Chinese Journal of Tissue Engineering Research ›› 2023, Vol. 27 ›› Issue (14): 2291-2296.doi: 10.12307/2023.483
Introduction to the ANTI∙DF principle for diabetic foot prevention and treatment
Li Rui, Ou Xiaolan, Liu Jun, Tian Heng, Qu Wenrui, Zhu Zhe, Zhang Zhenyu, Liu Qianqian, Guo Wenlai
- Department of Hand Surgery, Second Hospital of Jilin University, Changchun 130022, Jilin Province, China
-
Received:2022-08-12Accepted:2022-08-25Online:2023-05-18Published:2022-09-30 -
Contact:Li Rui, Department of Hand Surgery, Second Hospital of Jilin University, Changchun 130022, Jilin Province, China -
About author:Li Rui, MD, Department of Hand Surgery, Second Hospital of Jilin University, Changchun 130022, Jilin Province, China
CLC Number:
Cite this article
Li Rui, Ou Xiaolan, Liu Jun, Tian Heng, Qu Wenrui, Zhu Zhe, Zhang Zhenyu, Liu Qianqian, Guo Wenlai. Introduction to the ANTI∙DF principle for diabetic foot prevention and treatment[J]. Chinese Journal of Tissue Engineering Research, 2023, 27(14): 2291-2296.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
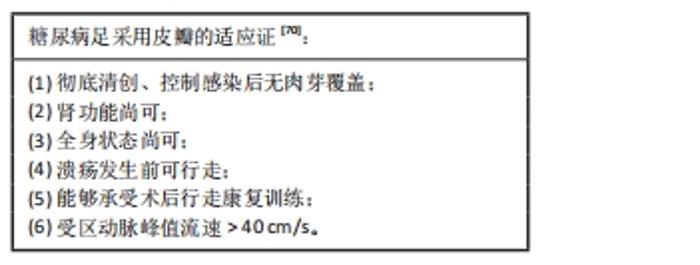
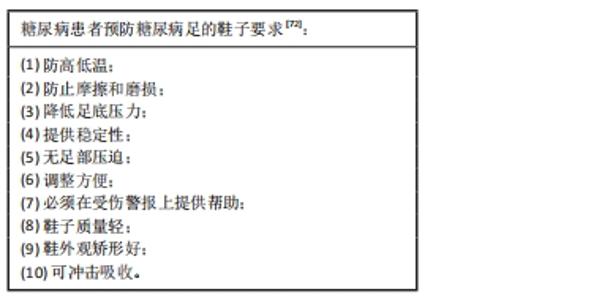
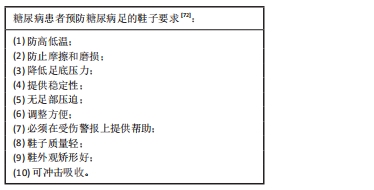
2 糖尿病引发的相关畸形(D) Diabetes mellitus-related deformities (D) 2.1 MOST形态改变就是畸形(D) 畸形(D)是MOST这4个解剖结构的形态发生改变。糖尿病足的MOST这4个解剖结构本身的形态发生改变,产生畸形(D)。肌肉(M)萎缩、缺损等变化影响肌力平衡,导致局部应力集中;骨关节(O)变化,例如骨折畸形愈合、关节脱位和关节僵硬等,导致局部应力集中;肌腱(T)粘连、挛缩也会导致局部应力集中,皮下组织(S)萎缩或变薄导致应力集中部位易破溃。 2.2 神经(N)病变导致MOST形态改变 神经(N)病变导致MOST这4个解剖结构的形态发生改变,产生畸形(D)。神经病变(N)可使足内、外在肌肉(M)萎缩、瘫痪,屈肌和伸肌平衡失调,步态改变[17];可造成夏科氏(Charcot)骨关节(O)病变[18];还可造成肌腱(T)、韧带退化;可造成皮肤及皮下组织(S)失神经营养病变变薄、萎缩等。因此导致足形态变化[畸形 (D)][19],例如爪形趾、锤状趾、跖骨头突出、拇外翻、马蹄内翻足等畸形,导致局部压力增加[5,19-22]。如马蹄足(跟腱挛缩)可造成前足底压力增加,内翻足造成足外侧压力增加,跖骨头突出可造成跖骨头下压力增加。在感觉神经病变的情况下(失去保护性感觉),在行走的过程中缺乏必要的反馈,导致行走过程中足底压力进一步增加且不被察觉,病变进一步加重[23-25]。植物(自主舒缩性)神经病变可导致皮肤出汗减少,干燥易破裂和形成裂隙[26]。因此,神经病变和机械应力升高共同作用下导致畸形、组织损伤和足部溃疡[27-28]。 2.3 动脉(A)缺血间接导致MOST形态改变 动脉(A)缺血也可影响MOST这4个解剖结构的形态,间接导致畸形(D)。例如缺血性肌肉(M)挛缩、骨关节(O)僵硬、皮下组织(S)萎缩及肌腱(T)退化等,导致形态改变,发生畸形(D)[17,29-30]。 2.4 畸形(D)导致足部溃疡(F) 2.4.1 畸形(D)导致局部应力集中 足底可分为10个基于解剖学的分区,包括足后跟的内侧、外侧,足中部,第1-5个跖骨,足拇趾,及剩余4个足趾。畸形(D)可导致足底某一分区局部压力压强峰值及累积冲量增加,持续反复的高压导致胼胝体的形成、局部组织(T)破溃坏死,继发感染(I),产生足部溃疡(F)。 2.4.2 失神经(N)保护 感觉神经病变可导致痛觉、温度觉、触觉、振动觉和位置觉的减退或丧失[1]。因此当脚受到过度压力、机械或创伤(刺伤、烫伤和擦伤)等原因导致组织(T)损伤时,在丧失保护性感觉的情况下不易被察觉[3],导致局部组织(T)进一步破溃坏死、感染(I),形成足部溃疡(F)[25],同时自主神经病变后局部血液供应减少[26],病变进一步加重,发生严重的难治性溃疡。 2.4.3 动脉(A)缺血 动脉(A)缺血导致畸形(D)局部应力集中部位更容易发生组织(T)坏死,增加感染(I)机会,产生足部溃疡(F)。而且动脉(A)缺血时,感染(I)更难控制,足部溃疡(F)更难愈合。 2.5 足部溃疡(F)治疗及预防 该课题组认为,足部溃疡(F)的预防和治疗顺序为先缓解畸形(D)造成的局部压力,改善神经(N)保护功能,改善动脉(A)供血,然后彻底清创坏死组织(T)、控制感染(I),最后闭合足部溃疡(F)。缓解畸形(D)造成的压力、改善神经(N)保护性感觉、恢复动脉(A)供血是预防及治疗的前提;清创坏死组织(T)是控制感染(I)的前提;清创坏死组织(T)和控制感染(I)是闭合足部溃疡(F)的前提。控制血糖、降压、降脂、改变生活方式(戒烟、节食、运动)等基础治疗应伴随糖尿病患者的治疗的始终。 2.5.1 缓解畸形(D)造成的局部减压(Off-loading) 外在保护性减压(Off-loading):起到暂时缓解畸形(D)造成的局部压力的作用,改善神经和血管的功能。