| [1] Zencica P, Chaloupka R, Hladíková J,et al. Adjacent segment degeneration after lumbosacral fusion in spondylolisthesis: a retrospective radiological and clinical analysis. Acta Chir Orthop Traumatol Cech. 2010;77(2):124-130.
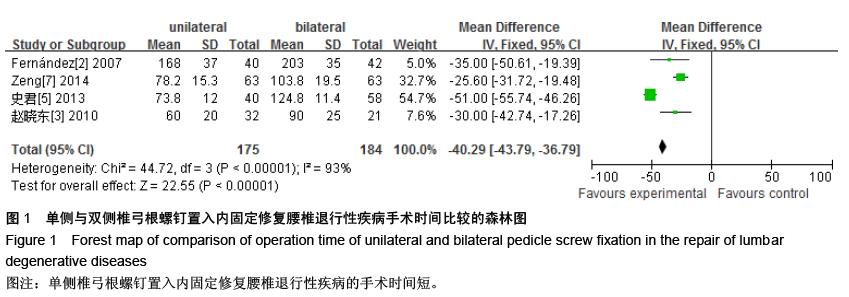
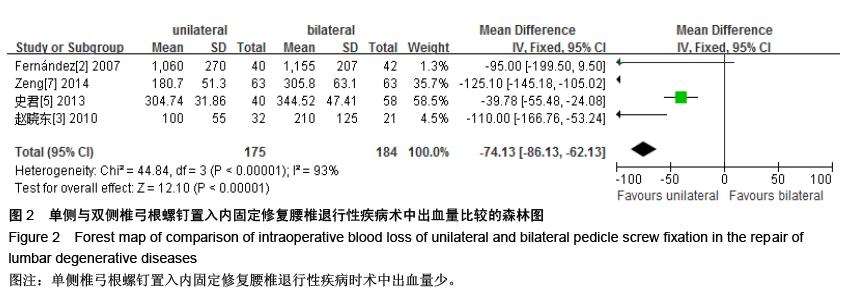
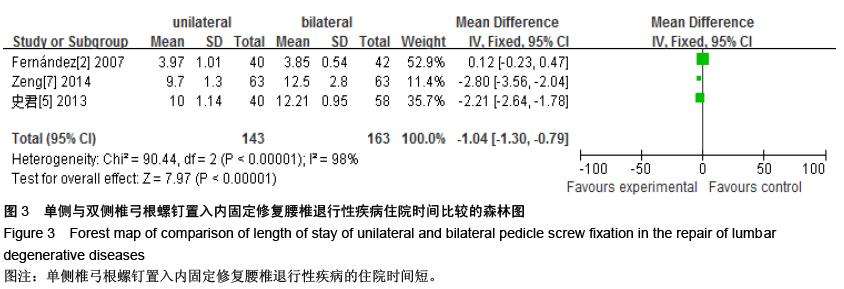
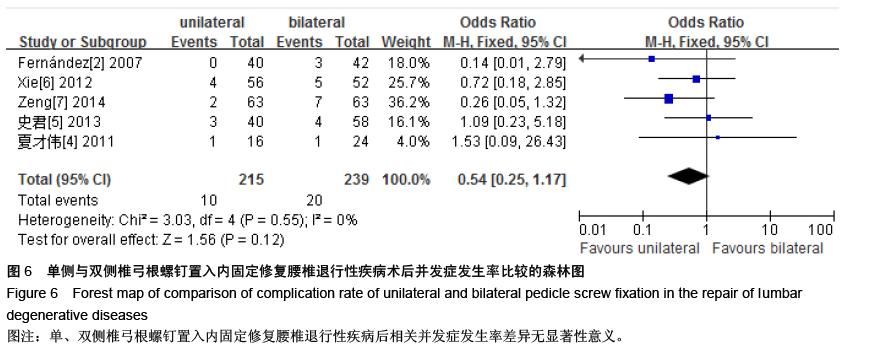
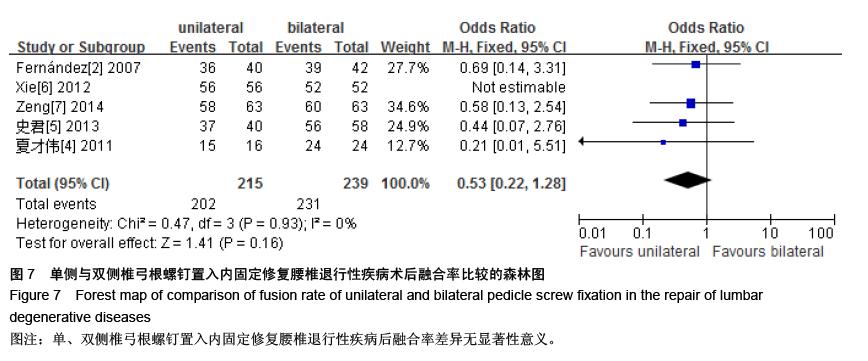
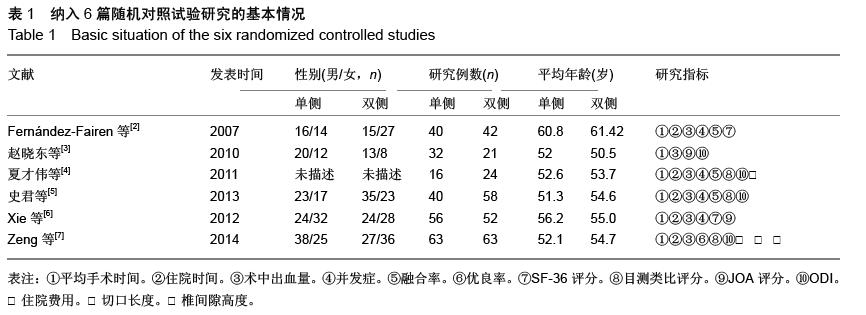
