[1] GBD 2019 FRACTURE COLLABORATORS. Global, regional, and national burden of bone fractures in 204 countries and territories, 1990-2019: a systematic analysis from the Global Burden of Disease Study 2019. Lancet Healthy Longev. 2021;2(9):e580-e592.
[2] CHUCKRAN CA, LIU C, BRUNO TC, et al. Neuropilin-1: a checkpoint target with unique implications for cancer immunology and immunotherapy. J Immunother Cancer. 2020,8(2):e000967.
[3] SMITH GT, RADIN DP, TSIRKA SE. From protein-protein interactions to immune modulation: Therapeutic prospects of targeting Neuropilin-1 in high-grade glioma. Front Immunol. 2022;13:958620.
[4] REZAEI M, MARTINS CAVACO AC, SEEBACH J, et al. Signals of the Neuropilin-1-MET Axis and Cues of Mechanical Force Exertion Converge to Elicit Inflammatory Activation in Coherent Endothelial Cells. J Immunol. 2019;202(5):1559-1572.
[5] CHIKH A, RAIMONDI C. Endothelial Neuropilin-1: a multifaced signal transducer with an emerging role in inflammation and atherosclerosis beyond angiogenesis. Biochem Soc Trans. 2024;52(1):137-150.
[6] BURCKHARDT CJ, MINNA JD, DANUSER G. SH3BP4 promotes neuropilin-1 and α5-integrin endocytosis and is inhibited by Akt. Dev Cell. 2021;56(8):1164-1181.e12.
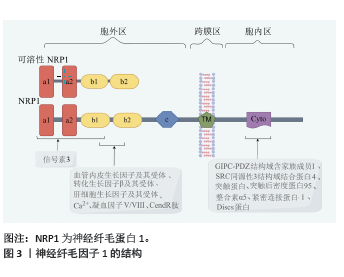
[7] GRUN D, ADHIKARY G, ECKERT RL. NRP-1 interacts with GIPC1 and SYX to activate p38 MAPK signaling and cancer stem cell survival. Mol Carcinog. 2019;58(4):488-499.
[8] BAYLISS AL, SUNDARARAMAN A, GRANET C, et al. Raftlin is recruited by neuropilin-1 to the activated VEGFR2 complex to control proangiogenic signaling. Angiogenesis. 2020;23(3):371-383.
[9] NOAH AA, EL-MEZAYEN NS, EL-GANAINY SO, et al. Reversal of fibrosis and portal hypertension by Empagliflozin treatment of CCl4-induced liver fibrosis: Emphasis on gal-1/NRP-1/TGF-β and gal-1/NRP-1/VEGFR2 pathways. Eur J Pharmacol. 2023;959: 176066.
[10] SARABIPOUR S, KINGHORN K, QUIGLEY KM, et al. Trafficking dynamics of VEGFR1, VEGFR2, and NRP1 in human endothelial cells. PLoS Comput Biol. 2024;20(2):e1011798.
[11] SHIRVALILOO M. The unfavorable clinical outcome of COVID-19 in smokers is mediated by H3K4me3, H3K9me3 and H3K27me3 histone marks. Epigenomics. 2022;14(3):153-162.
[12] YU Y, UCHIDA-FUKUHARA Y, WENG Y, et al. Neuropilin 1 (NRP1) Positively Regulates Adipogenic Differentiation in C3H10T1/2 Cells. Int J Mol Sci. 2023;24(8):7394.
[13] ROMANO E, CHORA I, MANETTI M, et al. Decreased expression of neuropilin-1 as a novel key factor contributing to peripheral microvasculopathy and defective angiogenesis in systemic sclerosis. Ann Rheum Dis. 2016;75(8):1541-1549.
[14] KILARI S, WANG Y, SINGH A, et al. Neuropilin-1 deficiency in vascular smooth muscle cells is associated with hereditary hemorrhagic telangiectasia arteriovenous malformations. JCI Insight. 2022;7(9):e155565.
[15] FANTIN A, LAMPROPOULOU A, GESTRI G, et al. NRP1 Regulates CDC42 Activation to Promote Filopodia Formation in Endothelial Tip Cells. Cell Rep. 2015;11(10):1577-1590.
[16] WANG Y, WANG E, ZHANG Y, et al. Neuropilin-1 maintains dimethylarginine dimethylaminohydrolase 1 expression in endothelial cells, and contributes to protection from angiotensin II-induced hypertension. FASEB J. 2019;33(1): 494-500.