主要方式为保守治疗:不行走(拐杖、轮椅或卧床)、减压鞋及鞋垫、毛毡减压垫、减压敷料、石膏、支具等[24,31-36]。适用于轻症,或感染尚未控制,可能造成畸形矫正手术部位感染的患者。减压应始终是预防和治疗计划的一部分[23]。 内在结构性减压(Off-loading):尽管保守治疗可取得一定的减压效果,但畸形依然存在,溃疡会反复复发。然而手术治疗既可有效减压、纠正畸形,还能防止复发,故而有效解压的主要方式为手术治疗。按部位分为足趾、跖骨、中足、后足及踝关节等的畸形矫正术;按组织器官分为MOST这4个解剖结构的畸形矫正术。肌肉(M)可行松解术、延长术及短缩术等;骨关节(O)可行截骨术、关节融合术、植骨术及关节囊及韧带松解或短缩术等[36-38];皮下组织(S)萎缩或缺损可行皮瓣转移术;肌腱(T)可行延长、短缩、移位或固定术[39]。 根据关节柔软型或半僵硬型可采取: (1)足趾畸形矫正:爪形趾、锤状趾及槌状趾等畸形可采用微创趾短屈肌腱切断术及微创趾长短屈肌腱切断术等[40-41];拇外翻可采取经皮微创Akin术及经皮微创Lapidus术等。 (2)跖骨头突出畸形矫正:可采用经皮微创跖骨远端漂浮截骨术[36]。中后足畸形矫正:包括各跗骨截骨术、融合术、关节囊及韧带松解术、肌腱移位术及肌腱固定术等[36,38]。跟腱挛缩可行腓肠肌松解术或经皮微创跟腱延长术。僵硬型可采取相应关节的融合术。 2.5.2 改善神经(N)保护功能 外在保护性减压(Off-loading):外在保护性减压同样起到暂时弥补失神经保护功能的作用。主要方式为保守治疗:不行走(拐杖、轮椅或卧床)、减压鞋及鞋垫、毛毡减压垫、减压敷料、石膏、支具等。适用于轻症,或感染尚未控制,可能造成神经手术部位感染的患者。 神经松解术:药物对糖尿病足的神经病变收效甚微。Dellon神经松解术包括腓总神经、腓深神经和胫神经松解术[42-43],常会使患者部分恢复神经保护性感觉。 2.5.3 改善动脉(A)供血 足背动脉,胫后动脉应该分别评判踝肱指数,并按照缺血程度分为4级。正常:0.8-1.3;轻度0.79-0.6;中度:0.59-0.4;重度:≤0.39[7,44]。以作者经验来看,ABI为中度时创面难以愈合,踝肱指数为重度时截肢可能性大。 感染等原因不适合手术时,可暂时使用扩血管药物,前列地尔常有一定效果。手术治疗包括腔内治疗(经皮腔内血管成形术、腔内球囊成形术)、支架植入术、血管旁路重建术、横向骨搬移和骨膜牵张等[45-51]。腔内治疗对于糖尿病足患者而言有一些局限,因为动脉常是长节段钙化、堵塞[52]。横向骨搬移或骨膜牵张术对不愿意接受或不适合其他手术的患者,有一定效果[53]。股动脉或腘动脉旁路(搭桥)手术引血到足部是目前效果最确切最持久的治疗手段。动脉旁路(搭桥)手术不但能够重建足部血供,还能同时为足部游离皮瓣供血[54]。 2.5.4 彻底清创坏死组织(T) 锐性清创:是迅速、彻底清创坏死组织的首选,可采用手术刀剪锐性清创[36,55]。此外,水刀(水动力系统)对去除生物膜很有效[56-57]。 其他降解:主要包括物理化学降解(酶)或生物讲解(蛆),适用于不愿意接受手术或全身状况不适合手术的患者、手术难以达到的深部创面或难以一次达到理想清创的创面等[55,58-59]。 2.5.5 控制感染(I) 全身应用抗生素:早期根据经验用药(可结合当地细菌谱),药敏试验结果出来后,根据药敏选用敏感药。 抗生素骨水泥:局部应用抗生素骨水泥,可迅速控制严重、顽固的深部组织感染[60]。 负压创面治疗(Negative pressure wound therapy,NPWT):常规NPWT或一次性NPWT,可有效控制感染[61-62]。抗生素骨水泥表面覆盖NPWT效果更佳。 敷料:浅表组织的较轻感染,且不愿意接受手术或全身状况不适合手术的患者,也可采用具有抗菌成分的敷料[63]。 2.5.6 闭合足部溃疡(F) 自愈:适用于基床良好的浅小创面,可采用敷料、常规NPWT或一次性NPWT等换药方法。其缺点需要良好的基床,愈合缓慢且愈合的皮肤不耐磨、不耐压(常瘢痕愈合)。如果需要4周以上的大创面,就得不偿失了。 缝合:适用于可直接缝合或拉拢延展缝合的创面。 植皮:适用于基床良好的任意大小的浅创面,愈合迅速(2周内),NPWT可提高成活率[64-66]。缺点是皮下组织薄时,不耐磨、不耐压[67]。 皮瓣:与自愈或植皮等方式相比,皮瓣治疗不需要有肉芽组织覆盖骨和肌腱的良好基床[68-69],整体基床好坏无所谓,适用范围更广。愈合时间短,2周内可愈合,愈合后耐磨、耐压,且费用低。皮瓣分为带血管蒂皮瓣和游离皮瓣,游离皮瓣的适用性更广。 然而糖尿病足患者血管条件通常较差,严重影响皮瓣的存活率。有研究汇总了18篇文献,共528例患者,总结出了糖尿病足采用皮瓣的适应证[70]。 "
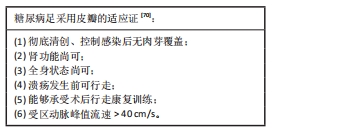
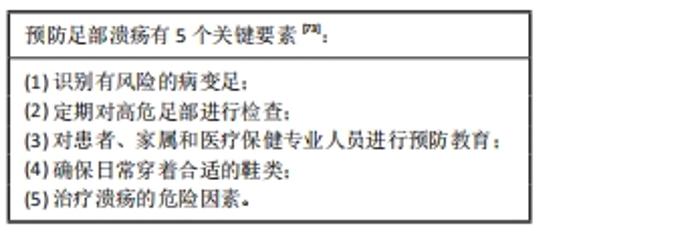
另有研究基本认同上述6条适应证,但认为尿毒症不属于禁忌证[71],只要局部有搏动良好的穿支小血管,即可皮瓣转移。该课题组采用的适应证为:术前穿支动脉超声脉峰值流速> 40 cm/s;并以术中穿支搏动良好作为金标准。 当足部没有受区供血动脉时,可以采用股动脉或腘动脉旁路(搭桥)手术引血到足部,重建足部血运的同时,为足部游离皮瓣供血。 3 糖尿病足的防治建议 Suggestions for diabetic foot prevention and treatment 国际糖尿病联盟(International Diabetes Federation,IDF)2017年发布的“IDF临床实践建议:糖尿病足”指南中显示,糖尿病足的病因包括周围神经病变、外周动脉疾病和感染[72]。除了这3个因素中的任何一个外,还可以增加创伤因素,最常见的创伤原因是使用不合适的鞋子和/或鞋垫。 3.1 预防糖尿病足部溃疡 国际糖尿病足工作组(International Working Group on the Diabetic Foot,IWGDF)在2019年发布“IWGDF实践指南:糖尿病足的预防和管理”明确指出如何预防糖尿病足[73]。一个经过适当培训的医疗专业人员团队应解决这5个要素,以此进行足部溃疡高风险人群的综合预防管理。 "
