[1] GOPINATH V. Osteoporosis. Med Clin North Am. 2023;107(2):213-225.
[2] ALI D, TENCEROVA M, FIGEAC F, et al. The pathophysiology of osteoporosis in obesity and type 2 diabetes in aging women and men: The mechanisms and roles of increased bone marrow adiposity. Front Endocrinol (Lausanne). 2022;13:981487.
[3] BARRON RL, OSTER G, GRAUER A, et al. Determinants of imminent fracture risk in postmenopausal women with osteoporosis. Osteoporos Int. 2020;31(11):2103-2111.
[4] CHEN P, LI Z, HU Y. Prevalence of osteoporosis in China: a meta-analysis and systematic review. BMC Public Health. 2016;16(1):1039.
[5] TRAJANOSKA K, RIVADENEIRA F.The genetic architecture of osteoporosis and fracture risk. Bone. 2019;126:2-10.
[6] DENG T, ZHANG W, ZHANG Y, et al. Thyroid-stimulating hormone decreases the risk of osteoporosis by regulating osteoblast proliferation and differentiation. BMC Endocr Disord. 2021;21(1):49.
[7] WANG S, DENG Z, MA Y, et al. The Role of Autophagy and Mitophagy in Bone Metabolic Disorders. Int J Biol Sci.2020;16(14):2675-2691.
[8] HU K, SHANG Z, YANG X, et al. Macrophage Polarization and the Regulation of Bone Immunity in Bone Homeostasis. J Inflamm Res. 2023;16:3563-3580.
[9] CHEN X, WANG Z, DUAN N, et al.Osteoblast-osteoclast interactions.Connect Tissue Res. 2018;59(2):99-107.
[10] 黎征鹏, 章晓云, 曾浩, 等. 基于“脏腑-骨痿”理论探讨绝经后骨质疏松症的发病机制[J].世界中医药,2024,19(19):1-8.
[11] 胡得翼, 鄢卫平, 李景周, 等.基于“肾虚血瘀”理论探讨骨质疏松症的病因病机及治疗现状[J]. 风湿病与关节炎,2023;12(11):44-47.
[12] SONG S, GUO Y, YANG Y, et al. Advances in pathogenesis and therapeutic strategies for osteoporosis. Pharmacol Ther. 2022;237:108168.
[13] NUNKOO S, KRISSHEEVEN M, CHITRAVANSHI A, et al. Clinical Efficacy and Safety of Teriparatide Versus Alendronate in Postmenopausal Osteoporosis: A Systematic Review of Randomized Controlled Trials. Cureus. 2024;16(11):e73068.
[14] IBRAHIM N, FOO LK, CHUA SL. Predicting the Severity of Adverse Events on Osteoporosis Drugs Using Attribute Weighted Logistic Regression. Int J Environ Res Public Health. 2023;20(4):3289.
[15] ROSSINI M, ADAMI G, ADAMI S, et al. Safety issues and adverse reactions with osteoporosis management. Expert Opin Drug Saf. 2016;15(3):321-332.
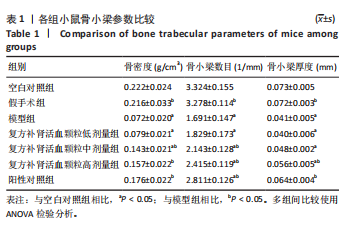
[16] 赵进东, 舒仪琼, 刘剑, 等. 复方补肾活血颗粒对肾虚血瘀证绝经后非老年骨质疏松症患者视觉模拟评分和骨密度影响的临床观察[J]. 中国骨质疏松杂志,2018,24(1):98-101.
[17] 王雨. 基于“肾虚血瘀”理论探究复方补肾活血颗粒治疗老年性骨质疏松症患者的临床研究[D]. 合肥:安徽中医药大学,2022.
[18] 朱余俊, 吕浩, 江渟. 复方补肾活血颗粒对人骨髓间充质干细胞增殖及Wnt/PI3K-AKT信号通路相关蛋白表达的影响[J].中国中医药信息杂志,2022,29(3):79-84.
[19] 乔明珠, 吕浩, 胡芷苜,等. 基于Wnt/β-catenin信号通路的复方补肾活血颗粒对骨髓间充质干细胞成骨、成脂分化的影响[J]. 中国中医药信息杂志,2023,30(11):107-113.
