GROSS公式和NADEL公式可得[6-7],总失血量=全身血液量×(术前红细胞压积-术后红细胞压积)/红细胞压积均值,红细胞压积均值指术前及术后红细胞压积的平均值。全身血液量=k1×身高(m)3+k2×体质量(kg)+k3,其中男性 k1=0.366 9,k2=0.032 19,k3=0.604 1,女性 k1=0.356 1,k2=0.033 08,k3=0.183 3。隐性失血量根据SEHAT等[8]的方法计算:隐性失血量=总失血量+输血量-显性失血量。
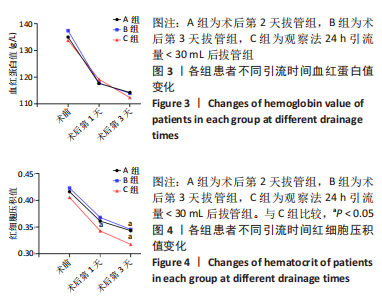
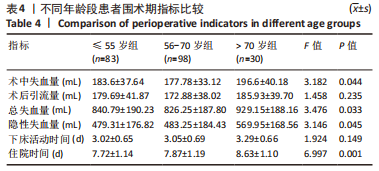
(2)血液指标:记录3组患者术后第1,3天血红蛋白、红细胞压积水平。
(3)记录围术期下床活动时间(从术后开始计算)、输血情况、并发症、住院时间、术后出院前目测类比评分和ODI,末次随访目测类比评分、ODI及伤口渗漏等并发症情况。
(4)手术部位感染定义为皮肤和皮下组织浅表感染,也可以是深部切口的持续渗液和延迟愈合。对于术后存在非机械性腰痛及发热的患者,如不排除延迟手术部位感染,则在出院后2周、1个月、3个月定期复查感染指标。
(5)随访:由5名同组成员分工完成,在住院期间对纳入的患者进行干预措施并记录详细信息后,口头及书面告知出院后注意事项,在术后1,3,6,12个月进行门诊规律随访,预留患者信息分批次进行随访。
1.7 统计学分析 采用 SPSS 23.0(IBM,NY,USA)统计软件进行分析,计量资料符合正态分布以x±s表示,组内比较采用配对t检验,多组数据比较满足方差齐性采用单因素方差分析,事后多重比较采用Bonferroni法;不满足方差齐性时采用Welch检验,事后多重比较采用Dunnett′s T3检验;计数资料以例数表示,采用卡方检验或Fisher精确概率检验进行分析。检验水准α=0.05。文章统计学方法已经西南医科大学附属医院生物统计学专家审核。