3.3 早期周围神经(N)病变的预防 周围神经(N)病变是糖尿病最常见的并发症。糖尿病周围神经(N)病变是全身神经的损伤,可以改变自主神经、运动和感觉功能。运动型周围神经病变最重要的结果是足部内在肌肉的去神经支配,这会破坏脚趾屈伸肌之间的正常平衡,导致常见的糖尿病足畸形(D)。这种畸形会增加某些部位的压力,导致皮下血肿及老茧形成,如果不及时发现和治疗,就会产生溃疡。 早期发现周围神经(N)病变的重要性在于按危险类别对目标人群进行分类,并根据类别组织随访策略(可能从高风险类别的每月访问变为低风险类别的每年访问)。通过非常具体的建议和建议教育患者如何预防伤害是预防周围神经(N)病变的关键。例如,教育患者:正确切割脚趾甲的方法;适当的温度洗脚;脚趾间使用湿润剂;赤脚走路的危害;日常使用前对鞋子进行充分检查,寻找里面是否有异物;使用无压迫性、颜色清晰的棉袜等[72]。 3.4 周围血管[动脉(A)]疾病的预防 对所有糖尿病患者进行充分的定期外周血管评估对于早期发现周围血管[动脉(A)]疾病是必不可少的,并且该评估必须至少包括:脉搏触诊、踝臂指数和多普勒超声检查。此外,预防和/或治疗周围血管[动脉(A)]疾病的重要措施之一是运动。有研究表明,每天步行30 min,每周至少5次,可使远端组织氧合率增加30%[72]。 "

| [1] FELDMAN EL, NAVE KA, JENSEN TS, et al. New horizons in diabetic neuropathy: mechanisms, bioenergetics, and pain. Neuron. 2017;93(6):1296-1313. [2] GONCALVES NP, VAEGTER CB, ANDERSEN H, et al. Schwann cell interactions with axons and microvessels in diabetic neuropathy. Nat Rev Neurol. 2017;13(3):135-147. [3] FELDMAN EL, CALLAGHAN BC, POP-BUSUI R, et al. Diabetic neuropathy. Nat Rev Dis Primers. 2019;5(1):42. [4] SLOAN G, SELVARAJAH D, TESFAYE S. Pathogenesis, diagnosis and clinical management of diabetic sensorimotor peripheral neuropathy. Nat Rev Endocrinol. 2021;17(7):400-420. [5] SAEEDI P, PETERSOHN I, SALPEA P, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract. 2019;157:107843. [6] ALAVI A, SIBBALD RG, MAYER D, et al. Diabetic foot ulcers: Part I. Pathophysiology and prevention. J Am Acad Dermatol. 2014;70(1):1.e1-e18; quiz 19-20. [7] MONTEIRO-SOARES M, RUSSELL D, BOYKO EJ, et al. Guidelines on the classification of diabetic foot ulcers (IWGDF 2019). Diabetes Metab Res Rev. 2020;36 Suppl 1:e3273. [8] PECORARO RE, REIBER GE, BURGESS EM. Pathways to diabetic limb amputation - basis for prevention. Diabetes Care. 1990;13(5):513-521. [9] JEFFCOATE WJ, VILEIKYTE L, BOYKO EJ, et al. Current challenges and opportunities in the prevention and management of diabetic foot ulcers. Diabetes Care. 2018;41(4):645-652. [10] ARMSTRONG DG, SWERDLOW MA, ARMSTRONG AA, et al. Five year mortality and direct costs of care for people with diabetic foot complications are comparable to cancer. J Foot Ankle Res. 2020;13(1):16. [11] WILLIAMS DT, PRICE P, HARDING KG. Amputation and mortality in new-onset diabetic foot ulcers stratified by etiology. Diabetes Care. 2003;26(11):3199-3200. [12] LAVERY LA, ASHRY HR, VANHOUTUM W, et al. Variation in the incidence and proportion at diabetes-related amputations in minorities. Diabetes Care. 1996;19(1):48-52. [13] SUN Y, GAO Y, CHEN J, et al. Evidence mapping of recommendations on diagnosis and therapeutic strategies for diabetes foot: an international review of 22 guidelines. Metabolism. 2019;100:153956. [14] MOORE Z, CARVILLE K, WEIR D, et al. Consensus document strategies to reduce practice variation in wound assessment and management. 2020. [15] SCHULTZ GS, SIBBALD RG, FALANGA V, et al. Wound bed preparation: a systematic approach to wound management. Wound Repair Regen. 