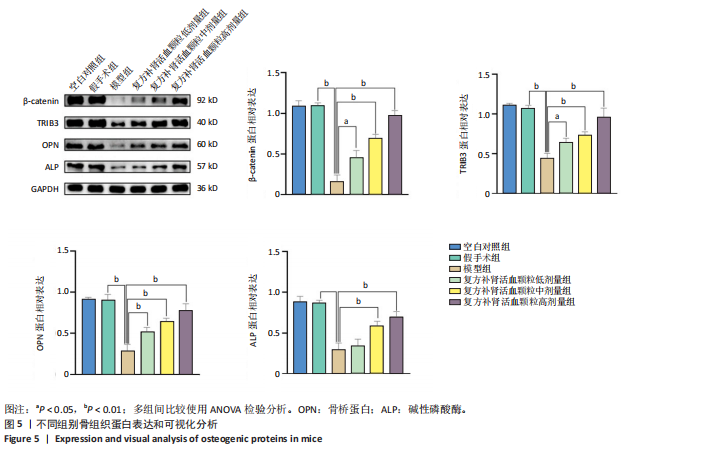
[20] 胡芷苜, 王久香, 江渟. 复方补肾活血颗粒含药血清经β-catenin/TRIB3调控人骨髓间充质干细胞成骨成脂分化[J]. 安徽中医药大学学报,2024,43(5):78-85.
[21] 乌云必力格, 青格勒, 斯琴, 等. 基于Wnt/β-cat信号通路探讨蒙药润骨灵治疗绝经后骨质疏松症小鼠的疗效及作用机制[J]. 中国民族医药杂志,2024,30(9):45-50.
[22] 韩丽侠, 杨晨晨, 高志泽, 等. NLRP3对小鼠骨质疏松及PI3K/Akt/mTOR信号通路的影响[J]. 中国老年学杂志,2024,44(17):4317-4322.
[23] 浦冬青, 冯丹丹, 张梦棣, 等. 黄芪补肾活血汤对芳香化酶抑制剂诱导骨质疏松模型小鼠破骨细胞活性的影响[J]. 中国组织工程研究,2025,29(14):2861-2867.
[24] HUANG F, WANG Y, LIU J, et al. Asperuloside alleviates osteoporosis by promoting autophagy and regulating Nrf2 activation. J Orthop Surg Res. 2024;19(1):855.
[25] 牛园园, 张天驰, 李沐哲, 等. 温肾通络止痛方通过AMPK/mTOR信号通路调控自噬对老年性骨质疏松模型小鼠的干预作用[J].中国中西医结合杂志,2024,44(1):84-90.
[26] 韦雨柔,田佳庆,肖方骏,等.活血通络胶囊对激素性股骨头坏死大鼠肠道菌群影响的研究[J].中国全科医学,2023,26(29):3674-3682.
[27] HSU SH, CHEN LR, CHEN KH. Primary Osteoporosis Induced by Androgen and Estrogen Deficiency: The Molecular and Cellular Perspective on Pathophysiological Mechanisms and Treatments. Int J Mol Sci. 2024;25(22):12139.
[28] LI X, LI N, PEI H, et al. Zhuanggu Shubi ointment mediated the characteristic bacteria-intestinal mucosal barrier-bone metabolism axis to intervene in postmenopausal osteoporosis. Front Cell Infect Microbiol. 2024;14:1500111.
[29] HU X, LEI X, LIN W, et al. Quercetin promotes osteogenic differentiation of bone marrow mesenchymal stem cells by modulating the miR-214-3p/Wnt3a/beta-catenin signaling pathway. Exp Cell Res. 2024; 444(2):114386.
[30] WANG S, LI Y, ZHANG N, et al. Screening of ESR2-targeted anti-postmenopausal osteoporosis chemistry from Rehmanniae Radix Preparata based on affinity ultrafiltration with UPLC-QE-Orbitrap-MS. J Chromatogr B Analyt Technol Biomed Life Sci. 2024;1251:124419.
[31] CHEN J, NG S, XU P, et al. Herbal formula xuling-jiangu improves bone metabolic balance in rats with ovariectomy-induced osteoporosis via the gut-bone axis. Front Pharmacol. 2024;15:1505231.
[32] ZHANG Y, HAN B, WEI Y, et al. Icariin Promotes Fracture Healing in Ovariectomized Rats. Med Sci Monit. 2020;26:e924554.
