[1] GLUCKMAN E, BROXMEYER HA, AUERBACH AD, et al. Hematopoietic reconstitution in a patient with Fanconi's anemia by means of umbilical-cord blood from an HLA-identical sibling. N Engl J Med. 1989;321(17):1174-1178.
[2] GLUCKMAN E. Hematopoietic stem-cell transplants using umbilical-cord blood. N Engl J Med. 2001;344(24):1860-1861.
[3] 田晓宁.脐血干细胞的特性及其临床应用[J].中国组织工程研究与临床康复,2009,13(36):7197-7200.
[4] BALLEN KK, GLUCKMAN E, BROXMEYER HE. Umbilical cord blood transplantation: the first 25 years and beyond. Blood. 2013;122(4): 491-498.
[5] CAIRO MS, ROCHA V, GLUCKMAN E, et al. Alternative allogeneic donor sources for transplantation for childhood diseases: unrelated cord blood and haploidentical family donors. Biol Blood Marrow Transplant. 2008;14(1 Suppl 1):44-53.
[6] SHEARER WT, LUBIN BH, CAIRO MS, et al. Cord Blood Banking for Potential Future Transplantation. Pediatrics. 2017;140(5): e20172695.
[7] LIU H, RICH ES, GODLEY L, et al. Reduced-intensity conditioning with combined haploidentical and cord blood transplantation results in rapid engraftment, low GVHD, and durable remissions. Blood. 2011;118(24): 6438-6445.
[8] GLUCKMAN E, RUGGERI A, ROCHA V, et al. Family-directed umbilical cord blood banking. Haematologica. 2011;96(11):1700-1707.
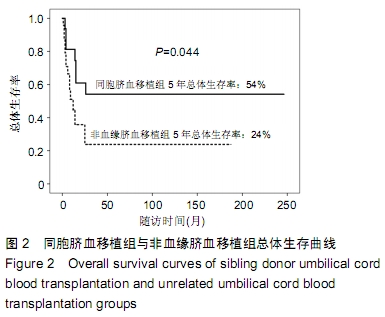
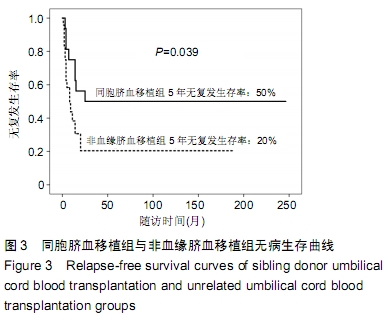
[9] PEFFAULT DE LATOUR R, BRUNSTEIN CG, PORCHER R, et al. Similar overall survival using sibling, unrelated donor, and cord blood grafts after reduced-intensity conditioning for older patients with acute myelogenous leukemia. Biol Blood Marrow Transplant. 2013;19(9): 1355-1360.
[10] LIU HL, SUN ZM, GENG LQ, et al. Similar survival, but better quality of life after myeloablative transplantation using unrelated cord blood vs matched sibling donors in adults with hematologic malignancies. Bone Marrow Transplant. 2014;49(8):1063-1069.
[11] TAKAHASHI S, OOI J, TOMONARI A, et al. Comparative single-institute analysis of cord blood transplantation from unrelated donors with bone marrow or peripheral blood stem-cell transplants from related donors in adult patients with hematologic malignancies after myeloablative conditioning regimen. Blood. 2007;109(3): 1322-1330.
[12] 张之南,沈悌.血液病诊断及疗效标准[M].3版.北京:科学出版社,2007.
[13] EAPEN M, KLEIN JP, SANZ GF, et al. Effect of donor-recipient HLA matching at HLA A, B, C, and DRB1 on outcomes after umbilical-cord blood transplantation for leukaemia and myelodysplastic syndrome: a retrospective analysis. Lancet Oncol. 2011;12(13):1214-1221.
[14] EAPEN M, KLEIN JP, RUGGERI A, et al. Impact of allele-level HLA matching on outcomes after myeloablative single unit umbilical cord blood transplantation for hematologic malignancy. Blood. 2014;123(1): 133-140.
[15] GRAGERT L, EAPEN M, WILLIAMS E, et al. HLA match likelihoods for hematopoietic stem-cell grafts in the U.S. registry. N Engl J Med. 2014; 371(4):339-348.
[16] 张龑丽,宋永平,王桂菊,等.脐血移植治疗恶性血液病的临床研究[J].临床血液学杂志,2004,17:137-140.
[17] GLUCKSBERG H, STORB R, FEFER A, et al. Clinical manifestations of graft-versus-host disease in human recipients of marrow from HL-A-matched sibling donors. Transplantation. 1974;18(4):295-304.
[18] PRZEPIORKA D, WEISDORF D, MARTIN P, et al. 1994 Consensus Conference on Acute GVHD Grading. Bone Marrow Transplant.1995; 15(6):825-828.
[19] SHULMAN HM, SULLIVAN KM, WEIDEN PL, et al. Chronic graft-versus-host syndrome in man. A long-term clinicopathologic study of 20 Seattle patients. Am J Med. 1980;69(2):204-217.
[20] BARKER JN, WAGNER JE. Umbilical-cord blood transplantation for the treatment of cancer. Nat Rev Cancer. 2003;3(7):526-532.
