[1] 何伟. 股骨头坏死的诊断与保髋治疗[J]. 中医正骨,2024,36(9):12-14+18.
[2] MOTTA F, TIMILSINA S, GERSHWIN ME, et al. Steroid-induced osteonecrosis. J Transl Autoimmun. 2022;5:100168.
[3] LI L, ZHAO S, LENG Z, et al. Pathological mechanisms and related markers of steroid-induced osteonecrosis of the femoral head. Ann Med. 2024;56(1):2416070.
[4] CHANG C, GREENSPAN A, GERSHWIN ME. The pathogenesis, diagnosis and clinical manifestations of steroid-induced osteonecrosis. J Autoimmun. 2020;110:102460.
[5] ZHANG Y, TANG J, YUE Z, et al. Tension-Free Weight-Bearing Model of Steroid-Induced Osteonecrosis of Femoral Head in Rats. J Vis Exp. 2024;(211). doi: 10.3791/66883.
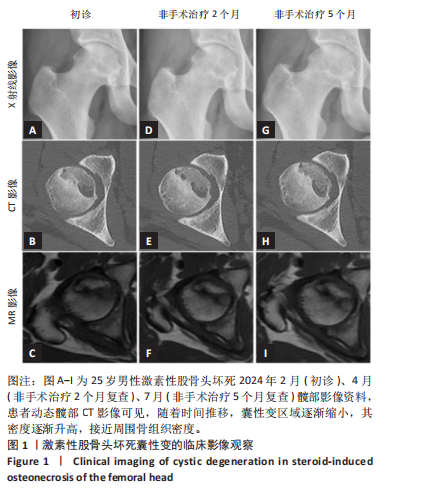
[6] 魏秋实, 何敏聪, 何晓铭, 等. 靶向囊性变探索激素性股骨头坏死塌陷与修复的动态时空关系[J]. 辽宁中医杂志,2025,52(5):1-4+221.
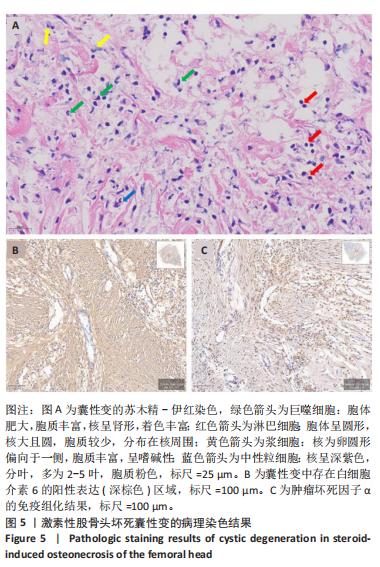
[7] 田佳庆,何敏聪,韦雨柔,等.激素性股骨头坏死囊性变分布规律及病理特点[J].中国组织工程研究,2023,27(31):4996-5001.
[8] LAKHOTIA D, SWAMINATHAN S, SHON WY, et al. Healing Process of Osteonecrotic Lesions of the Femoral Head Following Transtrochanteric Rotational Osteotomy: A Computed Tomography-Based Study. Clin Orthop Surg. 2017;9(1):29-36.
[9] 何宪顺, 韦雨柔, 何敏聪, 等. 活血通络法对激素性股骨头坏死囊性变患者血清骨吸收/成血管/成骨蛋白调节作用的研究[J].中国全科医学,2024,27(12):1504-1510.
[10] 何晓铭, 庞凤祥, 李子祺, 等. 基于“态靶结合”理论探讨股骨头坏死囊性变的辨治思路[J]. 辽宁中医杂志,2022,49(2):44-47.
[11] 魏腾飞, 肖方骏, 何晓铭, 等. 基于气血理论探讨囊性变在激素性股骨头坏死塌陷和修复中的意义[J].辽宁中医杂志,2024,51(10): 54-58.
[12] 魏秋实, 何伟, 张庆文, 等. 围塌陷期股骨头坏死不同影像学表现研究[J]. 中国修复重建外科杂志,2021,35(9):1105-1110.
[13] GAO F, HAN J, HE Z, et al. Radiological analysis of cystic lesion in osteonecrosis of the femoral head. Int Orthop. 2018;42(7):1615-1621.
[14] LIU GB, LI R, LU Q, et al. Three-dimensional distribution of cystic lesions in osteonecrosis of the femoral head. J Orthop Translat. 2020;22:109-115.
[15] 杨晓强, 肖欢, 田佳庆, 等. 活血通络胶囊对激素性股骨头坏死囊性变成血管修复的影响[J]. 中医正骨,2024,36(9):40-48.
[16] 彭鹏, 肖欢, 方伟华, 等. 激素性股骨头坏死囊性变组织骨修复机制分析与活血通络胶囊含药血清对肥大软骨细胞成骨分化影响的实验研究[J]. 中医正骨,2024,36(9):19-28.