[2] Fernández-Fairen M, Sala P, Ramírez H,et al. A prospective randomized study of unilateral versus bilateral instrumented posterolateral lumbar fusion in degenerative spondylolisthesis. Spine (Phila Pa 1976). 2007;32(4):395-401.
[3] 赵晓东,付美奇,袁智锐,等.单侧椎弓根螺钉固定治疗腰椎间盘突出伴腰椎不稳症[J].实用骨科杂志,2010,16(8): 608-611.
[4] 夏才伟,王生介,厉晓龙,等.单双侧椎弓根钉内固定结合椎间融合术治疗腰椎椎间盘突出症初期疗效比较[J].脊柱外科杂志, 2011,9(2):65-68.
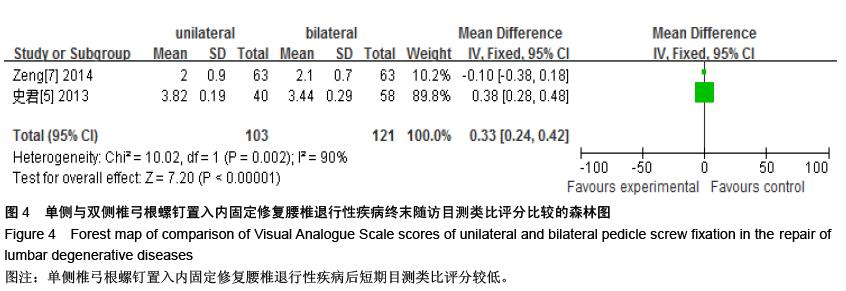
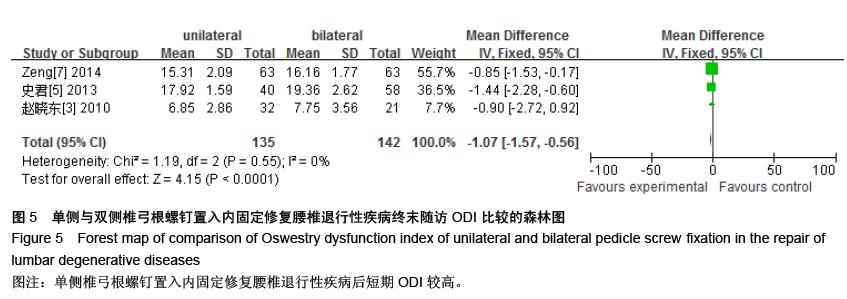
[5] 史君,胡力,周忠,等.单双侧椎弓根钉内固定结合椎间融合术治疗腰椎退行性疾病的疗效比较[J].中国矫形外科杂志,2013,21(7): 651-657.