[17] YAMASHITA S, KUDO A, KAWAKAMI H, et al. Mechanisms of angiogenic suppression in uteri exposed to diethylstilbestrol neonatally in the mouse. Biol Reprod. 2013;88(5):116.
[18] SHARMA S, EHRLICH M, ZHANG M, et al. NRP1 interacts with endoglin and VEGFR2 to modulate VEGF signaling and endothelial cell sprouting. Commun Biol. 2024;7(1):112.
[19] COLOTTI G, FAILLA CM, LACAL PM, et al. Neuropilin-1 is required for endothelial cell adhesion to soluble vascular endothelial growth factor receptor 1. FEBS J. 2022;289(1):183-198.
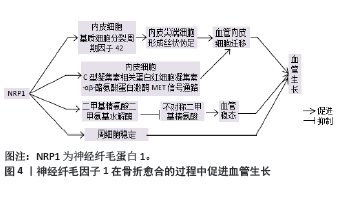
[20] XIE H, CUI Z, WANG L, et al. PDGF-BB secreted by preosteoclasts induces angiogenesis during coupling with osteogenesis. Nat Med. 2014;20(11):1270-1278.
[21] GAO B, DENG R, CHAI Y, et al. Macrophage-lineage TRAP+ cells recruit periosteum-derived cells for periosteal osteogenesis and regeneration. J Clin Invest. 2019;129(6):2578-2594.
[22] MUHL L, FOLESTAD EB, GLADH H, et al. Neuropilin 1 binds PDGF-D and is a co-receptor in PDGF-D-PDGFRβ signaling. J Cell Sci. 2017; 130(8):1365-1378.
[23] DHAR K, DHAR G, MAJUMDER M, et al. Tumor cell-derived PDGF-B potentiates mouse mesenchymal stem cells-pericytes transition and recruitment through an interaction with NRP-1. Mol Cancer. 2010;9:209.
[24] KUSUMBE AP, RAMASAMY SK, ADAMS RH. Coupling of angiogenesis and osteogenesis by a specific vessel subtype in bone. Nature. 2014; 507(7492):323-328.
[25] XU Z, KUSUMBE AP, CAI H, et al. Type H blood vessels in coupling angiogenesis-osteogenesis and its application in bone tissue engineering. J Biomed Mater Res B Appl Biomater. 2023;111(7): 1434-1446.
[26] XU J, HE SJ, XIA TT, et al. Targeting type H vessels in bone-related diseases. J Cell Mol Med. 2024;28(4):e18123.
[27] DANIEL M, SHEPPARD N, CARLOS G, et al. H Vessel Formation as a Marker for Enhanced Bone Healing in Irradiated Distraction Osteogenesis. Semin Plast Surg. 2024;38(1):31-38.
[28] ZHANG D, WANG Y, ZHOU Z, et al. Role of miRNA-regulated type H vessel formation in osteoporosis. Front Endocrinol (Lausanne). 2024; 15:1394785.
[29] QIN X, XI Y, JIANG Q, et al. Type H vessels in osteogenesis, homeostasis, and related disorders. Differentiation. 2023;134:20-30.
[30] LIU X, ZHANG P, GU Y, et al. Type H vessels: functions in bone development and diseases. Front Cell Dev Biol. 2023;11:1236545.
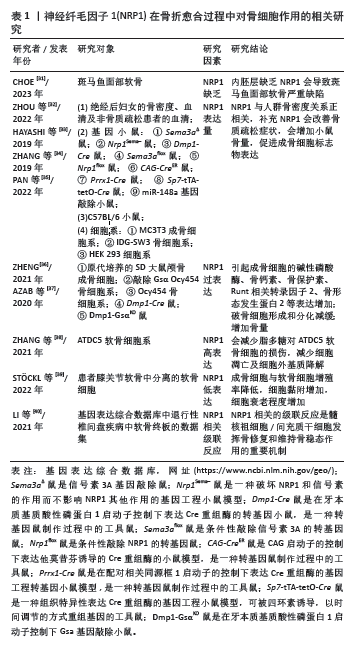
[31] CHOE CP. A Feasible Role of Neuropilin Signaling in Pharyngeal Pouch Formation in Zebrafish. Dev Reprod. 2023;27(3):137-147.
