Chinese Journal of Tissue Engineering Research ›› 2024, Vol. 28 ›› Issue (24): 3922-3929.doi: 10.12307/2024.087
Previous Articles Next Articles
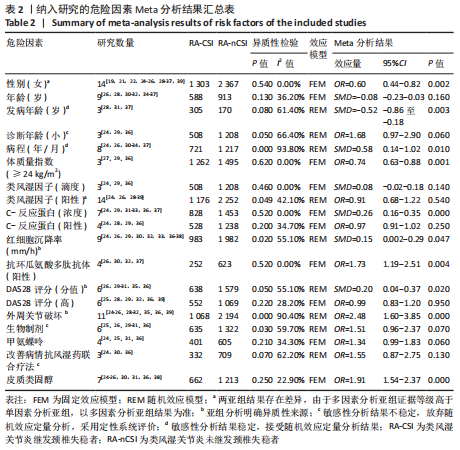
Meta-analysis of the incidence and related factors for cervical spine instability in patients with rheumatoid arthritis
Xu Chenghan1, 2, Zhuo Hanjie2, Chai Xubin2, Huang Yong2, Zhang Bowen2, Chen Qin1, 2, Hao Yupeng2, Li Lin2, Zhou Yingjie2
- 1Hunan University of Chinese Medicine, Changsha 410208, Hunan Province, China; 2Luoyang Orthopedic Traumatological Hospital of Henan Province (Henan Provincial Orthopedic Hospital), Luoyang 471002, Henan Province, China
-
Received:2023-04-12Accepted:2023-07-08Online:2024-08-28Published:2023-11-22 -
Contact:Zhou Yingjie, Master, Professor, Chief physician, Luoyang Orthopedic Traumatological Hospital of Henan Province (Henan Provincial Orthopedic Hospital), Luoyang 471002, Henan Province, China -
About author:Xu Chenghan, Master candidate, Physician, Hunan University of Chinese Medicine, Changsha 410208, Hunan Province, China; Luoyang Orthopedic Traumatological Hospital of Henan Province (Henan Provincial Orthopedic Hospital), Luoyang 471002, Henan Province, China -
Supported by:Traditional Chinese Medicine Inheritance and Innovative Talent Project (Zhongjing Project) (to ZYJ)
CLC Number:
Cite this article
Xu Chenghan, Zhuo Hanjie, Chai Xubin, Huang Yong, Zhang Bowen, Chen Qin, Hao Yupeng, Li Lin, Zhou Yingjie. Meta-analysis of the incidence and related factors for cervical spine instability in patients with rheumatoid arthritis[J]. Chinese Journal of Tissue Engineering Research, 2024, 28(24): 3922-3929.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
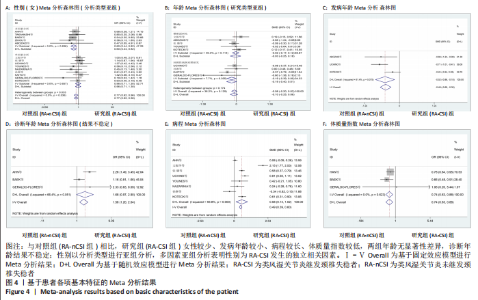
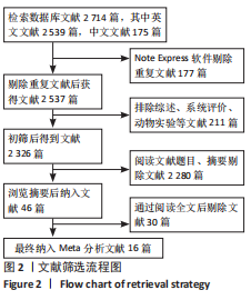
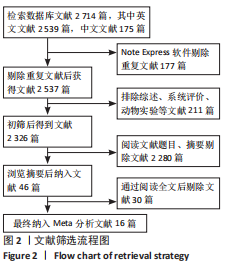
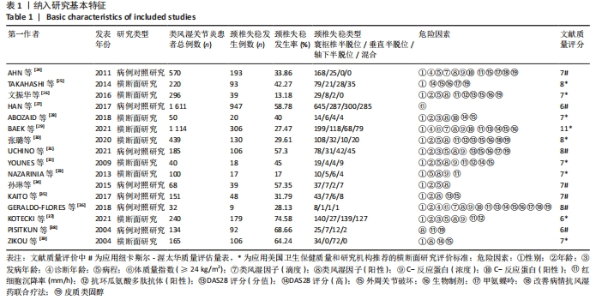
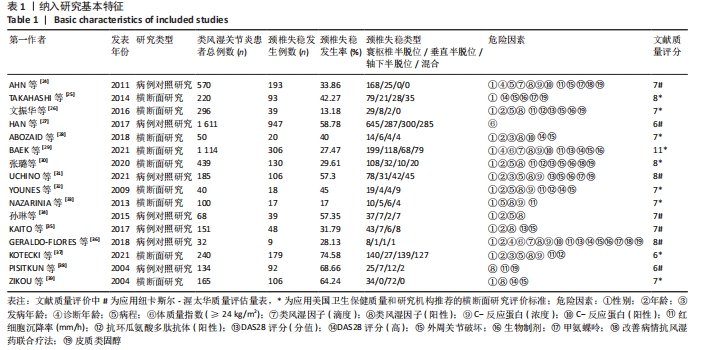
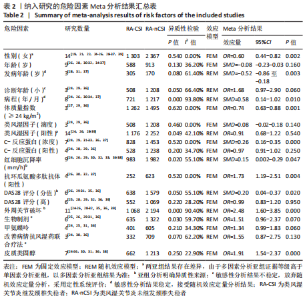
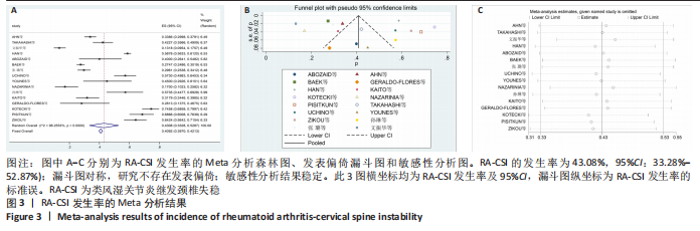
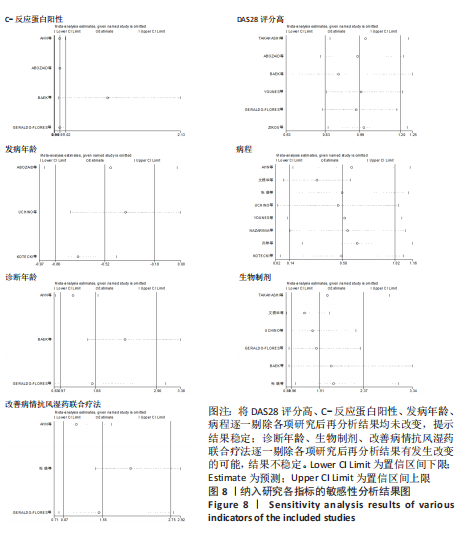
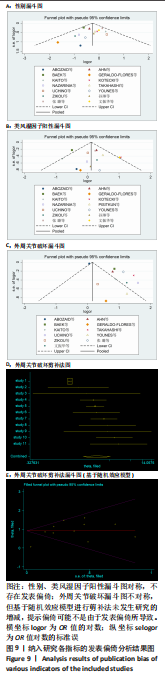
2.3.2 基于患者基本特征分析结果 (1)性别:14项研究报道了患者性别(女) [24-26,28-37,39],按照分析类型进行亚组分析结果显示,多因素分析亚组(OR=0.60,95%CI:0.44-0.82,P=0.002);单因素分析亚组(OR=0.96,95%CI:0.71-1.30,P=0.81);综合结果(OR=0.77,95%CI:0.62-0.96,P=0.02),两亚组分析结果出现差异,由于多因素分析证据等级高于单因素分析,且各研究间无异质性,以多因素分析亚组结果为准,提示女性为RA-CSI发生的独立保护因素,见图4A。 (2)年龄:共9项研究报道了患者年龄[26,28,30-32,34-37],按照研究类型进行亚组分析结果显示,横断面研究亚组(SMD=-0.02,95%CI:-0.17-0.12,P=0.74);病例对照研究亚组(SMD=-0.19,95%CI:-0.39-0.004,P=0.06);综合结果(SMD=-0.08,95%CI:-0.20-0.03,P=0.16),提示两组患者年龄无显著性差异,见图4B。 (3)发病年龄:共3项研究报道了患者发病年龄[28,31,37],结果显示,RA-CSI患者的发病年龄比RA-nCSI患者小(SMD=-0.52,95%CI:-0.86至-0.18,P=0.003) ,见图4C。 (4)诊断年龄:共3项研究报道了患者诊断年龄[24,29,36],Meta分析结果异质性较高,敏感性分析显示结果不稳定,放弃随机效应定量分析,采用定性系统评价,1项研究报道患者诊断年龄< 45岁是RA-CSI发生的危险因素[24],2项研究报道患者诊断年龄< 45岁不是RA-CSI发生的危险因素[29,36],见图4D。 (5)病程:共8项研究报道了患者病程[24,26,30-34,37],各研究间异质性较高,经亚组分析及敏感性分析无法降低异质性,经Meta回归无法明确异质性来源,敏感性分析结果稳定,采用随机效应进行Meta分析结果显示,RA-CSI患者病程较长(SMD=0.58,95%CI:0.14-1.02,P=0.01)。5项研究报道了患者病程校正OR值[24-26,28,39],分析结果异质性较高且敏感性分析显示结果不稳定,可能与分类变量节点选择不同有关,如研究分别以病程5年二分类、8年二分类或10年、20年三分类,因此放弃随机效应定量分析,采用定性系统评价,2项研究报道病程长是RA-CSI发生的危险因素[25-26],3项研究报道病程长对RA-CSI的发生无影响[24,28,39],见图4E。 (6) 体质量指数:共3项研究报道了患者体质量指数≥24 kg/m2 [27,29,36],结果显示,RA-CSI患者中体质量指数高的患者较少(OR=0.74,95%CI:0.63-0.88,P=0.001),见图4F。"
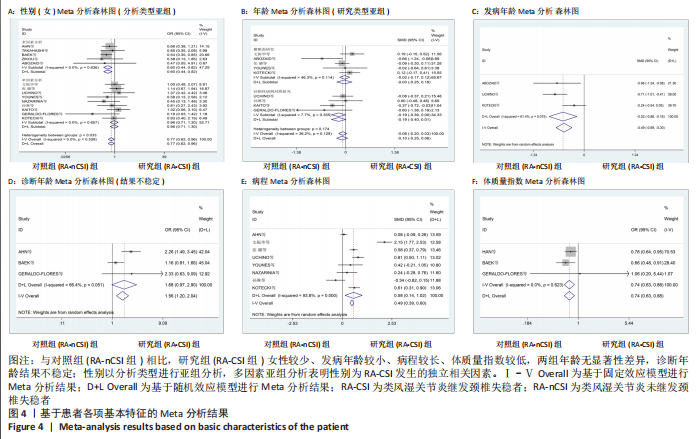
2.3.3 基于患者实验室检查及疾病活动度分析结果 (1)类风湿因子:共3项研究报道了患者类风湿因子滴度[24,29,36],结果显示,两组患者类风湿因子滴度无显著性差异(SMD=0.08,95%CI:-0.02-0.18,P=0.14)。有14项研究报道了患者类风湿因子阳性[24,26,28-39],按照分析类型进行亚组分析,多因素分析亚组(OR=0.91,95%CI:0.68-1.22,P=0.54);单因素分析亚组(OR=1.33,95%CI:1.02-1.72,P=0.04);综合结果(OR=1.17,95%CI:0.88-1.55,P=0.49),两亚组结果存在差异,其中类风湿因子阳性中单因素分析亚组与类风湿因子滴度的分析结果也不一致,但单因素分析亚组纳入研究更多且样本量较大,相较类风湿因子滴度的分析结果更有说服力,提示类风湿因子阳性是RA-CSI发生的非独立危险因素,见图5A,B。 (2) C-反应蛋白:共7项研究报道了患者C-反应蛋白浓度[24,29,31-33,36-37],按照研究类型进行亚组分析,横断面研究亚组 (SMD=0.31,95%CI:0.20-0.43,P=0.00);病例对照研究亚组(SMD=0.17,95%CI:0.02-0.31,P=0.03);综合结果(SMD=0.26,95%CI:0.16-0.35,P=0.00),提示RA-CSI患者C-反应蛋白浓度高。4项研究报道了患者C-反应蛋白阳性校正OR 值[24,28-29,36],存在权重过高(95.30%)研究[29],该研究为大样本量高质量研究,剔除该研究后结果未发生改变,提示结果稳定并接受此结果,结果显示,C-反应蛋白阳性对RA-CSI的发生无影响(OR=0.97,95%CI:0.91-1.02,P=0.25),综合两项Meta分析结果,C-反应蛋白是RA-CSI发生的非独立危险因素,见图5C,D。 (3)红细胞沉降率:共9项研究报道了患者红细胞沉降率速率[24,26,29-30,32-33,36-38],按照研究类型进行亚组分析,各组内异质性较低,整体存在高度异质性,说明研究类型为异质性来源,横断面研究亚组(SMD=0.05,95%CI:-0.05-0.14,P=0.32);病例对照研究亚组(SMD=0.33,95%CI:0.18-0.48,P=0.00);综合结果(SMD=0.15,95%CI:0.002-0.29,P=0.047),两亚组结果存在差异,横断面研究亚组患者红细胞沉降率速率一般于研究阶段统一收集检测,而病例对照研究亚组患者红细胞沉降率速率多通过历史病历资料获取,或为产生差异的主要原因,两亚组同属观察性研究,证据等级差别较小,因此以综合结果为准,提示RA-CSI患者红细胞沉降率浓度高。5项研究报道了患者红细胞沉降率加快(> 40 mm/h)[24,29,34,36,39],由于单一研究权重(99.98%)过高且该研究(OR=1.00,95%CI:1.00-1.01,P=0.007)无法提取更精确数据[29],Meta分析合并结果无显著性意义,采用定性系统评价,结果显示4项研究报道红细胞沉降率加快对RA-CSI的发生无影响[24,34,36,39],高权重研究报道红细胞沉降率加快是RA-CSI发生的危险因素[29],该研究为高质量大样文章,结果较为可信,见图5E。 (4)抗环瓜氨酸多肽抗体:共4项研究报道了患者抗环瓜氨酸多肽抗体阳性[26,30,32,37],按照研究类型进行亚组分析,组间组内均无异质性,结果显示,患者抗环瓜氨酸多肽抗体阳性是RA-CSI的危险因素(OR=1.73,95%CI:1.19-2.51,P=0.004),见图5F。 (5)DAS28评分:共6项研究报道了患者DAS28评分[26,29-31,33,35-36],按照数据类型(是否由四分位距转化)进行亚组分析,mean±SD亚组(SMD=0.44,95%CI:0.21-0.67,P=0.00);四分位距亚组(SMD=0.08,95%CI:-0.02-0.19,P=0.11);综合结果(SMD=0.20,95%CI:0.04-0.37,P=0.02),两亚组结果存在差异,或由于数据转换造成,以综合结果为准,提示RA-CSI患者DAS28评分较高。有6项研究报道了患者DAS28评分高对RA-CSI发生的影响[25,28-29,32,36,39],其中5项研究有校正OR值[25,28-29,36,39],存在权重过高(70.61%)研究[29],剔除该研究后结果未发生改变,提示结果稳定并接受此结果,结果显示,DAS28评分高对RA-CSI的发生无影响(OR=0.99,95%CI:0.83-1.20,P=0.95),见图5G-H。"