[17] SHAPOURI-MOGHADDAM A, MOHAMMADIAN S, VAZINI H, et al. Macrophage plasticity, polarization, and function in health and disease. J Cell Physiol. 2018;233(9):6425-6440.
[18] VIOLA A, MUNARI F, SÁNCHEZ-RODRÍGUEZ R, et al. The Metabolic Signature of Macrophage Responses. Front Immunol. 2019;10:1462.
[19] ZHANG D, DANG Y, DENG R, et al. Research Progress of Macrophages in Bone Regeneration. J Tissue Eng Regen Med. 2023;2023:1512966.
[20] KOHARA Y, KITAZAWA R, HARAGUCHI R, et al. Macrophages are requisite for angiogenesis of type H vessels during bone regeneration in mice. Bone. 2022;154:116200.
[21] YAO Y, CAI X, REN F, et al. The Macrophage-Osteoclast Axis in Osteoimmunity and Osteo-Related Diseases. Front Immunol. 2021;12: 664871.
[22] ZHU X, LEE CW, XU H, et al. Phenotypic alteration of macrophages during osteoarthritis: a systematic review. Arthritis Res Ther. 2021; 23(1):110.
[23] CHAMPAGNE CM, TAKEBE J, OFFENBACHER S, et al. Macrophage cell lines produce osteoinductive signals that include bone morphogenetic protein-2. Bone. 2002;30(1):26-31.
[24] GOODMAN SB, MARUYAMA M. Inflammation, Bone Healing and Osteonecrosis: From Bedside to Bench. J Inflamm Res. 2020;13:913-923.
[25] ZHENG J, YAO Z, XUE L, et al. The role of immune cells in modulating chronic inflammation and osteonecrosis. Front Immunol. 2022;13: 1064245.
[26] LOI F, CORDOVA LA, PAJARINEN J, et al. Inflammation, fracture and bone repair. Bone. 2016;86:119-130.
[27] PAJARINEN J, LIN T, GIBON E, et al. Mesenchymal stem cell-macrophage crosstalk and bone healing. Biomaterials. 2019;196:80-89.
[28] LAM J, TAKESHITA S, BARKER JE, et al. TNF-alpha induces osteoclastogenesis by direct stimulation of macrophages exposed to permissive levels of RANK ligand. J Clin Invest. 2000;106(12):1481-1488.
[29] DUPLOMB L, BAUD’HUIN M, CHARRIER C, et al. Interleukin-6 inhibits receptor activator of nuclear factor kappaB ligand-induced osteoclastogenesis by diverting cells into the macrophage lineage: key role of Serine727 phosphorylation of signal transducer and activator of transcription 3. Endocrinology. 2008;149(7):3688-3697.
[30] PIRRACO RP, REIS RL, MARQUES AP. Effect of monocytes/macrophages on the early osteogenic differentiation of hBMSCs. J Tissue Eng Regen Med. 2013;7(5):392-400.
[31] Cho SW, Soki FN, Koh AJ, et al. Osteal macrophages support physiologic skeletal remodeling and anabolic actions of parathyroid hormone in bone. Proc Natl Acad Sci U S A. 2014;111(4):1545-1550.
[32] Wei F, Zhou Y, Wang J, et al. The Immunomodulatory Role of BMP-2 on Macrophages to Accelerate Osteogenesis. Tissue Eng Part A. 2018;24(7-8):584-594.
[33] Lu X, Gao J, Bao W, et al. Interaction of Macrophages with Bone Healing Microenvironment: Mechanism and Biomaterials. Tissue Eng Part B Rev. 2024;30(3):285-298.
[34] Schlundt C, Fischer H, Bucher CH, et al. The multifaceted roles of macrophages in bone regeneration: A story of polarization, activation and time. Acta Biomater. 2021;133:46-57.
[35] Kaur S, Raggatt LJ, Batoon L, et al. Role of bone marrow macrophages in controlling homeostasis and repair in bone and bone marrow niches. Semin Cell Dev Biol. 2017;61:12-21.
[36] Yao Y, Cai X, Ren F, et al. The Macrophage-Osteoclast Axis in Osteoimmunity and Osteo-Related Diseases. Front Immunol. 2021; 12:664871.
[37] Tang PM, Nikolic-Paterson DJ, Lan HY. Macrophages: versatile players in renal inflammation and fibrosis. Nat Rev Nephrol. 2019; 15(3):144-158.
[38] Wynn TA. Cellular and molecular mechanisms of fibrosis. J Pathol. 2008;214(2):199-210.
[39] Lu X, Gao J, Bao W, et al. Interaction of Macrophages with Bone Healing Microenvironment: Mechanism and Biomaterials. Tissue Eng Part B Rev. 2024;30(3):285-298.
[40] Weivoda MM, Bradley EW. Macrophages and Bone Remodeling. J Bone Miner Res. 2023;38(3):359-369.
[41] Ren Q, Xing W, Jiang B, et al.Tenascin-C promotes bone regeneration via inflammatory macrophages. Cell Death Differ. 2025; 32(4):763-775.
|