[1] BJÖRKEGREN JLM, LUSIS AJ. Atherosclerosis: Recent developments. Cell. 2022;185(10):1630-1645.
[2] LIBBY P. The changing landscape of atherosclerosis. Nature. 2021; 592(7855):524-533.
[3] TSAO CW, ADAY AW, ALMARZOOQ ZI, et al. Heart disease and stroke statistics—2023 update: a report from the American Heart Association. Circul Res. 2023;147(8):e93-e621.
[4] JIA S, LIU Y, YUAN J. Evidence in Guidelines for Treatment of Coronary Artery Disease. Adv Exp Med Biol. 2020;1177:37-73.
[5] MONTRIEF T, KOYFMAN A, LONG B. Coronary artery bypass graft surgery complications: A review for emergency clinicians. Am J Emerg Med. 2018;36(12):2289-2297.
[6] HOOLE SP, BAMBROUGH PJH. Recent advances in percutaneous coronary intervention. Heart. 2020;106(18):1380-1386.
[7] DOENST T, HAVERICH A, SERRUYS P, et al. PCI and CABG for Treating Stable Coronary Artery Disease: JACC Review Topic of the Week. J Am Coll Cardiol. 2019;73(8):964-976.
[8] HONG SJ, HONG MK. Drug-eluting stents for the treatment of coronary artery disease: A review of recent advances. Expert Opin Drug Deliv. 2022;19(3):269-280.
[9] LEE DH, DE LA TORRE HERNANDEZ JM. The Newest Generation of Drug-eluting Stents and Beyond. Eur Cardiol. 2018;13(1):54-59.
[10] TORII S, JINNOUCHI H, SAKAMOTO A, et al. Drug-eluting coronary stents: insights from preclinical and pathology studies. Nat Rev Cardiol. 2020;17(1):37-51.
[11] BAAN J JR, CLAESSEN BE, DIJK KB, et al. A randomized comparison of paclitaxel-eluting balloon versus everolimus-eluting stent for the treatment of any in-stent restenosis: the DARE trial. JACC Cardiovasc Interv. 2018;11(3):275-283.
[12] WANG R, LU J, YIN J, et al. A TEMPOL and rapamycin loaded nanofiber-covered stent favors endothelialization and mitigates neointimal hyperplasia and local inflammation. Bioact Mater. 2023;19(1):666-677.
[13] UDRIȘTE AS, BURDUȘEL AC, NICULESCU AG, et al. Coatings for cardiovascular stents—an up-to-date review. Int J Mol Sci. 2024; 25(2):1078.
[14] DU R, WANG Y, HUANG Y, et al. Design and testing of hydrophobic core/hydrophilic shell nano/micro particles for drug-eluting stent coating. NPG Asia Mater. 2018;10(7):642-658.
[15] LATTUCA B, ODORICO X, OCCEAN B, et al. Long-term efficacy and safety of newer generation ultrathin strut drug-eluting stents: a systematic review and meta-analysis. Eur Heart J. 2020; 41(Supplement_2):ehaa946.2543.
[16] HAUDE M, INCE H, ABIZAID A, et al. Safety and performance of the second-generation drug-eluting absorbable metal scaffold in patients with de-novo coronary artery lesions (BIOSOLVE-II): 6 month results of a prospective, multicentre, non-randomised, first-in-man trial. Lancet. 2016;387(10013):31-39.
[17] MOUSAVIZADEH SM, YU M, GILCHRIST MD, et al. Preparation of a polycaprolactone coating on WE43 for biodegradable stent applications using dual solvents, ultrasonic atomization spray, and anodization. Prog Org Coat. 2024;193(8):108528.
[18] HERMAWAN H, DUBE D, MANTOVANI D. Developments in metallic biodegradable stents. Acta Biomater. 2010;6(5):1693-1697.
[19] HU X, ZHAO W, ZHANG Z, et al. Novel 3D printed shape-memory PLLA-TMC/GA-TMC scaffolds for bone tissue engineering with the improved mechanical properties and degradability. Chin Chem Lett. 2023;34(1):107451.
[20] WEN Y, LI Y, YANG R, et al. Biofunctional coatings and drug-coated stents for restenosis therapy. Mater Today Bio. 2024;29(6):101259.
[21] BARTOSCH M, SCHUBERT S, BERGER FJB. Magnesium stents–fundamentals, biological implications and applications beyond coronary arteries. Bionanomaterials. 2015;16(1):3-17.
[22] TOONG DWY, NG JCK, HUANG Y, et al. Bioresorbable metals in cardiovascular stents: Material insights and progress. Materialia. 2020;12(4):100727.
[23] ALEXY RD, LEVI DS. Materials and manufacturing technologies available for production of a pediatric bioabsorbable stent. Biomed Res Int. 2013;2013(1):137985.
[24] O’BRIEN B, ZAFAR H, IBRAHIM A, et al. Coronary stent materials and coatings: a technology and performance update. Ann Biomed Eng. 2016;44(2):523-535.