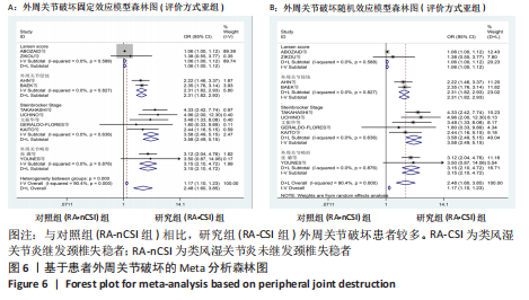
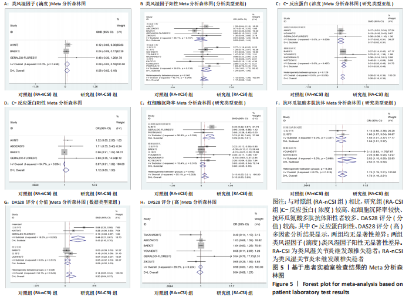
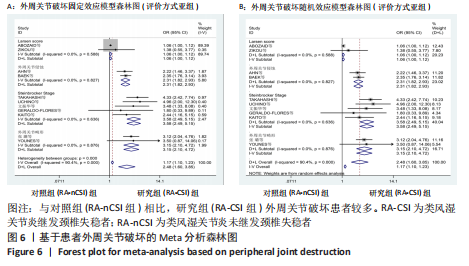
2.3.4 基于患者外周关节破坏分析结果 共11项研究报道了患者外周关节破坏[24-26,28-32,35-36,39],按照评价方式进行亚组分析,组内异质性较低,整体存在中度异质性,说明评价方式为异质性来源,Larsen评分亚组(OR=1.06,95%CI:0.995-1.12,P=0.07);外周关节侵蚀亚组(OR=2.31,95%CI:1.82-2.93,P=0.00);Steinbrocker分级亚组(OR=3.58,95%CI:2.49-5.15,P=0.00);关节畸形亚组(OR=3.15,95%CI:2.10-4.72,P=0.00);综合结果(OR=2.48,95%CI:1.60-3.85,P=0.00),以综合结果为准,提示外周关节破坏是RA-CSI发生的危险因素,Larsen评分亚组与其他亚组结果不一致,或与ABOZAID等[28]研究的样本量较少但研究精度与质量较高,在固定效应模型下权重过高有关,见图6。"
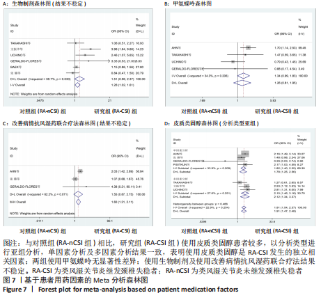
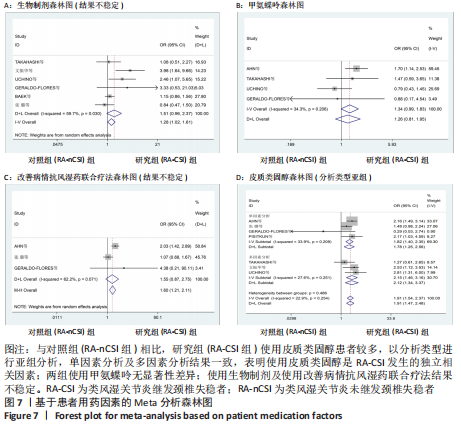
2.3.5 基于患者用药因素分析结果: (1)生物制剂:共6项研究报道了患者使用生物制剂[25-26,29-31,36],分析结果异质性较高,经亚组分析无法消除异质性且敏感性分析显示结果不稳定,放弃随机效应定量分析,采用定性系统评价,2项研究报道使用生物制剂在RA-CSI患者中更常见[26,31];有4项研究报道使用生物制剂对RA-CSI的发生无影响[25,29-30,36],见图 7A。 (2)甲氨蝶呤:共4项研究报道了患者使用甲氨蝶呤[24-25,31,36],结果显示,患者服用甲氨蝶呤对RA-CSI的发生无影响(OR=1.34,95%CI:0.99-1.83,P=0.06),见图 7B。 (3)改善病情抗风湿药联合疗法:共3项研究报道了患者使用改善病情抗风湿药联合疗法[24,30,36],分析结果异质性较高,敏感性分析显示结果不稳定,放弃随机效应定量分析,采用定性系统评价,1项研究报道使用改善病情抗风湿药联合疗法在RA-CSI患者中更常见[24],有2项研究报道使用改善病情抗风湿药联合疗法对RA-CSI的发生无影响[30,36],见图 7C。 (4)皮质类固醇:共7项研究报道了患者使用皮质类固醇[24-26,30-31,36,38],按照分析类型进行亚组分析,各组内及整体异质性较低,多因素分析亚组(OR=2.15,95%CI:1.46-3.16,P=0.00);单因素分析亚组(OR=1.82,95%CI:1.40-2.35,P=0.00);综合结果(OR=1.91,95%CI:1.54-2.37,P=0.00),各亚组结果一致且各研究间异质性较低,以综合结果为准,提示使用皮质类固醇是RA-CSI发生的独立危险因素,见图 7D。"
| [1] SHARIF K, SHARI A, JUMAH F, et al. Rheumatoid arthritis in review: clinical, anatomical, cellular and molecular points of view. Clin Anat. 2018;31(2):216-223. [2] CHU Y, WANG F, ZHOU M, et al. A preliminary study on the characterization of follicular helper T (Tfh) cells in rheumatoid arthritis synovium. Acta Histochem. 2014; 116(3):539-543. [3] YURUBE T, SUMI M, NISHID K, et al. Accelerated development of cervical spine instabilities in rheumatoid arthritis: a prospective minimum 5-year cohort study. PloS One. 2014;9(2):e88970. [4] MAŃCZAK M, GASIK R. Cervical spine instability in the course of rheumatoid arthritis - imaging methods. Reumatologia. 2017;55(4):201-207. [5] SHLOBIN NA, DAHDALEH NS. Cervical spine manifestations of rheumatoid arthritis: a review. Neurosurg Rev. 2021; 44(4):1957-1965. [6] CASEY AT, CROCKARD HA, BLAND JM, et al. Surgery on the rheumatoid cervical spine for the non-ambulant myelopathic patient-too much, too late? Lancet. 