[21] SUN ZM, TANG BL. How I treat adult malignant hematological diseases with single cord blood transplantation. Zhonghua Xue Ye Xue Za Zhi. 2019;40(6):449-452.
[22] 孙自敏,朱江,汤宝林,等.非血缘脐血干细胞移植与同胞造血干细胞移植治疗MDS-EB和AML-MRC的对比观察[J].中华血液学杂志, 2019,40(4): 187-190.
[23] 余正平,丁家华,陈宝安,等. 脐血造血干细胞移植治疗36例血液病患者的临床分析[J]. 中华血液学杂志,2017,38(8):719-721.
[24] HARNICAR S, PONCE DM, HILDEN P, et al. Intensified Mycophenolate Mofetil Dosing and Higher Mycophenolic Acid Trough Levels Reduce Severe Acute Graft-versus-Host Disease after Double-Unit Cord Blood Transplantation. Biol Blood Marrow Transplant. 2015;21(5):920-925.
[25] ROCHA V, LABOPIN M, SANZ G, et al. Transplants of umbilical-cord blood or bone marrow from unrelated donors in adults with acute leukemia. N Engl J Med. 2004;351(22):2276-2285.
[26] WAGNER JE, BARKER JN, DEFOR TE, et al. Transplantation of unrelated donor umbilical cord blood in 102 patients with malignant and nonmalignant diseases: influence of CD34 cell dose and HLA disparity on treatment-related mortality and survival. Blood. 2002; 100(5):1611-1618.
[27] VAN HEECKEREN WJ, FANNING LR, MEYERSON HJ, et al. Influence of human leucocyte antigen disparity and graft lymphocytes on allogeneic engraftment and survival after umbilical cord blood transplant in adults. Br J Haematol. 2007;139(3):464-474.
[28] FRASSONI F, GUALANDI F, PODESTÀ M, et al. Direct intrabone transplant of unrelated cord-blood cells in acute leukaemia: a phase I/II study. Lancet Oncol. 2008;9(9):831-839.
[29] KURTZBERG J, PRASAD VK, CARTER SL, et al. Results of the Cord Blood Transplantation Study (COBLT): clinical outcomes of unrelated donor umbilical cord blood transplantation in pediatric patients with hematologic malignancies. Blood. 2008;112(10):4318-4327.
[30] 万鼎铭,何海燕,边志磊,等.父母供者外周血单倍体干细胞移植治疗儿童复发难治急性白血病[J].中国组织工程研究, 2014,18(32):5237-5243.
[31] 王娴静,董秀娟,陈蕾,等.异基因造血干细胞移植治疗儿童恶性血液病15例临床分析[J].白血病·淋巴瘤,2014,23(12):717-720.
[32] EAPEN M, RUBINSTEIN P, ZHANG MJ, et al. Outcomes of transplantation of unrelated donor umbilical cord blood and bone marrow in children with acute leukaemia: a comparison study. Lancet. 2007;369(9577):1947-1954.
[33] RUGGERI A, PAVIGLIANITI A, GLUCKMAN E, et al. Impact of HLA in cord blood transplantation outcomes. HLA. 2016;87(6):413-421.
[34] GALE RP, EAPEN M. Who is the best alternative allotransplant donor? Bone Marrow Transplant. 2015;50 Suppl 2:S40-42.
[35] WANG J, ZHAN P, OUYANG J, et al. Unrelated donor umbilical cord blood transplantation versus unrelated donor bone marrow transplantation in adult and pediatric patients: A meta-analysis. Leuk Res. 2010;34(8):1018-1022.
[36] 童娟,孙自敏.非血缘脐血移植与非血缘骨髓/外周血干细胞移植治疗恶性血液病临床疗效的研究现状[J]. 国际输血及血液学杂志,2017,40(1):1-7.
[37] 刘会兰,孙自敏.非血缘脐血移植治疗成人恶性血液病[J].国际输血及血液学杂志,2011,34(4):333-336.
[38] BALLEN KK. New trends in umbilical cord blood transplantation. Blood. 2005;105(10):3786-3792.
[39] SACHDEVA A, GUNASEKARAN V, MALHOTRA P, et al. Umbilical Cord Blood Banking: Consensus Statement of the Indian Academy of Pediatrics. Indian Pediatr. 2018;55(6):489-494.
[40] HERR AL, KABBARA N, BONFIM CM, et al. Long-term follow-up and factors influencing outcomes after related HLA-identical cord blood transplantation for patients with malignancies: an analysis on behalf of Eurocord-EBMT. Blood. 2010;116(11):1849-1856.
[41] ROCHA V, WAGNER JE, SOBOCINSKI KA, et al. Graft-versus-host disease in children who have received a cord-blood or bone marrow transplant from an HLA-identical sibling. Eurocord and International Bone Marrow Transplant Registry Working Committee on Alternative Donor and Stem Cell Sources. N Engl J Med. 2000;342(25): 1846-1854.
[42] ROCHA V, CORNISH J, SIEVERS EL, et al. Comparison of outcomes of unrelated bone marrow and umbilical cord blood transplants in children with acute leukemia. Blood. 2001;97(10):2962-2971.
|