[33] 卜寒梅, 王世坤, 李远栋, 等. 补肾中药基于OPG/RANKL/RANK信号通路对原发性骨质疏松症作用机制的研究进展[J]. 中草药, 2022,53(10):3209-3217.
[34] HAN SY, LEE JR, KWON YK, et al. Ostreae Testa prevent ovariectomy-induced bone loss in mice by osteoblast activations. J Ethnopharmacol. 2007;114(3):400-405.
[35] FENG X, JIANG S, ZHANG F, et al. Shell water-soluble matrix protein from oyster shells promoted proliferation, differentiation and mineralization of osteoblasts in vitro and vivo. Int J Biol Macromol. 2022;201:288-297.
[36] WANG J, HUANG Y, GUO L, et al. Molecular mechanism of Achyranthis bidentatae radix and Morindae officinalis radix in osteoporosis therapy:An investigation based on network pharmacology, molecular docking, and molecular dynamics simulations. Biochem Biophys Rep. 2023;36:101586.
[37] LIU J, LIU J, LIU L,et al.Reprogrammed intestinal functions in Astragalus polysaccharide-alleviated osteoporosis: combined analysis of transcriptomics and DNA methylomics demonstrates the significance of the gut-bone axis in treating osteoporosis. Food Funct. 2021;12(10):4458-4470.
[38] GUO W, YANG XG, SHI YL, et al.The effects and mechanism of paeoniflorin in promoting osteogenic differentiation of MC3T3-E1. J Orthop Surg Res. 2022;17(1):90.
[39] LUO JS, ZHAO X, YANG Y. Effects of emodin on inflammatory bowel disease-related osteoporosis. Biosci Rep. 2020;40(1):BSR20192317.
[40] LV H, WANG J, ZHU Y, et al. Study on the Mechanism of Compound Kidney-Invigorating Granule for Osteoporosis based on Network Pharmacology and Experimental Verification. Evid Based Complement Alternat Med. 2022;2022:6453501.
[41] WANG X, QU Z, ZHAO S, et al. Wnt/beta-catenin signaling pathway: proteins’ roles in osteoporosis and cancer diseases and the regulatory effects of natural compounds on osteoporosis. Mol Med. 2024;30(1):193.
[42] DU K, HERZIG S, KULKARNI RN, et al. TRB3: a tribbles homolog that inhibits Akt/PKB activation by insulin in liver. Science. 2003;300(5625):1574-1577.
[43] ARIF A, ALAMERI AA, TARIQ UB, et al. The functions and molecular mechanisms of Tribbles homolog 3 (TRIB3) implicated in the pathophysiology of cancer. Int Immunopharmacol. 2023;114:109581.
[44] BAI XS, LV LW, ZHOU YS.Tribbles pseudokinase 3 inhibits the adipogenic differentiation of human adipose-derived mesenchymal stem cells. Beijing Da Xue Xue Bao Yi Xue Ban.2020;52(1):1-9.
[45] FAN J, LEE CS, KIM S, et al. Trb3 controls mesenchymal stem cell lineage fate and enhances bone regeneration by scaffold-mediated local gene delivery. Biomaterials. 2021;264:120445.
[46] 王子文, 王久香, 吕浩, 等. 复方补肾活血颗粒含药血清通过Trb3调控hBMSCs成骨成脂分化[J]. 中国骨质疏松杂志,2023,29(4): 544-549+561.
[47] ZHU Z, HU X, LIU K, et al. E3 ubiquitin ligase Siah1 aggravates NAFLD through Scp2 ubiquitination. Int Immunopharmacol. 2023;124(Pt A): 110897.
[48] KNAUER SK, MAHENDRARAJAH N, ROOS WP, et al. The inducible E3 ubiquitin ligases SIAH1 and SIAH2 perform critical roles in breast and prostate cancers. Cytokine Growth Factor Rev. 2015;26(4):405-413.
[49] YUAN H, WU H, CHENG J, et al. SIAH1 ubiquitination-modified HMGCR inhibits lung cancer progression and promotes drug sensitivity through cholesterol synthesis. Cancer Cell Int. 2023;23(1):71.
[50] ZHOU Y, LI L, LIU Q, et al. E3 ubiquitin ligase SIAH1 mediates ubiquitination and degradation of TRB3. Cell Signal. 2008;20(5):942-948.
[51] TAN L, YAMMANI RR. Co-Immunoprecipitation-Blotting: Analysis of Protein-Protein Interactions. Methods Mol Biol. 2022;2413:145-154.
|