1996; 347(9007):1004-1007. [7] OMAR AM, PINTER ZW, STREUFERT BD, et al. C1-T2 decompression and fusion for C2 erosive pannus-a case report. Spinal Cord Ser Cases. 2021;7(1):64. [8] RADCLIFF KE, HUSSAIN MM, MOLDAVSKY M, et al. In vitro biomechanics of the craniocervical junction-a sequential sectioning of its stabilizing structures. Spine J. 2015;15(7):1618-1628. [9] PHUNTSOK R, ELLIS BJ, HERRON MR, et al. The occipitoatlantal capsular ligaments are the primary stabilizers of the occipitoatlantal joint in the craniocervical junction: a finite element analysis. J Neurosurg Spine. 2019. doi: 10.3171/2018.10.SPINE181102. [10] KAY J, UPCHURCH KS. ACR/EULAR 2010 rheumatoid arthritis classification criteria. Rheumatology(Oxford). 2012;51 Suppl 6:vi5-vi 9. [11] ARNETT FC, EDWORTHY SM, BLOCH DA, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988;31(3):315-324. [12] STANG A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603-605. [13] SHI J, LUO D, WAN X, et al. Detecting the skewness of data from the five-number su mmary and its application in meta-analysis. Stat Methods Med Res. 2023. doi: 10.1177/09622802231172043. [14] LUO D, WAN X, LIU J, et al. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res. 2018; 27(6):1785-1805. [15] WAN X, WANG W, LIU J, et al. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135. [16] MCGRATH S, ZHAO X, STEELE R, et al. Estimating the sample mean and standard deviation from co mmonly reported quantiles in meta-analysis. Stat Methods Med Res. 2020;29(9):2520-2537. [17] HORITA M, NISHIDA K, HASHIZUME K, et al. Prevalence of and Risk Factors for the Progression of Upper Cervical Lesions in Patients with Rheumatoid Arthritis. Acta Med Okayama. 2019;73(3):235-240. [18] INOUE T, HIGASHI T, KOBAYASHI N, et al. Risk factors associated with aggravation of cervical spine lesions in patients with rheumatoid arthritis: a retrospective longitudinal cohort study. Spine (Phila Pa 1976). 2022;47(6):484-489. [19] AL-DAOSERI HA, MOHA MMED SAEED MA, AHMED RA. Prevalence of cervical spine instability among rheumatoid arthritis patients in south Iraq. J Clin Orthop Trauma. 2020; 11(5):876-882. [20] LEBOUILLE-VELDMAN AB, SPENKELINK D, ALLAART CF, et al. The association between Disease Activity Score and rheumatoid arthritis-associated cervical deformity: radiological evaluation of the Best trial. J Neurosurg Spine. 2023;38(4):465-472. [21] NEVA MH, HÄKKINEN A, MÄKINEN H, et al. High prevalence of asymptomatic cervical spine subluxation in patients with rheumatoid arthritis waiting for orthopaedic surgery. Ann Rheum Dis. 2006;65(7):884-888. [22] 杨喜梅,薛苗,孟磊,等.老年类风湿关节炎患者颈椎失稳的影响因素[J].