Chinese Journal of Tissue Engineering Research ›› 2024, Vol. 28 ›› Issue (5): 813-820.doi: 10.12307/2023.980
Meta-analysis of cement-augmented pedicle screw for thoracolumbar degenerative diseases with osteoporosis
Yu Zhaoyu1, Tan Lixin2, Sun Kai3, Lu Yao1, Li Yong1
- 1Third Department of Orthopedics, Zhuhai Branch, Guangdong Provincial Hospital of Chinese Medicine, Zhuhai 519000, Guangdong Province, China; 2Second Clinical Medicine College, Guangzhou University of Chinese Medicine, Guangzhou 510080, Guangdong Province, China; 3Department of Orthopedics, Ezhou Hospital of Traditional Chinese Medicine, Ezhou 436000, Hubei Province, China
-
Received:2022-11-26Accepted:2023-01-31Online:2024-02-18Published:2023-08-17 -
Contact:Li Yong, Chief physician, Third Department of Orthopedics, Zhuhai Branch, Guangdong Provincial Hospital of Chinese Medicine, Zhuhai 519000, Guangdong Province, China -
About author:Yu Zhaoyu, Doctoral candidate, Attending physician, Third Department of Orthopedics, Zhuhai Branch, Guangdong Provincial Hospital of Chinese Medicine, Zhuhai 519000, Guangdong Province, China -
