[1] WANG YL, LI XY, LIU L, et al. Oblique lumbar interbody fusion versus minimally invasive transforaminal lumbar interbody fusion for the treatment of degenerative disease of the lumbar spine: a systematic review and meta-analysis. Neurosurg Rev. 2023;46(1):100.
[2] ALEEM IS, DREW B. Cochrane in CORR@:surgical versus non-surgical treatment for lumbar spinal stenosis. Clin OrthopRelat Res. 2017;475(11):2632-2637.
[3] GBD 2021 LOW BACK PAIN COLLABORATORS. Global, regional, and national burden of low back pain, 1990-2020, its attributable risk factors, and projections to 2050: a systematic analysis of the Global Burden of Disease Study 2021. Lancet Rheumatol. 2023;5(6): e316-e329.
[4] 郭卿,刘会玲,李身泰,等.基于运动疗法的预康复在腰椎间盘突出症手术患者中的应用研究[J].现代中西医结合杂志,2023, 32(20):2902-2905.
[5] 张伟,姜盟盟,孙其志.腰椎术后非感染性发热的相关因素分析[J].中国矫形外科杂志,2020,28(18):1716-1718.
[6] SOUTHWORTH SR, WOODWARD EJ, PENG A, et al. An integrated safety analysis of intravenous ibuprofen (Caldolor(®)) in adults . J Pain Res. 2015;8:753-765.
[7] LEE JJ, KIM JH, JEON JH, et al. A retrospective controlled study of postoperative fever after posterior lumbar interbody fusion due to degenerative lumbar disease. Medicine (Baltimore). 2022;101(20): e29231.
[8] SEO J, PARK JH, SONG EH, et al. Postoperative Nonpathologic Fever After Spinal Surgery: Incidence and Risk Factor Analysis. World Neurosurg. 2017;103:78-83.
[9] 陈升富,李晓琳,王维刚,等.中药解热作用研究进展[J].中国临床药理学与治疗学,2022,27(3):334-344.
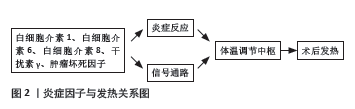
[10] LAI J, WU H, QIN A. Cytokines in Febrile Diseases. J Interferon Cytokine Res. 2021;41(1):1-11.
[11] HOPKINS SJ. Central nervous system recognition of peripheral inflammation: a neural, hormonal collaboration. Acta Biomed. 2007; 78 Suppl 1:231-247.
[12] 耿捷,高书图,赵祚塨.中医药在骨科术后非感染性发热的应用探析[J].中医药导报,2010,16(9):82-83.
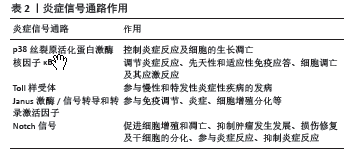
[13] CUADRADO A, NEBREDA AR. Mechanisms and functions of p38 MAPK signalling. Biochem J. 2010;429(3):403-417.
[14] ASHWELL JD. The many paths to p38 mitogen-activated protein kinase activation in the immune system. Nat Rev Immunol. 2006;6(7): 532-540.
[15] GARAMI A, STEINER AA, ROMANOVSKY AA. Fever and hypothermia in systemic inflammation. Handb Clin Neurol. 2018;157:565-597.
[16] NARAYAN M, MEDINILLA SP. Fever in the postoperative patient. Emerg Med Clin North Am. 2013;31(4):1045-1058.
[17] SAAVEDRA F, MYBURG C, LANFRANCONI MB, et al. Fiebre postoperatoria en cirugía ortopédica y urológica [Postoperative fever in orthopedic and urologic surgery]. Medicina (B Aires). 2008;68(1):6-12.
[18] O’DEA E, HOFFMANN A. NF-κB signaling. Wiley Interdiscip Rev Syst Biol Med. 2009;1(1):107-115.
[19] HAYDEN MS, GHOSH S. Shared principles in NF-kappaB signaling. Cell. 2008;132(3):344-362.