中国老年学杂志,2017,37(23):5918-5919. [23] OLÁH C, KARDOS Z, KOSTYÁL L, et al. Assessment of cervical spine involvement in rheumatoid arthritis patients in the era of biologics: a real-life, cross-sectional MRI study. Rheumatol Int. 2020;40(6):915-921. [24] AHN JK, HWANG JW, OH JM, et al. Risk factors for development and progression of atlantoaxial subluxation in Korean patients with rheumatoid arthritis. Rheumatol Int. 2011;31(10):1363-1368. [25] TAKAHASHI S, SUZUKI A, KOIKE T, et al. Current prevalence and characteristics of cervical spine instability in patients with rheumatoid arthritis in the era of biologics. Mod rheumatol. 2014;24(6):904-909. [26] 文振华,李敬扬,蒋会平,等.类风湿关节炎患者颈椎失稳的发生率及相关危险因素分析[J].中华风湿病学杂志,2016,20(5):299-303. [27] HAN MH, RYU JI, KIM CH, et al. Factors that predict risk of cervical instability in rheumatoid arthritis patients. Spine (Phila Pa 1976). 2017;42(13):966-973. [28] ABOZAID H, EL-DIN HASSAN RA, ELMADANY WA, et al. Is it the age at disease onset or the disease radiological severity that affects cervical spine involvement in patients with rheumatoid arthritis? Clin Med Insights Arthritis Musculoskelet Disord. 2018;11:1179544118759688. [29] BAEK IW, JOO YB, PARK KS, et al. Risk factors for cervical spine instability in patients with rheumatoid arthritis. Clin Rheumatol. 2021;40(2):547-555. [30] 张璐,胡小红,王庆文,等.类风湿关节炎合并颈椎失稳的人群分布及临床特征[J].北京大学学报(医学版), 2020,52(6):1034-1039. [31] UCHINO Y, HIGASHI T, KOBAYASHI N, et al. Risk factors associated with cervical spine lesions in patients with rheumatoid arthritis: an observational study. BMC Musculoskelet Disord. 2021;22(1):408. [32] YOUNES M, BELGHALI S, KRIÂA S, et al. Compared imaging of the rheumatoid cervical spine: prevalence study and associated factors. Joint Bone Spine. 2009;76(4):361-368. [33] NAZARINIA M, JALLI R, KAMALI SARVESTANI E, et al. Asymptomatic atlantoaxial subluxation in rheumatoid arthritis. Acta Med Iran. 2014;52(6):462-466. [34] 孙琳,张碧莹,刘蕊,等.类风湿关节炎引起颈椎半脱位的临床和影像学特点分析[J]. 中华风湿病学杂志, 2015,19(11):745-749. [35] KAITO T, OHSHIMA S, FUJIWARA H, et al. Incidence and risk factors for cervical lesions in patients with rheumatoid arthritis under the current pharmacologic treatment paradigm. Mod rheumatol. 2017;27(4):593-597. [36] GERALDO-FLORES NA, MERLOS-LÓPEZ RJ, RODRÍGUEZ-WONG JA, et al. The severity of rheumatoid arthritis as a timely predictor of instability in the asymptomatic cervical spine. Acta Ortop Mex. 2018;32(6):342-346. [37] KOTECKI M, GASIK R, GŁUSZKO P, et al. Radiological evaluation of cervical spine involvement in rheumatoid arthritis: a cross-sectional retrospective study. J Clin Med. 2021;10(19):4587. [38] PISITKUN P, PATTAROWAS C, SIRIWONGPAIRAT P, et al. Reappraisal of cervical spine subluxation in Thai patients with rheumatoid arthritis. Clin Rheumatol. 