2003;11(2):S1-S28. [16] GUARRO G, COZZANI F, ROSSINI M, et al. The modified TIME-H scoring system, a versatile tool in wound management practice:a preliminary report. Acta Biomed. 2021;92(4):e2021226. [17] ORLANDO G, BALDUCCI S, BAZZUCCHI I, et al. Neuromuscular dysfunction in type 2 diabetes:underlying mechanisms and effect of resistance training. Diabetes Metab Res Rev. 2016;32(1):40-50. [18] ORLANDO G, REEVES ND, BOULTON AJM, et al. Sedentary behaviour is an independent predictor of diabetic foot ulcer development: an 8-year prospective study. Diabetes Res Clin Pract. 2021;177:108877. [19] ARMSTRONG DG, BOULTON AJM, BUS SA. Diabetic foot ulcers and their recurrence. New Engl J Med. 2017;376(24):2367-2375. [20] JEYAM A, MCGURNAGHAN SJ, BLACKBOURN LAK, et al. Diabetic neuropathy is a substantial burden in people with type 1 diabetes and is strongly associated with socioeconomic disadvantage: a population-representative study from scotland. Diabetes Care. 2020;43(4):734-742. [21] ESTHER CL, BELEN O AA, ARANZAZU RM, et al. Foot deformities in patients with diabetic mellitus (with and without peripheral neuropathy). J Tissue Viability. 2021;30(3):346-351. [22] MOLINES-BARROSO RJ, LAZARO-MARTINEZ JL, ARAGON-SANCHEZ FJ, et al. Forefoot ulcer risk is associated with foot type in patients with diabetes and neuropathy. Diabetes Res Clin Pract. 2016;114:93-98. [23] BUS SA. The role of pressure offloading on diabetic foot ulcer healing and prevention of recurrence. Plast Reconstr Surg. 2016;138: 179S-187S. [24] BUS SA, ARMSTRONG DG, GOODAY C, et al. Guidelines on offloading foot ulcers in persons with diabetes (IWGDF 2019 update). Diabetes Metab Res Rev. 2020;36 Suppl 1:e3274. [25] WUKICH DK, ARMSTRONG DG, ATTINGER CE, et al. Inpatient management of diabetic foot disorders: a clinical guide. Diabetes Care. 2013;36(9):2862-2871. [26] LEPANTALO M, APELQVIST J, SETACCI C, et al. Diabetic foot. Eur J Vasc Endovasc Surg. 2011;42:S60-S74. [27] MASSON EA, HAY EM, STOCKLEY I, et al. Abnormal foot pressures alone may not cause ulceration. Diabetic Medicine. 1989;6(5):426-428. [28] VEVES A, MURRAY HJ, YOUNG MJ, et al. The risk of foot ulceration in diabetic-patients with high foot pressure -a prospective-study. Diabetologia. 1992;35(7):660-663. [29] KOUTAKIS P, WEISS DJ, MISERLIS D, et al. Oxidative damage in the gastrocnemius of patients with peripheral artery disease is myofiber type selective. Redox Biol. 2014;2:921-928. [30] ROBBINS JL, JONES WS, DUSCHA BD, et al. Relationship between leg muscle capillary density and peak hyperemic blood flow with endurance capacity in peripheral artery disease. J Appl Physiol. 