Design
A retrospective case analysis.
Time and setting
The study was done between October 2012 and August 2013 at the Second Department of Orthopedics, Hospital of Traditional Chinese Medicine, Xinjiang Medical University, China.
Subjects
Three males and five females were diagnosed as arthritis of the knee accompanied with ipsilateral femoral extra-articular deformity and treated by one-stage total knee arthroplasty . The age ranged from 49 to 82 years (average
65.8 years). All operations were done by the same work team. There were five patients with compensatory intra-articular osteotomy and three with extra-articular osteotomy. Posterior stability prostheses were used in all patients with a constraited insert in three patients (Table 1).
.jpg)
Diagnostic criteria: Refer to the relevant contents of “Diagnosis and treatment of osteoarthritis (Chinese Orthopaedic Association-2010)” for diagnosis of osteoarthritis[8]. Make diagnosis of articular deformity of femur according to lower extremity weight-bearing radiography.
Inclusion criteria: ①meeting these diagnostic criteria;
②one-stage total knee arthroplasty; ③ Ⅲ-Ⅳ level according to Kellgren-Lawrence X-ray grading system[9];
④understanding the purpose of operation and cooperation.
Exclusion criteria: ①poor compliance; ②difficult to make exact evaluate with related disorder of other diseases.
Methods
Preoperative plan
Preoperative planning usually includes the following aspects: assessing surgical risk (indications and contraindications), selection of the prosthesis, the measurement of prosthesis size, preparation of the skin, application of tourniquet, choice of incision and application of prophylactic antibiotic. It is emphasized that comprehensive physical examination helped to evaluate soft-tissues balance, and thorough imaging studies especially preoperative full-length weight-bearing radiograph of the lower extremity were made in preoperative plan[10]. Extra-articular corrective osteotomy was performed if the femoral condylar resection violated the integrity of the insertion of either the medial or the lateral collateral ligament. Otherwise, intra-articular osteotomy was the option. Patients’ complaints and demands for life style were involved in the plan. As this group of patients were old, had low activity demands and cannot tolerant two consecutive operations or more, we prone to one-stage operation, instead of two steps (one-stage osteotomy and two-stage total knee arthroplasty after healing).
Surgical technique
Parapatellar medial approach and extra-medullary guide system were used in all cases. According to the preoperative plan, intra-articular compensatory osteotomy was done in five patients. As for extra-articular osteotomy fixtures were fixed first. The osteotomy of front and rear sides of condylar surface should adjust to the patellofemoral trajectory line to gain good angular rotation. We selected plate or intramedullary nail fixation for extra-articular osteotomy. Soft-tissues balancing techniques were considered after clearance of intra-articular osteophyte. We used pie-crusting technique in one valgus knee and two varus knees for the contracture collateral ligaments. We used sliding osteotmy technique in one patient for posterior lateral instability after routine osteotomy. Important blood vessels, nerves, and other soft tissue structures were protected through. Retractors were placed correctly, avoiding excessive traction.
Five patients (No. 1, 3, 4, 6, 7) underwent intra-articular one-stage compensatory osteotomy and total knee arthroplasty, three patients (No. 2, 5, 8) underwent extra-articular osteotomy and total knee arthroplasty, with lateral plate fixed in No. 2 and bilateral plates in No. 5 and intramedullar nail in No. 8. Three patients (No. 1, 3, 5) adjusted the level of the distal osteotomy as insufficient in first time. Extensive release of medial soft-tissue complex and tighten of lateral soft-tissue complex were needed in seven varus knees (No. 1, 2, 3, 4, 6, 7, 8) and one screw was used for tightening medial collateral ligament through clipping osteotomy to attain the soft tissue balancing. A quadricepsplasty was performed in one knee of extension contracture due to quadriceps fibrosis after fracture (No. 5). Four buckling knees (No. 1, 3, 6, 7) and one anti-sheets knee were adjusted by inclination of prosthesis in sagittal plane. All knees were replaced with the PS prosthesis.
Postoperative follow-up
Routine treatment includes prophylactic antibiotic, gastrointestinal mucosal agents and local cryotherapy for 24-48 hours, anticoagulant for 2-3 weeks, multiple-model analgesics. Recovery training went on for 2-4 weeks. Chuck brace of knee was used for patients with postoperative ligament dysfunction.
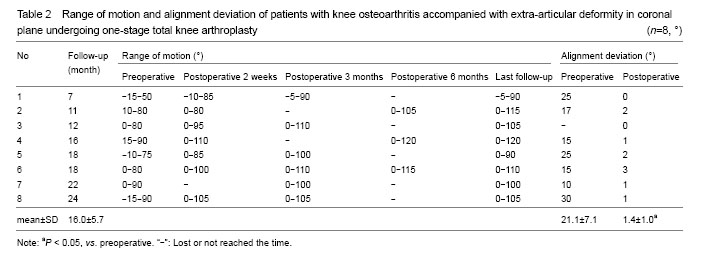
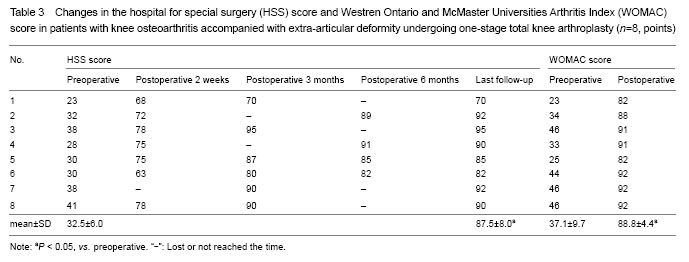
Main outcome measure
The hospital for special surgery score[11], Western Ontario and McMaster Universities Arthritis Index[12], alignments deviation and X-ray were main assessment markers for all patients. Radiographs were performed with patients positioned in a method based on the recommendations described by Cooke et al [13-14]. For the weight bearing AP radiograph, the patient was placed in the standing position with their backside against the cassette. The feet were positioned together or slightly separated in order to provide good balance. The central ray was directed perpendicular to the joint space between the patella and femoral condyles. The central ray was directed perpendicular to the film.
Clinical and functional evaluations were recorded at 2 weeks, 3 months, 6 months and 1 year according to the hospital for special surgery score and Western Ontario and McMaster Universities Arthritis Index score postoperatively; and every yearly follow-up face to face, or by telephone at least.
Statistical analysis
All data were analyzed using SPSS 17.0 software. Two sample t-test was utilized for the hospital for special surgery score, Westren Ontario and McMaster Universities Arthritis Index score and alignment deviation before and after surgery, and test level α = 0.05.
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)