[32] ZHOU HL, WEI MH, DI DS, et al. Association between SEMA3A signaling pathway genes and BMD/OP risk: An epidemiological and experimental study. Front Endocrinol (Lausanne). 2022;13:1014431.
[33] HAYASHI M, NAKASHIMA T, YOSHIMURA N, et al. Autoregulation of Osteocyte Sema3A Orchestrates Estrogen Action and Counteracts Bone Aging. Cell Metab. 2019;29(3):627-637.
[34] ZHANG L, ZHENG L, LI C, et al. Sema3a as a Novel Therapeutic Option for High Glucose-Suppressed Osteogenic Differentiation in Diabetic Osteopath. Front Endocrinol (Lausanne). 2019;10:562.
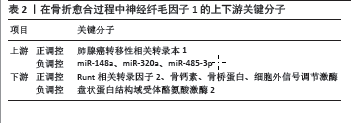
[35] PAN B, ZHENG L, LIU S, et al. MiR-148a deletion protects from bone loss in physiological and estrogen-deficient mice by targeting NRP1. Cell Death Discov. 2022;8(1):470.
[36] ZHENG L. Luteolin Stimulates Proliferation and Inhibits Late Differentiation of Primary Rat Calvarial Osteoblast Induced by High-dose Dexamethasone via Sema3A /NRP1/Pleixin A1. Curr Pharm Biotechnol. 2021;22(11):1538-1545.
[37] AZAB E, CHANDLER KB, UDA Y, et al. Osteocytes control myeloid cell proliferation and differentiation through Gsα-dependent and -independent mechanisms. FASEB J. 2020;34(8):10191-10211.
[38] ZHANG H, LU Y, WU B, et al. Semaphorin 3A mitigates lipopolysaccharide-induced chondrocyte inflammation, apoptosis and extracellular matrix degradation by binding to Neuropilin-1. Bioengineered. 2021;12(2):9641-9654.
[39] STÖCKL S, REICHART J, ZBORILOVA M, et al. Semaphorin 3A-Neuropilin-1 Signaling Modulates MMP13 Expression in Human Osteoarthritic Chondrocytes. Int J Mol Sci. 2022;23(22):14180.
[40] LI W, ZHANG S, ZHAO Y, et al. Revealing the Key MSCs Niches and Pathogenic Genes in Influencing CEP Homeostasis: A Conjoint Analysis of Single-Cell and WGCNA. Front Immunol. 2022;13:933721.
[41] SU C, WANG H, XU L, et al. MALAT1/miR-320a in bone marrow mesenchymal stem cells function may shed light on mechanisms underlying osteoporosis. Arch Med Sci. 2021;18(6):1638-1649.
[42] QIU M, XIE Y, TAN G, et al. Synovial mesenchymal stem cell-derived exosomal miR-485-3p relieves cartilage damage in osteoarthritis by targeting the NRP1-mediated PI3K/Akt pathway: Exosomal miR-485-3p relieves cartilage damage. Heliyon. 2024;10(2):e24042.
[43] ZHANG Y, SU J, TENG Y, et al. Nrp1, a Neuronal Regulator, Enhances DDR2-ERK-Runx2 Cascade in Osteoblast Differentiation via Suppression of DDR2 Degradation. Cell Physiol Biochem. 2015; 36(1):75-84.
[44] HAYASHI M, NAKASHIMA T, TANIGUCHI M, et al. Osteoprotection by semaphorin 3A. Nature. 2012;485(7396):69-74.
[45] CHAPOVAL SP, HRITZO M, QI X, et al. Semaphorin 4A Stabilizes Human Regulatory T Cell Phenotype via Plexin B1. Immunohorizons. 2019;3(2):71-87.
[46] ŁABĘDŹ-MASŁOWSKA A, VERGORI L, KĘDRACKA-KROK S, et al. Mesenchymal stem cell-derived extracellular vesicles exert pro-angiogenic and pro-lymphangiogenic effects in ischemic tissues by transferring various microRNAs and proteins including ITGa5 and NRP1. J Nanobiotechnology. 2024;22(1):60.
[47] KIM JM, LIN C, STAVRE Z, et al. Osteoblast-Osteoclast Communication and Bone Homeostasis. Cells. 2020;9(9):2073.