[20] SUN SC. The non-canonical NF-κB pathway in immunity and inflammation. Nat Rev Immunol. 2017;17(9):545-558.
[21] POMA P. NF-κB and Disease. Int J Mol Sci. 2020;21(23):9181.
[22] MOORTHY AK, HUANG DB, WANG VY, et al. X-ray structure of a NF-kappaB p50/RelB/DNA complex reveals assembly of multiple dimers on tandem kappaB sites. J Mol Biol. 2007;373(3):723-734.
[23] ABRAHAM E. NF-kappaB activation. Crit Care Med. 2000;28(4 Suppl): N100-N104.
[24] LAWRENCE T. The nuclear factor NF-kappaB pathway in inflammation. Cold Spring Harb Perspect Biol. 2009;1(6):a001651.
[25] DE SILVA NS, SILVA K, ANDERSON MM, et al. Impairment of Mature B Cell Maintenance upon Combined Deletion of the Alternative NF-κB Transcription Factors RELB and NF-κB2 in B Cells. J Immunol. 2016; 196(6):2591-2601.
[26] CRISWELL LA. Gene discovery in rheumatoid arthritis highlights the CD40/NF-kappaB signaling pathway in disease pathogenesis. Immunol Rev. 2010;233(1):55-61.
[27] CHANG SK, ARENDT BK, DARCE JR, et al. A role for BLyS in the activation of innate immune cells. Blood. 2006;108(8): 2687-2694.
[28] YU H, LIN L, ZHANG Z, et al. Targeting NF-κB pathway for the therapy of diseases: mechanism and clinical study. Signal Transduct Target Ther. 2020;5(1):209.
[29] LIANG H, YANG X, LIU C, et al. Effect of NF-κB signaling pathway on the expression of MIF, TNF-α, IL-6 in the regulation of intervertebral disc degeneration. J Musculoskelet Neuronal Interact. 2018;18(4):551-556.
[30] 焦谊,刘志凤,于天源,等.“退热六法”对不同月龄幼兔退热效果及TLR4/NF-κB信号通路的影响[J].长春中医药大学学报,2022, 38(7):746-751.
[31] BLOMQVIST A, ENGBLOM D. Neural Mechanisms of Inflammation-Induced Fever. Neuroscientist. 2018;24(4):381-399.
[32] FITZGERALD KA, KAGAN JC. Toll-like Receptors and the Control of Immunity. Cell. 2020;180(6):1044-1066.
[33] FUKATA M, VAMADEVAN AS, ABREU MT. Toll-like receptors (TLRs) and Nod-like receptors (NLRs) in inflammatory disorders. Semin Immunol. 2009;21(4):242-253.
[34] ROMANOVSKY AA, STEINER AA, MATSUMURA K. Cells that trigger fever. Cell Cycle. 2006;5(19):2195-2197.
[35] STEINER AA, CHAKRAVARTY S, RUDAYA AY, et al. Bacterial lipopolysaccharide fever is initiated via Toll-like receptor 4 on hematopoietic cells. Blood. 2006;107(10):4000-4002.
[36] SANTACROCE L, COLELLA M, CHARITOS IA, et al. Microbial and Host Metabolites at the Backstage of Fever: Current Knowledge about the Co-Ordinate Action of Receptors and Molecules Underlying Pathophysiology and Clinical Implications. Metabolites. 2023;13(3):461.
[37] SARAPULTSEV A, GUSEV E, KOMELKOVA M, et al. JAK-STAT signaling in inflammation and stress-related diseases: implications for therapeutic intervention. Mol Biomed. 2023;4(1):40.
[38] LIU J, WANG F, LUO F. The Role of JAK/STAT Pathway in Fibrotic Diseases: Molecular and Cellular Mechanisms. Biomolecules. 2023;13(1):119.
[39] 赵九洲,姜晓旭,李宏伟,等. JAK-STAT信号通路与巨噬细胞炎症调控的研究进展[J]. 癌变·畸变·突变,2020,32(5):402-404+408.