[25] KIRILLOVA A, YEAZEL TR, ASHEGHALI D, et al. Fabrication of Biomedical Scaffolds Using Biodegradable Polymers. Chem Rev. 2021; 121(18):11238-11304.
[26] BLASI P. Poly (lactic acid)/poly (lactic-co-glycolic acid)-based microparticles: An overview. J Pharm Investig. 2019;49(4):337-346.
[27] LEE PC, ZAN BS, CHEN LT, et al. Multifunctional PLGA-based nanoparticles as a controlled release drug delivery system for antioxidant and anticoagulant therapy. Int J Nanomed. 2019;14:1533-1549.
[28] BUTT MA. Thin-film coating methods: a successful marriage of high-quality and cost-effectiveness—a brief exploration. Coatings. 2022;12(8):1115.
[29] LI J, HU X, CHEN Y, et al. Review of recent progress in vascular stents: From conventional to functional vascular stents. Chin Chem Lett. 2024;35(1):110492.
[30] WU X, WYMAN I, ZHANG G, et al. Preparation of superamphiphobic polymer-based coatings via spray-and dip-coating strategies. Prog Org Coat. 2016;90(1):463-471.
[31] MUTHIAH P, BHUSHAN B, YUN K, et al. Dual-layered-coated mechanically-durable superomniphobic surfaces with anti-smudge properties. J Colloid Interface Sci. 2013;409(21):227-236.
[32] BOSE S, KELLER SS, ALSTROM TS, et al. Process optimization of ultrasonic spray coating of polymer films. Langmuir. 2013;29(23): 6911-6919.
[33] GOGATE P, KHAIRE R. Use of ultrasonic atomization for encapsulation and other processes in food and pharmaceutical manufacturing. Power ultrasonics, 2023:773-794.
[34] NAIDU H, KAHRAMAN O, FENG H. Novel applications of ultrasonic atomization in the manufacturing of fine chemicals, pharmaceuticals, and medical devices. Ultrason Sonochem. 2022;86(5):105984.
[35] PHAM NP, BOELLAARD E, BURGHARTZ JN, et al. Photoresist coating methods for the integration of novel 3-D RF microstructures.J Microelectromech Syst. 2004;13(3):491-499.
[36] GAL R, DERES L, TOTH K, et al. The Effect of Resveratrol on the Cardiovascular System from Molecular Mechanisms to Clinical Results. Int J Mol Sci. 2021;22(18):10152.
[37] PARSAMANESH N, ASGHARI A, SARDARI S, et al. Resveratrol and endothelial function: A literature review. Pharmacol Res. 2021;170(8): 105725.
[38] LI H, XIA N, HASSELWANDER S, et al. Resveratrol and Vascular Function. Int J Mol Sci. 2019;20(9):2155.
[39] BREUSS JM, ATANASOV AG, UHRIN P. Resveratrol and Its Effects on the Vascular System. Int J Mol Sci. 2019;20(7):1523.
[40] PENG Y, ZHENG X, ZHANG S, et al. Advances in the activity of resveratrol and its derivatives in cardiovascular diseases. Arch Pharm (Weinheim). 2025;358(2):e2400865.
[41] MALAGUARNERA L. Influence of Resveratrol on the Immune Response. Nutrients. 2019;11(5):946.
[42] PAGE MJ, KELL DB, PRETORIUS E.The Role of Lipopolysaccharide-Induced Cell Signalling in Chronic Inflammation. Chronic Stress (Thousand Oaks). 2022;6:24705470221076390.
[43] WEBER M, STEINLE H, GOLOMBEK S, et al. Blood-Contacting Biomaterials: In Vitro Evaluation of the Hemocompatibility. Front Bioeng Biotechnol. 2018;6(16):99.
[44] MICHNO A, GRUZEWSKA K, RONOWSKA A, et al. Resveratrol Inhibits Metabolism and Affects Blood Platelet Function in Type 2 Diabetes. Nutrients. 2022;14(8):1633.
[45] MARUMO M, EKAWA K, WAKABAYASHI I. Resveratrol inhibits Ca(2+) signals and aggregation of platelets. Environ Health Prev Med. 2020; 25(1):70.
[46] NANKIVELL V, PRIMER K, VIDANAPATHIRANA A, et al. Vascular biology of smooth muscle cells and restenosis. Mechanisms of vascular disease: A textbook for vascular specialists, 2020:117-139.
[47] EL-MOKADEM M, EL-RAMLY M, HASSAN A, et al. Comparison between catheter-based delivery of paclitaxel after bare-metal stenting and drug-eluting stents in coronary artery disease patients at high risk for in-stent restenosis. Cardiovasc Revascula. 2017;18(8):596-600.
[48] WANG Y, LEI L, SU Q, et al. Resveratrol Inhibits Insulin‐Induced Vascular Smooth Muscle Cell Proliferation and Migration by Activating SIRT1. Evid Based Complement Alternat Med. 2022;2022(1):8537881.