2011; 111(1):81-86. [31] BUS SA, ARMSTRONG DG, VAN DEURSEN RW, et al. IWGDF guidance on footwear and offloading interventions to prevent and heal foot ulcers in patients with diabetes. Diabetes Metab Res Rev. 2016;32:25-36. [32] VAN NETTEN JJ, LAZZARINI PA, ARMSTRONG DG, et al. Diabetic Foot Australia guideline on footwear for people with diabetes. J Foot Ankle Res. 2018;11:2. [33] LAVERY LA, LAFONTAINE J, HIGGINS KR, et al. Shear-reducing insoles to prevent foot ulceration in high-risk diabetic patients. Adv Skin Wound Care. 2012;25(11):519-524. [34] RIZZO L, TEDESCHI A, FALLANI E, et al. Custom-made orthesis and shoes in a structured follow-up program reduces the incidence of neuropathic ulcers in high-risk diabetic foot patients. Int J Lower Extrem Wounds. 2012;11(1):59-64. [35] SCIRE V, LEPORATI E, TEOBALDI L, et al. Effectiveness and safety of using podikon digital silicone padding in the primary prevention of neuropathic lesions in the forefoot of diabetic patients. J Am Podiat Med Assn. 2009;99(1):28-34. [36] KILICOGLU OI, DEMIREL M, AKTAS S. New trends in the orthopaedic management of diabetic foot. Efort Open Rev. 2018;3(5):269-277. [37] FAGLIA E, CLERICI G, CAMINITI M, et al. Feasibility and effectiveness of internal pedal amputation of phalanx or metatarsal head in diabetic patients with forefoot osteomyelitis. J Foot Ankle Surg. 2012;51(5):593-598. [38] YAMMINE K, ASSI C. Surgical offloading techniques should be used more often and earlier in treating forefoot diabetic ulcers: an evidence-based review. Int J Lower Extrem Wounds. 2020;19(2):112-119. [39] MESHKIN DH, FAGOTHAMAN K, ARNESON J, et al. Plantar foot ulcer recurrence in neuropathic patients undergoing percutaneous tendo-achilles lengthening. J Foot Ankle Surg. 2020;59(6):1177-1180. [40] TAMIR E, VIGLER M, AVISAR E, et al. Percutaneous tenotomy for the treatment of diabetic toe ulcers. Foot Ankle Int. 2014;35(1):38-43. [41] TAMIR E, MCLAREN AM, GADGIL A, et al. Outpatient percutaneous flexor tenotomies for management of diabetic claw toe deformities with ulcers:a preliminary report. Canadian J Surg. 2008;51(1):41-44. [42] CHAUDHRY V, RUSSELL J, BELZBERG A. Decompressive surgery of lower limbs for symmetrical diabetic peripheral neuropathy. Cochrane Database Syst Rev. 2008(3):CD006152. [43] DELLON AL. Treatment of symptomatic diabetic neuropathy by surgical decompression of multiple peripheral nerves. Plastic Reconstr Surg. 1992;89(4):689-697; discussion 98-99. [44] HINCHLIFFE RJ, BROWNRIGG JRW, APELQVIST J, et al. IWGDF guidance on the diagnosis, prognosis and management of peripheral artery disease in patients with foot ulcers in diabetes. Diabetes Metab Res Rev. 2016;32:37-44. [45] WECK M, SLESACZECK T, PAETZOLD H, et al. Structured health care for subjects with diabetic foot ulcers results in a reduction of major amputation rates. Cardiovasc Diabetol. 