[40] NESPITAL T, STROUS GJ. The Jak/STAT signaling pathway is downregulated at febrile temperatures. PLoS One. 2012;7(11): e49374.
[41] ZHANG L, SHI W, LIU J, et al. Interleukin 6 (IL-6) Regulates GABAA Receptors in the Dorsomedial Hypothalamus Nucleus (DMH) through Activation of the JAK/STAT Pathway to Affect Heart Rate Variability in Stressed Rats. Int J Mol Sci. 2023;24(16):12985.
[42] ZHOU B, LIN W, LONG Y, et al. Notch signaling pathway: architecture, disease, and therapeutics. Signal Transduct Target Ther. 2022;7(1):95.
[43] GARIS M, GARRETT-SINHA LA. Notch Signaling in B Cell Immune Responses. Front Immunol. 2021;11:609324.
[44] 程静,万磊,赵磊,等.基于Notch1信号通路调控巨噬细胞极化改善佐剂关节炎大鼠关节炎症的机制[J].海南医学院学报,2023, 29(23):1780-1785.
[45] SUAREZ RODRIGUEZ F, SANLIDAG S, SAHLGREN C. Mechanical regulation of the Notch signaling pathway. Curr Opin Cell Biol. 2023; 85:102244.
[46] GALLENSTEIN N, TICHY L, WEIGAND MA, et al. Notch Signaling in Acute Inflammation and Sepsis. Int J Mol Sci. 2023;24(4):3458.
[47] DERADA TROLETTI C, LOPES PINHEIRO MA, CHARABATI M, et al. Notch signaling is impaired during inflammation in a Lunatic Fringe-dependent manner. Brain Behav Immun. 2018;69:48-56.
[48] 王蓉燕齐,韩赵成,樊欢欢,等.从内伤发热论颅脑手术后非感染性发热的中医辨证[J].天津中医药大学学报,2022,41(2):173-176.
[49] 崔玉石.青蒿鳖甲汤联合十全大补方治疗腰椎术后非感染性发热的疗效评价[D].北京:北京中医药大学,2022.
[50] 严佳宝,刘秉新,郭俊彪,等.桃核承气汤对腰椎术后瘀热互结证的疗效[J].广东医学,2023,44(7):838-841.
[51] 张高翔,王德成,苏凤哲,等.清热活血法治疗腰椎间盘突出症术后发热的临床观察[J].河北医药,2020,42(19):2943-2946.
[52] 张智伟,胡仕祥,赵哲.大黄蛰虫汤治疗外科术后非感染性发热(血瘀证)疗效研究[J].中国中医急症,2022,31(1):46-48+66.
[53] 杨鸫祥.身痛逐瘀汤治疗骨伤科术后非感染性发热临床观察[J].中华中医药学刊,2013,31(6):1427-1428.
[54] 麻晓璐,应志强.自拟补气清热汤治疗胸腰椎骨折术后非感染性发热37例[J].浙江中医杂志,2019,54(3):201-202.
[55] 顾天雯,燕文海,王姣姣,等.活血化瘀方结合手法复位治疗A型胸腰段骨折的效果及对骨代谢指标的影响[J].湖北中医药大学学报,2023,25(5):74-76.
[56] 曾意荣,樊粤光,刘红,等.补肾活血中药对大鼠骨髓间充质干细胞体外增殖的影响[J]. 中药新药与临床药理,2007,18(2):93-96.
[57] 杨宇,黄兴琳,江忠敏,等.中药红花化学成分与药理作用研究新进展[J].中华中医药学刊,2023,41(10):119-126.
[58] 邓静,颜丹娜,吴孟华,等.桃仁药性与应用的古今比较[J].中药材,2023,46(4):1034-1042.
[59] 杨晓寰,张敏,纪璇,等.上呼吸道感染患者抗生素治疗前后中医证型变化关系[J].天津中医药大学学报,2012,31(1):17-19.
[60] 孔畅,林定坤,李永津,等.三仁汤治疗脊柱病术后湿阻发热的临床研究[J].时珍国医国药,2006(6):1045-1046.