[49] ASADPOUR S, YEGANEH H, KHADEMI F, et al. Resveratrol-loaded polyurethane nanofibrous scaffold: viability of endothelial and smooth muscle cells. Biomed Mater. 2019;15(1): 015001.
[50] LI Y, FENG L, LI G, et al. Resveratrol prevents ISO-induced myocardial remodeling associated with regulating polarization of macrophages through VEGF-B/AMPK/NF-kB pathway. Int Immunopharmacol. 2020;84(7):106508.
[51] CHICHAREON P, KATAGIRI Y, ASANO T, et al. Mechanical properties and performances of contemporary drug-eluting stent: focus on the metallic backbone. Expert Rev Med Devic. 2019;16(3):211-228.
[52] BARRETT TJ. Macrophages in Atherosclerosis Regression. Arterioscler Thromb Vasc Biol. 2020;40(1):20-33.
[53] BLAGOV AV, MARKIN AM, BOGATYREVA AI, et al. The Role of Macrophages in the Pathogenesis of Atherosclerosis. Cells. 2023; 12(4):522.
[54] HOU P, FANG J, LIU Z, et al. Macrophage polarization and metabolism in atherosclerosis. Cell Death Dis. 2023;14(10):691.
[55] MURRAY PJ. Macrophage Polarization. Annu Rev Physiol. 2017;79(1): 541-566.
[56] YUNNA C, MENGRU H, LEI W, et al. Macrophage M1/M2 polarization. Eur J Pharmacol. 2020;15(877):173090.
[57] JINNOUCHI H, GUO L, SAKAMOTO A, et al. Diversity of macrophage phenotypes and responses in atherosclerosis. Cell Mol Life Sci. 2020; 77(10):1919-1932.
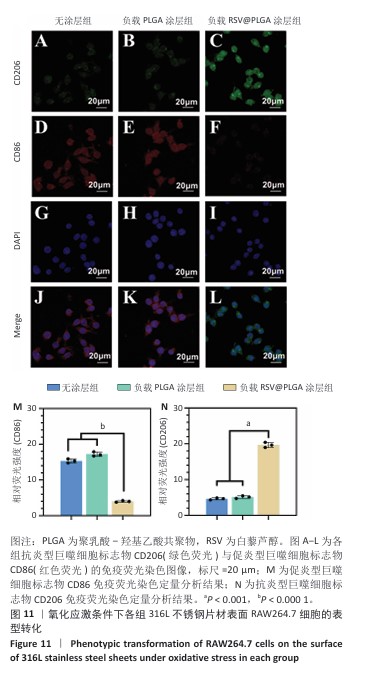
[58] HUANG X, LI Y, FU M, et al. Polarizing Macrophages In Vitro. Methods Mol Biol. 2018;1784:119-126.
[59] KOŹLIK M, HARPULA J, CHUCHRA PJ, et al. Drug-eluting stents: Technical and clinical progress. Biomimetics. 2023;8(1):72.
[60] SCAFA UDRIȘTE A, NICULESCU AG, GRUMEZESCU AM, et al. Cardiovascular stents: a review of past, current, and emerging devices. Materials. 2021;14(10):2498.
[61] CONDELLO F, SPACCAROTELLA C, SORRENTINO S, et al. Stent Thrombosis and Restenosis with Contemporary Drug-Eluting Stents: Predictors and Current Evidence. J Clin Med. 2023;12(3):1238.
[62] HASSAN S, ALI MN, GHAFOOR B. Evolutionary perspective of drug eluting stents: from thick polymer to polymer free approach. J Cardiothorac Surg. 2022;17(1):65.
[63] NOGIC J, MCCORMICK LM, FRANCIS R, et al. Novel bioabsorbable polymer and polymer-free metallic drug-eluting stents. J Cardiol. 2018;71(5):435-443.
[64] WANG C, LV J, YANG M, et al. Recent advances in surface functionalization of cardiovascular stents. Bioact Mater. 2025;44(2): 389-410.
[65] LIU L, LAN X, CHEN X, et al. Multi-functional plant flavonoids regulate pathological microenvironments for vascular stent surface engineering. Acta Biomater. 2023;157(3):655-669.
[66] LIU Y, SHI Y, ZHANG M, et al. Natural polyphenols for drug delivery and tissue engineering construction: A review. Eur J Med Chem. 2024; 266(4):116141.
[67] 张晓琨,张晓晴,伍芳.超声雾化喷涂工艺制备醋酸纤维素多孔膜[J].电子元件与材料,2018,37(10):67-72.
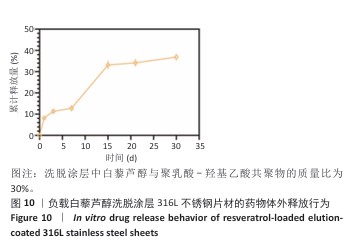
|