[1] POH PS, LINGNER T, KALKHOF S, et al. Enabling technologies towards personalization of scaffolds for large bone defect regeneration. Curr Opin Biotechnol. 2022;74:263-270.
[2] SHI H, ZHOU Z, LI W, et al. Hydroxyapatite based materials for bone tissue engineering: A brief and comprehensive introduction. Crystals. 2021;11(2):149.
[3] BALDWIN P, LI D J, AUSTON DA, et al. Autograft, allograft, and bone graft substitutes: clinical evidence and indications for use in the setting of orthopaedic trauma surgery. J Orthop Trauma. 2019;33(4):203-213.
[4] WANG W, YEUNG KW. Bone grafts and biomaterials substitutes for bone defect repair: A review. Bioact Mater. 2017;2(4):224-247.
[5] BALDINI N, DE SANCTIS M, FERRARI M. Deproteinized bovine bone in periodontal and implant surgery. Dent Mater. 2011;27(1):61-70.
[6] PERIĆ KAČAREVIĆ Z, KAVEHEI F, HOUSHMAND A, et al. Purification processes of xenogeneic bone substitutes and their impact on tissue reactions and regeneration. Int J Artif Organs. 2018;41(11):789-800.
[7] RODRÍGUEZ-LUGO V, KARTHIK T, MENDOZA-ANAYA D, et al. Wet chemical synthesis of nanocrystalline hydroxyapatite flakes: effect of pH and sintering temperature on structural and morphological properties. R Soc Open Sci. 2018;5(8):180962.
[8] SARTORI S, SILVESTRI M, FORNI F, et al. Ten‐year follow‐up in a maxillary sinus augmentation using anorganic bovine bone (Bio‐Oss). A case report with histomorphometric evaluation. Clin Oral Implants Res. 2003;14(3):369-372.
[9] MATHINA M, SHINYJOY E, KAVITHA L, et al. A comparative study of naturally and synthetically derived bioceramics for biomedical applications. Mater Today Proc. 2020;26:3600-3603.
[10] 李忠杰,李绍波.磷酸钙人工骨修复骨缺损的研究进展[J].生物骨科材料与临床研究,2021,18(4): 87-91.
[11] GEORGE SM, NAYAK C, SINGH I, et al. Multifunctional hydroxyapatite composites for orthopedic applications: a review. ACS Biomater Sci Eng. 2022;8(8):3162-3186.
[12] YUAN H, VAN BLITTERSWIJK C, DE GROOT K, et al. A comparison of bone formation in biphasic calcium phosphate (BCP) and hydroxyapatite (HA) implanted in muscle and bone of dogs at different time periods. J Biomed Mater Res A. 2006;78(1):139-147.
[13] SCALERA F, GERVASO F, SANOSH K, et al. Influence of the calcination temperature on morphological and mechanical properties of highly porous hydroxyapatite scaffolds. Ceram Int. 2013;39(5):4839-4846.
[14] ZHENG Y, WU G, LIU T, et al. A novel BMP2‐coprecipitated, layer‐by‐layer assembled biomimetic calcium phosphate particle: A biodegradable and highly efficient osteoinducer. Clin Implant Dent Relat Res. 2014;16(5):643-654.
[15] LIU T, ZHENG Y, WU G, et al. BMP2-coprecipitated calcium phosphate granules enhance osteoinductivity of deproteinized bovine bone, and bone formation during critical-sized bone defect healing. Sci Rep. 2017;7(1):1-12.
[16] XU G, SHEN C, LIN H, et al. Development, in-vitro characterization and in-vivo osteoinductive efficacy of a novel biomimetically-precipitated nanocrystalline calcium phosphate with internally-incorporated bone morphogenetic protein-2. Front Bioeng Biotechnol. 2022;10: 920696.
[17] WAN B, RUAN Y, SHEN C, et al. Biomimetically precipitated nanocrystalline hydroxyapatite. Nano TransMed. 2022;1(2-4):e9130008.
[18] DUAN R, BARBIERI D, LUO X, et al. Variation of the bone forming ability with the physicochemical properties of calcium phosphate bone substitutes. Biomater Sci. 2018; 6(1):136-145.
[19] ZHU X, FAN H, XIAO Y, et al. Effect of surface structure on protein adsorption to biphasic calcium-phosphate ceramics in vitro and in vivo. Acta Biomater. 2009;5(4):1311-1318.
[20] LI X, DENG Y, CHEN X, et al. Gelatinizing technology combined with gas foaming to fabricate porous spherical hydroxyapatite bioceramic granules. Mater Lett. 2016;185: 428-431.