[61] VERMA A, AGGARWAL K, AGRAWAL R, et al. Molecular mechanisms regulating the pharmacological actions of icariin with special focus on PI3K-AKT and Nrf-2 signaling pathways. Mol Biol Rep. 2022;49(9): 9023-9032.
[62] LUO Z, DONG J, WU J. Impact of Icariin and its derivatives on inflammatory diseases and relevant signaling pathways. Int Immunopharmacol. 2022;108:108861.
[63] PATEL SS, ACHARYA A, RAY RS, et al. Cellular and molecular mechanisms of curcumin in prevention and treatment of disease. Crit Rev Food Sci Nutr. 2020;60(6):887-939.
[64] REIS L, OLIVEIRA MK, ROJAS VCT, et al. Curcumin attenuates
LPS-induced sickness behavior and fever in rats by modulating Nrf2
activity. Neurosci Lett. 2022;781:136680.
[65] KIM JH, PARK GY, BANG SY, et al. Crocin suppresses LPS-stimulated expression of inducible nitric oxide synthase by upregulation of heme oxygenase-1 via calcium/calmodulin-dependent protein kinase 4. Mediators Inflamm. 2014;2014:728709.
[66] LEE YJ, KIM JH, KIM Y. Dendrobium moniliforme Stem Extract Inhibits Lipoteichoic Acid-Induced Inflammatory Responses by Upregulation of Heme Oxygenase-1. J Microbiol Biotechnol. 2018;28(8): 1310-1317.
[67] 程芳,胡坤敏,朱珊. 活血化瘀类中药抗炎机制研究进展[J]. 中国医药导报,2023,20(8):46-49+65.
[68] 马宁宁,范姗姗,李欣,等. 川芎的抗炎物质筛选及其作用机制分析[J]. 中国实验方剂学杂志,2018,24(18):140-146.
[69] 戴娜,王从安,师彬.丹参活性成分防治骨关节炎作用机制的研究进展[J].环球中医药,2023,16(10):2147-2152.
[70] 赵子樟,李佳晌,宿树兰,等. 基于网络药理学及细胞实验的乳香-没药功效成分抗炎机制研究[J]. 中国中药杂志,2021,46(21): 5674-5682.
[71] 赵丽辉,赵子樟,李佳晌,等.乳香、没药活性成分KTDA、FSA及其配伍的抗炎镇痛作用及机制研究[J].中药新药与临床药理, 2022,33(11):1460-1465.
[72] 杨宝,徐莲莲,陈芳有,等.没药化学成分及抗炎活性研究[J].中草药,2023,54(9):2716-2721.
[73] 李艳,苗明三.益母草药理作用研究进展[J].中华中医药学刊,2023, 41(5):102-106.
[74] 杨正汉,赵继荣,王兴盛,等.牛膝及其有效成分防治腰椎间盘突出症的研究进展[J].中华中医药学刊,2023,41(1):143-147.
[75] 王惠,冯玛莉,张越,等.藏柴胡与北柴胡急性毒性、解热、抗炎作用的对比研究[J].世界科学技术-中医药现代化,2020,22(5): 1517-1523.
[76] 胡建燃,李平,赵红梅,等.柴胡总黄酮的体外抗炎及抗氧化活性研究[J].中国食品添加剂,2023,34(9):82-88.
[77] 郑立,汤韵秋,余琳媛,等. 连翘挥发油自微乳的制备及解热作用[J]. 中华中医药学刊,2020,38(3):149-153.
[78] 席亚莉,白雅雯,麻春杰,等. 连翘的免疫调节活性成分及作用机制研究进展[J]. 中华中医药学刊,2023,41(12):194-197.
[79] 徐雯,吴艳清,丁浩然,等. 广藿香的药理作用及机制研究进展[J]. 上海中医药杂志,2017,51(10):103-106.
[80] 楚继敏,孙素姣. 野菊花活性成分的抗炎机制研究进展[J]. 中医药临床杂志,2021,33(10):2023-2026.