2004;23(1):14-18. [39] ZIKOU AK, ALAMANOS Y, ARGYROPOULOU MI, et al. Radiological cervical spine involvement in patients with rheumatoid arthritis: a cross sectional study. J Rheumatol. 2005;32(5):801-806. [40] JOAQUIM AF, GHIZONI E, TEDESCHI H, et al. Radiological evaluation of cervical spine involvement in rheumatoid arthritis. Neurosurg Focus. 2015;38(4):E4. [41] BAKER JF, OSTERGAARD M, GEORGE M, et al. Greater body mass independently predicts less radiographic progression on X-ray and MRI over 1-2 years. Ann Rheum Dis. 2014;73(11):1923-1928. [42] UKKOLA O, SANTANIEMI M. Adiponectin: a link between excess adiposity and associated comorbidities? J Mol Med (Berl). 2002;80(11):696-702. [43] BUGATTI S, BOGLIOLO L, MANZO A, et al. Impact of anti-citrullinated protein antibodies on progressive systemic bone mineral density loss in patients with early rheumatoid arthritis after two years of treat-to-target. Front Immunol. 2021;12:701922. [44] KIM KW, KIM BM, MOON HW, et al. Role of C-reactive protein in osteoclastogenesis in rheumatoid arthritis. Arthritis Res Ther. 2015;17(1):41. [45] YUAN J, XIONG X, ZHANG B, et al. Genetically predicted C-reactive protein mediates the association between rheumatoid arthritis and atlantoaxial subluxation. Front Endocrinol (Lausanne). 2022;13:1054206. [46] KAITO T, OHSHIMA S, FUJIWARA H, et al. Predictors for progression of two different types of cervical lesions in rheumatoid arthritis treated with biologic agents. J Orthop Sci. 2019;24(2):214-218. [47] SORIMACHI Y, IIZUKA H, ARA T, et al. Atlanto-axial joint of atlanto-axial subluxation patients due to rheumatoid arthritis before and after surgery: morphological evaluation using CT reconstruction. Eur Spine J. 2011;20(5):798-803. [48] LIAO S, JUNG MK, HÖRNIG L, et al. Injuries of the upper cervical spine-how can instability be identified? Int Orthop. 2020;44(7):1239-1253. [49] WANG Y, ZHAO R, GU Z, et al. Effects of glucocorticoids on osteoporosis in rheumatoid arthritis: a systematic review and meta-analysis. Osteoporos Int. 2020;31(8):1401-1409. [50] HUANG Y, CAI GQ, PENG JP, et al. Glucocorticoids induce apoptosis and matrix metalloproteinase-13 expression in chondrocytes through the NOX4/ROS/p38 MAPK pathway. J Steroid Biochem Mol Biol. 2018;181:52-62. [51] SMOLEN JS, LANDEWÉ R, BIJLSMA J, et al. EULAR reco mmendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2019 update. Ann Rheum Dis. 2020; 79(6):685-699. [52] XIE W, HUANG H, LI G, et al. Dynamical trajectory of glucocorticoids tapering and discontinuation in patients with rheumatoid arthritis co mmencing glucocorticoids with csDMARDs: a real-world data from 2009 to 2020. Ann Rheum Dis. 2021;80(8):997-1003. [53] VELDMAN AB, ALLAART CF, VLEGGEERT-LANKAMP C. The influence of reducing disease activity score on cervical spine deformity in rheumatoid arthritis: a systematic review. Biomed Res Int. 2022;2022:9403883. [54] KAITO T, OHSHIMA S, FUJIWARA H, et al. Predictors for the progression of cervical lesion in rheumatoid arthritis under the treatment of biological agents. Spine (Phila Pa 1976). 2013;38(26):2258-2263. [55] MÖLLER B, EVERTS-GRABER J, FLORENTINUS S, et al. Low hemoglobin and radiographic damage progression in early rheumatoid arthritis: secondary analysis from a phase iii trial. Arthritis Care Res (Hoboken). 2018;70(6):861-868. [56] HAN MH, RYU JI, KIM CH, et al. Influence of systemic bone mineral density on atlantoaxial subluxation in patients with rheumatoid arthritis. Osteoporos Int. 2017;28(6):1931-1938. |
| [1] | Zhong Jun, Wang Wen. Network meta-analysis of different anatomical repair strategies to improve chronic lateral ankle instability [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1470-1476. |
| [2] | Ma Shuwei, He Sheng, Han Bing, Zhang Liaoyun. Exosomes derived from mesenchymal stem cells in treatment of animals with acute liver failure: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(7): 1137-1142. |
| [3] | Zhang Zeyi, Yang Yimin, Li Wenyan, Zhang Meizhen. Effect of foot progression angle on lower extremity kinetics of knee osteoarthritis patients of different ages: a systematic review and meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 968-975. |
| [4] | Hu Zhixing, Li Qun, Yang Chao, Wang Xiaoxiao, Fang Luochangting, Hou Wuqiong, Lin Na, Chen Weiheng, Liu Chunfang, Lin Ya. Network meta-analysis of the modeling effects of different factors on rabbit models of steroid-induced osteonecrosis of femoral head [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 976-984. |
| [5] | Yu Zhaoyu, Tan Lixin, Sun Kai, Lu Yao, Li Yong. Meta-analysis of cement-augmented pedicle screw for thoracolumbar degenerative diseases with osteoporosis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(5): 813-820. |
| [6] | Abuduwupuer·Haibier, Alimujiang·Yusufu, Maihemuti·Yakufu, Maimaitimin·Abulimiti, Tuerhongjiang·Abudurexiti. Meta-analysis of efficacy and safety of terlipatide and bisphosphate in the treatment of postmenopausal osteoporosis fractures [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(4): 639-645. |