2013;12:45. [46] CHAN P, STUART W, HINCHLIFFE R. New reporting standards are required to assess the impact of vascular intervention on patients with diabetic foot ulceration. Eur J Vasc Endovasc Surg. 2015;50(2):139-140. [47] MILLS JL. Lower limb ischaemia in patients with diabetic foot ulcers and gangrene:recognition, anatomic patterns and revascularization strategies. Diabetes Metab Res Rev. 2016;32:239-245. [48] 王江宁,高磊.糖尿病足慢性创面治疗的新进展[J].中国修复重建外科杂志,2018,32(7):832-837. [49] CHEN Y, KUANG X, ZHOU J, et al. Proximal tibial cortex transverse distraction facilitating healing and limb salvage in severe and recalcitrant diabetic foot ulcers. Clin Orthop Relat Res. 2019;478(4):1. [50] 赵劲民,李刚.胫骨横向骨搬移技术治疗糖尿病足的专家共识(2020)[J].中国修复重建外科杂志,2020,34(8):945-950. [51] 刘杰,花奇凯,李山郎,等.骨膜牵张技术用于糖尿病足治疗的理论基础及临床结果验证[J]. 中国组织工程研究,2022,26(32):5236-5241. [52] CAVANAGH PR, LIPSKY BA, BRADBURY AW, et al. Treatment for diabetic foot ulcers. Lancet. 2005;366(9498):1725-1735. [53] 王斌,刘伟,霍永新,等.股-股动脉旁路移植联合胫骨横向骨搬移术治疗下肢动脉硬化闭塞症或合并糖尿病足[J].中国修复重建外科杂志,2018,32(12):1576-1580. [54] CHANG CH, HUANG CC, HSU H, et al. Editor’s choice - diabetic limb salvage with endovascular revascularisation and free tissue transfer:long-term follow up. Eur J Vasc Endovasc Surg. 2019;57(4):527-536. [55] DAYYA D, O’NEILL OJ, HUEDO-MEDINA TB, et al. Debridement of Diabetic Foot Ulcers. Adv Wound Care (New Rochelle). 2021. doi: 10.1089/wound.2021.0016. [56] LIU JQ, GE YN, WANG Q, et al. Waterjet in bacterial clearance of diabetic lower extremity contaminated wounds: a retrospective cohort study. Int J Low Extrem Wounds. 2021. doi: 10.1177/15347346211024204. [57] 陈小丽,郑焱玲,曹茂华,等.超声水刀清创系统辅助治疗糖尿病足部皮肤溃疡的观察[J].局解手术学杂志,2013,22(1):78-79. [58] PAJARILLO C, SHERMAN RA, SHERIDAN R, et al. Health professionals’ perceptions of maggot debridement therapy. J Wound Care. 2021; 30(Sup9a):VIIi-VIIxi. [59] CEROVSKY V, BEM R. Lucifensins, the insect defensins of biomedical importance:the story behind maggot therapy. Pharmaceuticals. 2014; 7(3):251-264. [60] EHYA REM, ZHANG H, QI BW, et al. Application and clinical effectiveness of antibiotic-loaded bone cement to promote soft tissue granulation in the treatment of neuropathic diabetic foot ulcers complicated by osteomyelitis: a randomized controlled trial. J Diabetes Res. 2021; 2021:9911072. [61] JI SZ, LIU XB, HUANG J, et al. Consensus on the application of negative pressure wound therapy of diabetic foot wounds. Burns Trauma. 2021; 9:tkab018. [62] BORYS S, HOHENDORFF J, FRANKFURTER C, et al. Negative pressure wound therapy use in diabetic foot syndrome-from mechanisms of action to clinical practice. Eur J Clin Invest. 