Supported by:Zhuhai Science and Technology Plan Project, No. 2220004000345 (to YZY)
CLC Number:
Cite this article
Yu Zhaoyu, Tan Lixin, Sun Kai, Lu Yao, Li Yong. Meta-analysis of cement-augmented pedicle screw for thoracolumbar degenerative diseases with osteoporosis[J]. Chinese Journal of Tissue Engineering Research, 2024, 28(5): 813-820.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
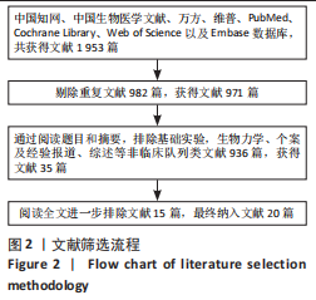
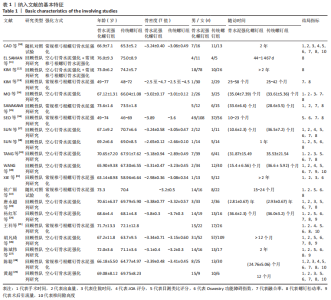
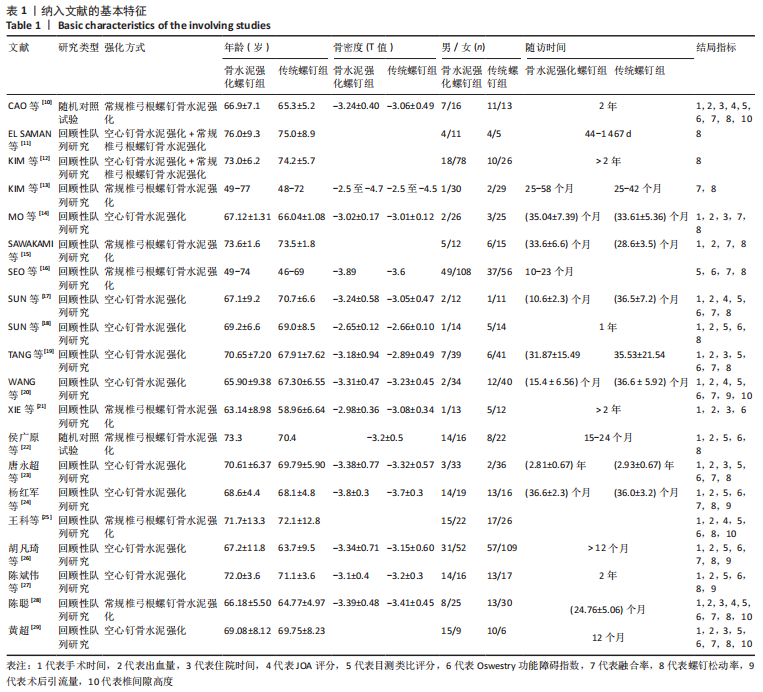
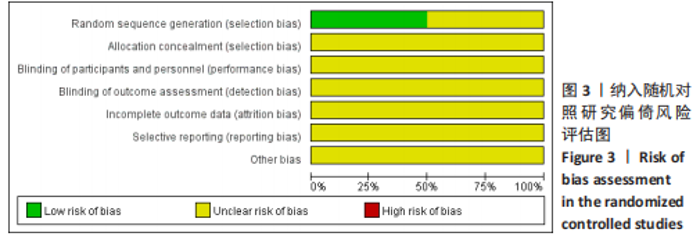
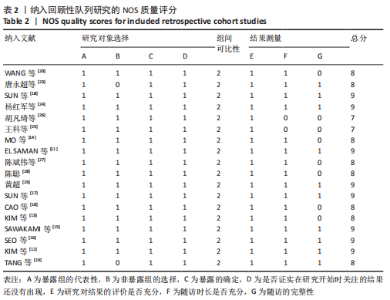
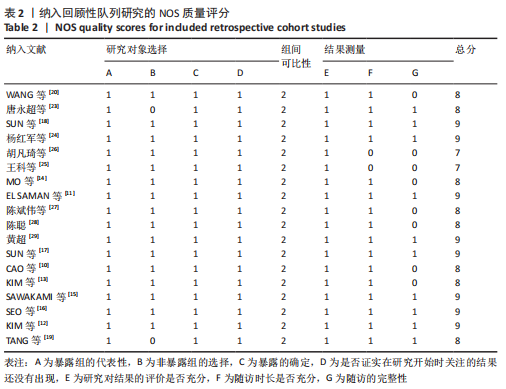
2.1 文献检索结果及质量评价 初步检索到1 953篇文献,查重后获取文献971篇,阅读文献标题及摘要后,剔除明显不相符文献,剩余35篇文献,仔细阅读全文,按标准进行严格筛选,最终纳入20篇文献[10-29],具体过程见图2。纳入文献的基本特征见表1。其中2篇为随机对照试验[10,22],均未提及分配隐藏及盲法,文献质量评价结果见图3。18篇为回顾性队列研究[11-21,23-29],质量评价结果见表2。所有研究共涉及1 566例患者,其中骨水泥强化螺钉组789例,常规螺钉组777例。15项研究提及了骨水泥强化螺钉组有不同程度骨水泥渗漏[10,12,14,16-19,21-24,26-29],3项研究未出现骨水泥渗漏[13,15,25],其他均未提及骨水泥渗漏情况。6项研究提及患者出现不同部位好转,治疗后均好转[15-16,18-20,29]。1项研究有3例患者术口不愈合,需行二期缝合[16]。1项研究未提及任何不良反应发生与否[11],其他研究均未出现神经、脊髓损伤等重大不良反应。"
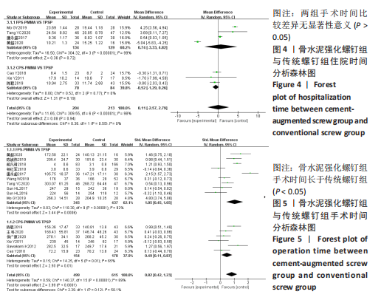
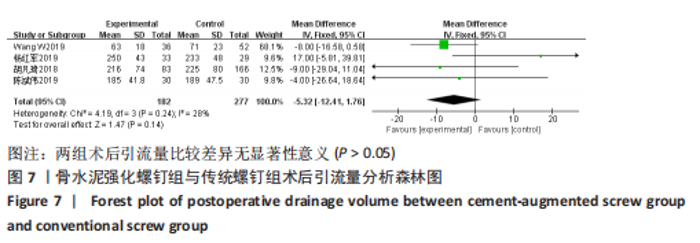