[81] 崔园园,刘佳昕,邢博宇,等.甘草抗炎活性物质基础及其作用机制研究进展[J].中华中医药学刊,2024,42(6):99-103+276.
[82] 韩维维,钟晴,张蓉,等. 甘草有效成分及其作用机制研究进展[J]. 生命的化学,2023,43(12):1956-1962.
[83] SHANG X, PAN H, LI M, et al. Lonicera japonica Thunb.: ethnopharmacology, phytochemistry and pharmacology of an important traditional Chinese medicine. J Ethnopharmacol. 2011; 138(1):1-21.
[84] 曾安琪,华桦,陈朝荣,等. 金银花、山银花抗炎药理作用研究[J]. 中国中药杂志,2020,45(16):3938-3944.
[85] 关秀锋,王锐,李晓龙,等. 金银花的化学成分与药理作用研究新进展[J]. 化学工程师,2020,34(4):59-62.
[86] LIU C, CHU D, KALANTAR-ZADEH K, et al. Cytokines: From Clinical Significance to Quantification. Adv Sci (Weinh). 2021;8(15): e2004433.
[87] 陈升富,李晓琳,王维刚,等. 中药解热作用研究进展[J]. 中国临床药理学与治疗学,2022,27(3):334-344.
[88] BLOMQVIST A. Prostaglandin E2 Production by Brain Endothelial Cells and the Generation of Fever. DNA Cell Biol. 2023;42(3):107-112.
[89] XUE R, MIAO YF, YANG JC, et al. [Prostaglandin(PG) E2 in regulation of immunity and inflammatory diseases]. Sheng Li Ke Xue Jin Zhan. 2011;42(3):165-168.
[90] YE K, LI Y, XING Y, et al. A Randomized Study on the Prophylactic Use of Acetaminophen to Prevent Fever after the Removal of Drainage Tubes for Lumbar Surgery. Orthop Surg. 2023;15(2):440-447.
[91] LI Z, SHEN J, LI Q, et al. Drug Fever Induced by Piperacillin/Tazobactam in a Scoliosis Patient: A Case Report. Medicine (Baltimore). 2015; 94(46):e1875.
[92] XU D, HU X, ZHANG H, et al. Analysis of risk factors for deep vein thrombosis after spinal infection surgery and construction of a nomogram preoperative prediction model. Front Cell Infect Microbiol. 2023;13:1220456.
[93] BERISTAIN-COVARRUBIAS N, PEREZ-TOLEDO M, THOMAS MR, et al. Understanding Infection-Induced Thrombosis: Lessons Learned From Animal Models. Front Immunol. 2019;10:2569.
[94] PIERANNUNZII L, FOSSALI A, DE LUCIA O, et al. Suture-related pseudoinfection after total hip arthroplasty. J Orthop Traumatol. 2015;16(1):59-65.
[95] DRAGOVIC M, PEJOVIC M, STEPIC J, et al. Comparison of four different suture materials in respect to oral wound healing, microbial colonization, tissue reaction and clinical features-randomized clinical study. Clin Oral Investig. 2020;24(4):1527-1541.
[96] LOCK AM, GAO R, NAOT D, et al. Induction of immune gene expression and inflammatory mediator release by commonly used surgical suture materials: an experimental in vitro study. Patient Saf Surg. 2017;11:16.
[97] WANG H, REN D, SUN H, et al. Research progress on febrile non-hemolytic transfusion reaction: a narrative review. Ann Transl Med. 2022;10(24):1401.
[98] SEO J, PARK JH, SONG EH, et al. Postoperative Nonpathologic Fever After Spinal Surgery: Incidence and Risk Factor Analysis. World Neurosurg. 2017;103:78-83.
[99] ABDALLAH DY, JADAAN MM, MCCABE JP. Body mass index and risk of surgical site infection following spine surgery: a meta-analysis. Eur Spine J. 2013;22(12):2800-2809.
[100] LUO M, CAO Q, WANG D, et al. The impact of diabetes on postoperative outcomes following spine surgery: A meta-analysis of 40 cohort studies with 2.9 million participants. Int J Surg. 2022;104:106789. |