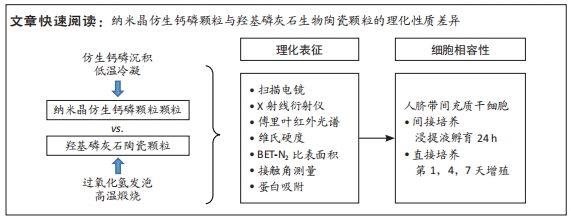
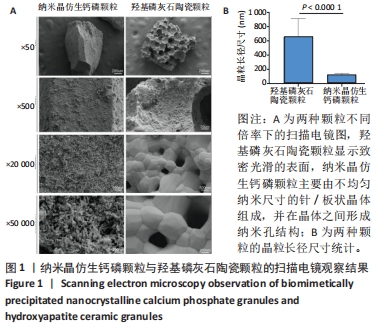
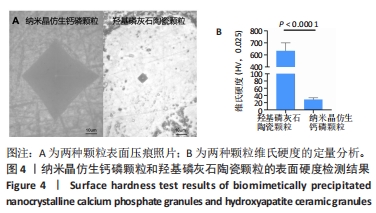
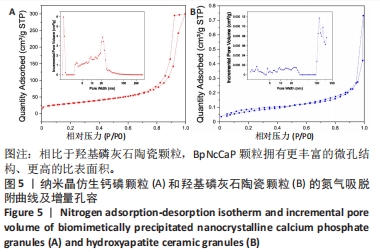
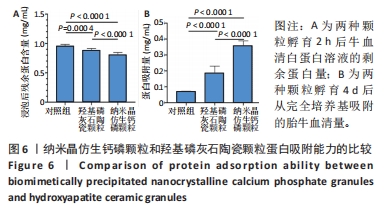
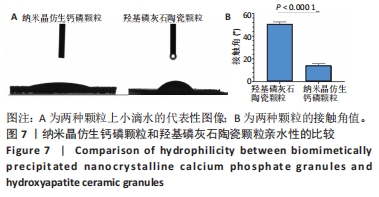
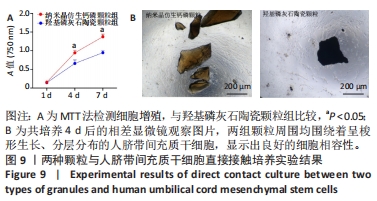
[21] XU G, WANG T, SHEN C, et al. In-vitro physicochemical characterization of a novel type of bone-defect-filling granules-BpNcCaP in comparison to deproteinized bovine bone (Bio-Oss®). Nano TransMed. 2023;2(1):e9130016.
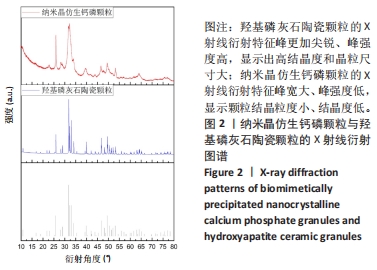
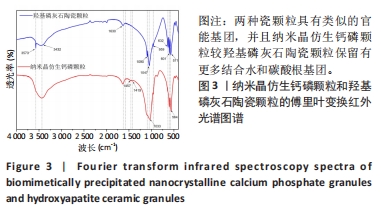
[22] ŚLÓSARCZYK A, PASZKIEWICZ Z, PALUSZKIEWICZ C. FTIR and XRD evaluation of carbonated hydroxyapatite powders synthesized by wet methods. J Mol Struct. 2005;744:657-661.
[23] 陈鹏.结晶度对羟基磷灰石成骨和骨诱导性影响的研究[D].广州:华南理工大学, 2019.
[24] DALL’ARA E, ÖHMAN C, BALEANI M, et al. The effect of tissue condition and applied load on Vickers hardness of human trabecular bone. J Biomech. 2007;40(14):3267-3270.
[25] ZHU W, IMAMURA H, MARIN E, et al. Effects of annealing in air on microstructure and hardness of hydroxyapatite ceramics. J Phys D Appl Phys. 2021;54(31):315301.
[26] XU Z, LIU C, WEI J, et al. Effects of four types of hydroxyapatite nanoparticles with different nanocrystal morphologies and sizes on apoptosis in rat osteoblasts. J Appl Toxicol. 2012;32(6):429-435.
[27] PATEL N, GIBSON IR, KE S, et al. Calcining influence on the powder properties of hydroxyapatite. J Mater Sci Mater Med. 2001;12:181-188.
[28] ONI OP, HU Y, TANG S, et al. Syntheses and applications of mesoporous hydroxyapatite: a review. Mater Chem Front. 2023;7:9-43.
[29] CHAKRABORTY PK, ADHIKARI J, SAHA P. Variation of the properties of sol–gel synthesized bioactive glass 45S5 in organic and inorganic acid catalysts. Mater Adv. 2021;2(1):413-425.
[30] NAGASAKI T, NAGATA F, SAKURAI M, et al. Effects of pore distribution of hydroxyapatite particles on their protein adsorption behavior. J Asian Ceram Soc. 2017;5(2):88-93.
[31] WANG K, ZHOU C, HONG Y, et al. A review of protein adsorption on bioceramics. Interface Focus. 2012;2(3):259-277.
[32] KLIMEK K, BELCARZ A, PAZIK R, et al. “False” cytotoxicity of ions-adsorbing hydroxyapatite—Corrected method of cytotoxicity evaluation for ceramics of high specific surface area. Mater Sci Eng C. 2016;65:70-79. |