| [7] | Bai Xiaotian, Chen Zhaoying, Song Yiling, Wang Ye, Liu Jingmin. Effect of minimalist shoes on foot muscle morphology: systematic evaluation and Meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(4): 646-650. |
| [8] | Wang Juan, Wang Ling, Zuo Huiwu, Zheng Cheng, Wang Guanglan, Chen Peng. Rehabilitative efficacy of kinesio taping following anterior cruciate ligament reconstruction: a Meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(4): 651-656. |
| [9] | Wang Yuetong, Peng Liang, Su Yuying, Liu Jiajun. Effect of balance training on chronic ankle instability: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(24): 3930-3936. |
| [10] | Wu Ruiqi, Zhou Yi, Xia Tian, Zhang Chi, Yang Qipei, Zhang Xuan, Zhang Yazhong, Cui Wei. Mendelian randomization study on the association between rheumatoid arthritis and osteoporosis and bone mineral density [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(23): 3715-3721. |
| [11] | Dong Kuan, Xu Chengli, Tian Jing, Xu Changchun. Effects of endurance training with blood flow restriction on aerobic capacity, lower limb muscle strength, and sports performance: a Meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(23): 3766-3772. |
| [12] | Chang Wanpeng, Zhang Zhongwen, Yang Yulin, Zi Yang, Yang Mengqi, Du Bingyu, Wang Nan, Yu Shaohong. Efficacy of rehabilitation exoskeleton robots on post-stroke lower limb motor dysfunction: a Meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(2): 321-328. |
| [13] | Ran Lei, Han Haihui, Xu Bo, Wang Jianye, Shen Jun, Xiao Lianbo, Shi Qi. Molecular docking analysis of the anti-inflammatory mechanism of Cibotium barometz and Epimedium for rheumatoid arthritis: animal experiment validation [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(2): 208-215. |
| [14] | Zhang Guoxu, Zeng Jianbo, Li Jing, Xie Qijun, Zhou Guanbin, Guan Jianhao, Chen Wenchuang, Chen Haiyun. Meta-analysis of efficacy of orthopedic robot-assisted versus freehand percutaneous sacroiliac screw fixation for posterior pelvic ring fractures [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(18): 2932-2938. |
| [15] | Wang Ke, Zhang Zeyi, Zhang Liwen, Zhang Meizhen. Biomechanics characteristics during sitting up in knee osteoarthritis patients of different ages: a systematic review and meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(18): 2939-2946. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||