[6] Xie Y, Ma H, Li H, et al. Comparative study of unilateral and bilateral pedicle screw fixation in posterior lumbar interbody fusion. Orthopedics. 2012;35(10):e1517-1523.
[7] Zeng J, Yao H, Dai M,et al. Clinical application of unilateral pedicle screw for lumbar intervertebral disc protrusion. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2014;28(1):74-78.
[8] Sasso RC, Best NM, Mummaneni PV,et al. Analysis of operative complications in a series of 471 anterior lumbar interbody fusion procedures. Spine (Phila Pa 1976). 2005;30(6):670-674.
[9] Slucky AV, Brodke DS, Bachus KN,et al. Less invasive posterior fixation method following transforaminal lumbar interbody fusion:a biomechanicalmanalysis. Spine J.2006;6(1):78-85.
[10] Shah RR, Mohammed S, Saifuddin A,et al. Radiologic evaluation of adjacent superior segment facet joint violation following transpedicular instrumentation of the lumbar spine. Spine (Phila Pa 1976). 2003;28(3): 272-275.
[11] McAfee PC, Farey ID, Sutterlin CE,et al. The effect of spinal implant rigidity on vertebral bone density. A canine model. Spine (Phila Pa 1976). 1991;16 (6 Suppl): S190-197.
[12] Iwatsuki K, Yoshimine T, Aoki M.Bilateral interlaminar fenestration and unroofing for the decompression of nerve roots by using a unilateral approach in lumbar canal stenosis. Surg Neurol. 2007;68(5):487-492.
[13] Kotil K, Ali Akçetin M, Sava? Y. Clinical and radiologic outcomes of TLIF applications with or without pedicle screw: a double center prospective pilot comparative study. J Spinal Disord Tech. 2013; 26(7):359-366.
[14] 陈志明.腰椎单侧椎弓根螺钉固定的生物力学研究及临床应用[D].上海:第二军医大学,2009.
[15] 薛剑,靳安民,孙小平,等.单侧腰椎弓根螺钉及经椎板关节突螺钉固定与双侧固定的比较[J].中国组织工程研究, 2013,17(9): 1571-1578.
[16] 周纲,杨晓辉,黄卫民,等.双侧及单侧椎弓根螺钉置入与椎间植骨融合修复老年退行性腰椎滑脱[J].中国组织工程研究, 2015,19(31):4973-4977.
[17] Doulgeris JJ, Aghayev K, Gonzalez-Blohm SA,et al. Biomechanical comparison of an interspinous fusion device and bilateral pedicle screw system as additional fixation for lateral lumbar interbody fusion. Clin Biomech (Bristol, Avon). 2015;30(2):205-210.
[18] Villavicencio AT, Serxner BJ, Mason A,et al.Unilateral and bilateral pedicle screw fixation in transforaminal lumbar interbody fusion: radiographic and clinical analysis.World Neurosurg. 2015;83(4):553-559.
[19] Xiao SW,Jiang H,Yang LJ,et al.Comparison of unilateral versus bilateral pedicle screw fixation with cage fusion in degenerative lumbar diseases: a meta-analysis.Eur Spine J.2015;24(4):764-774.
[20] Yang X,Wang H,Zhao Q,et al. A comparison of unilateral and bilateral pedicle screw fixation combined with transforaminal lumbar interbody fusion for lumbar degenerative diseases.Chin Med J (Engl). 2014;127 (20):3592-3596.
[21] 厉晓龙,刘锦波.单侧椎弓根螺钉内固定椎间融合术治疗腰椎间盘突出症的研究进展[J].中国矫形外科杂志, 2011,19(19): 1623-1625.
[22] 楚戈,卡哈尔•艾肯木,何祖胜.单、双侧后外侧椎弓根钉置入并植骨融合治疗退变性腰椎滑脱的随机对照[J].中国组织工程研究与临床康复,2011,15(35):6540-6545. |
.jpg)
.jpg)