[48] LI S, SONG C, YANG S, et al. Supercritical CO2 foamed composite scaffolds incorporating bioactive lipids promote vascularized bone regeneration via Hif-1α upregulation and enhanced type H vessel formation. Acta Biomater. 2019;94:253-267.
[49] LI J, CHEN X, REN L, et al. Type H vessel/platelet-derived growth factor receptor β+ perivascular cell disintegration is involved in vascular injury and bone loss in radiation-induced bone damage. Cell Prolif. 2023;56(7):e13406.
[50] LIU W, GUO S, TANG Z, et al. Magnesium promotes bone formation and angiogenesis by enhancing MC3T3-E1 secretion of PDGF-BB. Biochem Biophys Res Commun. 2020;528(4):664-670.
[51] LI N, INOUE K, SUN J, et al. Osteoclasts are not a source of SLIT3. Bone Res. 2020;8:11.
[52] XU R, YALLOWITZ A, QIN A, et al. Targeting skeletal endothelium to ameliorate bone loss. Nat Med. 2018;24(6):823-833.
[53] ZHENG Z, WU L, LI Z, et al. Mir155 regulates osteogenesis and bone mass phenotype via targeting S1pr1 gene. Elife. 2023;12:e77742.
[54] YANG C, LIU Y, WANG Z, et al. Controlled mechanical loading improves bone regeneration by regulating type H vessels in a S1Pr1-dependent manner. FASEB J. 2022;36(10):e22530.
[55] WANG N, LI JY, ZENG B, et al. Sphingosine-1-Phosphate Signaling in Cardiovascular Diseases. Biomolecules. 2023;13(5):818.
[56] TIAN M, HAN YB, YANG GY, et al. The role of lactoferrin in bone remodeling: evaluation of its potential in targeted delivery and treatment of metabolic bone diseases and orthopedic conditions. Front Endocrinol (Lausanne). 2023;14:1218148.
[57] SHI P, FAN F, CHEN H, et al. A bovine lactoferrin-derived peptide induced osteogenesis via regulation of osteoblast proliferation and differentiation. J Dairy Sci. 2020;103(5):3950-3960.
[58] KIM CW, SON KN, CHOI SY, et al. Human lactoferrin upregulates expression of KDR/Flk-1 and stimulates VEGF-A-mediated endothelial cell proliferation and migration. FEBS Lett. 2006;580(18):4332-4336.
[59] 李争争, 赵军伟, 罗伟, 等. 神经毡蛋白-1在创伤性颅脑损伤伴胫骨骨折愈合过程中的表达变化[J].中南大学学报(医学版), 2017,42(2):154-160.
[60] MIAO HQ, SOKER S, FEINER L, et al. Neuropilin-1 mediates collapsin-1/semaphorin III inhibition of endothelial cell motility: functional competition of collapsin-1 and vascular endothelial growth factor-165. J Cell Biol. 1999;146(1):233-242.
[61] GROSSO A, BURGER MG, LUNGER A, et al. It Takes Two to Tango: Coupling of Angiogenesis and Osteogenesis for Bone Regeneration. Front Bioeng Biotechnol. 2017;5:68.
[62] RODRIGUES EM, GIOVANINI AF, RIBAS CAPM, et al. The Nervous System Development Regulator Neuropilin-1 as a Potential Prognostic Marker and Therapeutic Target in Brain Cancer. Cancers (Basel). 2023;15(20):4922.
[63] MENG S, HARA T, SATO H, et al. Revealing neuropilin expression patterns in pancreatic cancer: From single‑cell to therapeutic opportunities (Review). Oncol Lett. 2024;27(3):113.
[64] XING Y, QIU L, LIU D, et al. The role of smart polymeric biomaterials in bone regeneration: a review. Front Bioeng Biotechnol. 2023;11: 1240861.
[65] SUN F, SUN X, WANG H, et al. Application of 3D-Printed, PLGA-Based Scaffolds in Bone Tissue Engineering. Int J Mol Sci. 2022;23(10):5831.
[66] LI X, ZHU L, CHE Z, et al. Progress of research on the surface functionalization of tantalum and porous tantalum in bone tissue engineering. Biomed Mater. 2024;19(4).
[67] PAPYNOV EK, SHICHALIN OO, BELOV AA, et al. CaSiO3-HAp Metal-Reinforced Biocomposite Ceramics for Bone Tissue Engineering. J Funct Biomater. 2023;14(5):259.
|