2019;49(4):e13067. [63] ANDREWS KL, HOUDEK MT, KIEMELE LJ. Wound management of chronic diabetic foot ulcers: from the basics to regenerative medicine. Prosthet Orthot Int. 2015;39(1):29-39. [64] SANTEMA TB, POYCK PPC, UBBINK DT. Skin grafting and tissue replacement for treating foot ulcers in people with diabetes. Cochrane Database Syst Rev. 2016;2(2):CD011255. [65] TZENG YS, DENG SC, WANG CH, et al. Treatment of nonhealing diabetic lower extremity ulcers with skin graft and autologous platelet gel: a case series. Biomed Res Int. 2013;2013:837620. [66] GKOTSOULIAS E. Split thickness skin graft of the foot and ankle bolstered with negative pressure wound therapy in a diabetic population: the results of a retrospective review and review of the literature. Foot Ankle Spec. 2020;13(5):383-391. [67] JEON H, KIM J, YEO H, et al. Treatment of diabetic foot ulcer using matriderm in comparison with a skin graft. Arch Plast Surg. 2013;40(4): 403-408. [68] BATTISTON B, CICLAMINI D, TANG JB. Compound or specially designed flaps in the lower extremities. Clin Plast Surg. 2020;47(4):535-546. [69] KWON JG, CHO MJ, PAK CJ, et al. A retrospective case series on free flap reconstruction for ischemic diabetic foot: the nutrient flap further explained. Plast Reconstr Surg. 2022;149(6):1452-1461. [70] O’CONNOR EJF, VESELY M, HOLT PJ, et al. A systematic review of free tissue transfer in the management of non-traumatic lower extremity wounds in patients with diabetes. Eur J Vasc Endovasc Surg. 2011; 41(3):391-399. [71] KOTHA VS, FAN KL, SCHWITZER JA, et al. Amputation versus free flap:long-term outcomes of microsurgical limb salvage and risk factors for amputation in the diabetic population. Plast Reconstr Surg. 2021; 147(3):742-750. [72] IBRAHIM A. IDF Clinical practice recommendation on the diabetic foot: a guide for healthcare professionals. Diabetes Res Clin Pract. 2017; 127:285-287. [73] SCHAPER NC, VAN NETTEN JJ, APELQVIST J, et al. Practical Guidelines on the prevention and management of diabetic foot disease (IWGDF 2019 update). Diabetes Metab Res Rev. 2020;36 Suppl 1:e3266. |
| [1] | Nong Fuxiang, Jiang Zhixiong, Li Yinghao, Xu Wencong, Shi Zhilan, Luo Hui, Zhang Qinglang, Zhong Shuang, Tang Meiwen. Bone cement augmented proximal femoral nail antirotation for type A3.3 intertrochanteric femoral fracturalysis [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(在线): 1-10. |
| [2] | Yang Jiujie, Li Zhi, Wang Shujie, Tian Ye, Zhao Wei. Intraoperative neurophysiological monitoring of functional changes following durotomy with decompression for acute spinal cord injury [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(8): 1232-1236. |
| [3] | Song Hehua, Wei Zairong. Diabetic peripheral neuropathy: research and therapy [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(8): 1278-1285. |
| [4] | Zhao Wei, Feng Wei, Yang Tieyi, Ren Wei, Wang Yuxin, Lyu Huicheng, Chang Zhiqiang, Feng Xiaodong, Wang Ziheng, Guo Shibing. Antibiotic bone cement intramedullary nail prepared using 3D printed mold for the treatment of long bone infection in lower limbs [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(7): 1023-1030. |
| [5] | Xu Qijing, Yang Yichun, Lei Wei, Yang Ying, Yu Jiang, Xia Tingting, Zhang Meng, Zhang Tao, Zhang Qian. Advances and problems in cell-free treatment of diabetic skin chronic wounds [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(6): 962-969. |
| [6] | Zhou Jie, Pei Xibo, Wan Qianbing. Advances and biological application of asymmetric dressings [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(3): 434-440. |
| [7] | Wang Kaiyu, Hu Peng, Wei Zairong, Huang Guangtao, Zhou Jian, He Guijia, Nie Kaiyu. Use of expanders and implants in breast reconstruction complicated with infection [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(3): 461-469. |
| [8] | Han Tao, Hao Jianqiang, Li Wenbo, Shi Jie, Gao Qiuming. Advantages and problems of antibiotic-loaded bone cements for bone and joint infections [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(3): 470-477. |
| [9] | Li Mingxiu, Wang Xuan, Yang Jie, Li Yi. An osteoarthritis model in vitro: characteristics and new design idea [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(2): 300-306. |
| [10] | Liu Xiaoyun, Deng Yuping, Li Feifei, Zhao Dongliang, Yang Yang, Huang Tao, Tan Wenchang, Wu Yaobin, Huang Wenhua, Li Yanbing. Effect of elastin degradation of patellar tendon on the quasi-static tensile mechanical properties [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(18): 2831-2836. |
| [11] | Wang Yuesheng, Gao Wei, Peng Cheng. Surface treatment of dental implant materials and their antibacterial and osteoinductive ability [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(12): 1961-1968. |
| [12] | Hu Jinlong, Quan Huahong, Wang Jingcheng, Zhang Pei, Zhang Jiale, Chen Pengtao, Liang Yuan. Effect of copper sulfide nanoparticles loaded thermosensitive hydrogel Pluronic F127 on infected wound healing in rats [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(12): 1927-1931. |
| [13] | Huang Chuwen, Jiang Hua, Li Minqing. Complications and death causes of peripheral blood stem cell transplantation in the treatment of thalassemia major [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(1): 42-48. |
| [14] | Lu Pan, Zhang Chunlin, Wang Yongkui, Yan Xu, Dong Chao, Yue Yisen, Li Long, Zhu Andi. Volume changes of cervical herniated discs after open-door laminoplasty and conservative treatment as assessed by three-dimensional volume method [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1395-1401. |
| [15] | Lu Qinxue, Xu Ning, Yang Yinglan, Han Qianqian, Duanmu Xianyu, Guo Yuwei, Han Qing. Femoroacetabular impingement: strength trainings for nerve-muscle, peripheral muscle and core muscle [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(5): 786-791. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||