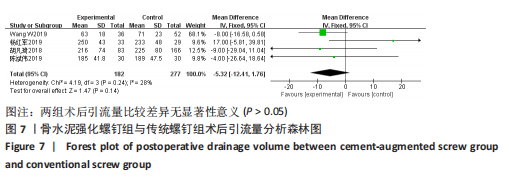
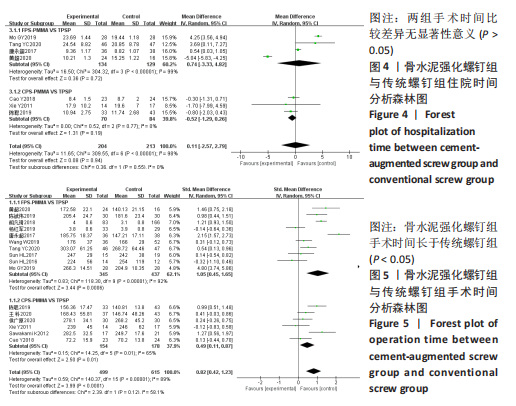
2.2 Meta分析结果 2.2.1 住院时间 7项研究报告了417例患者的住院时间[10,14,19,21,23,28-29],各研究有明显异质性(I2=98%,P < 0.000 01),遂采用随机效应模型,结果显示两组住院时间比较差异无显著性意义(MD=0.11,95%CI:-2.57,2.79),P=0.94),如图4所示。按照不同骨水泥螺钉强化方式进行亚组分析,4项研究比较了空心钉骨水泥强化组与传统椎弓根螺钉的手术时间[14,19,23,29],结果显示两组住院时间比较差异无显著性意义(MD=0.74,95%CI:-3.33,4.82,P=0.72)。3项研究比较了常规椎弓根螺钉强化组与传统椎弓根螺钉组的手术时间[10,21,28],结果表显示两组手术时间比较差异无显著性意义(MD=-0.52,95%CI:-1.29,0.26,P=0.19)。 2.2.2 手术时间 16项研究报告了1 114例患者的手术时间[10,14-15,17-29],各研究间异质性较大(I2=89%,P < 0.000 01),故采用随机效应模型,采用SMD表示其效应量(各计量资料单位不一致),结果表明两组手术时间比较差异有显著性意义(SMD=0.82,95%CI:0.42,1.23,P < 0.000 1),骨水泥强化螺钉组手术时间相对更长。按照不同骨水泥强化方式进行亚组分析,10项研究比较了空心钉水泥强化组与传统椎弓根螺钉的手术时间[14,17-20,23-24,26-27,29],结果显示空心钉骨水泥强化组手术时间要多于传统螺钉组(SMD=1.05,95%CI:0.45,1.65,P=0.000 6)。6项研究比较了常规椎弓根螺钉强化组与传统椎弓根螺钉组的手术时间[10,15,21-22,25,28],结果显示常规椎弓根螺钉强化组手术时间要长于传统椎弓根螺钉组(SMD=0.49,95%CI:0.11,0.87,P=0.01),见图5。 "
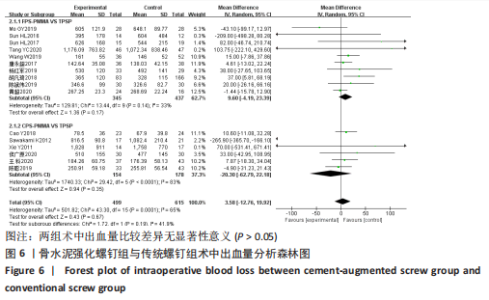
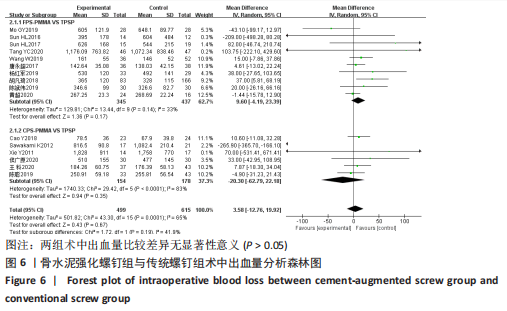
2.2.3 术中出血量 16项研究报告了1 114例患者的术中出血量[10,14-15,17-29],各研究间异质性较大(I2=65%,P=0.000 1),遂采用随机效应模型,结果显示两组术中出血量比较差异无显著性意义(MD=3.58,95%CI:-12.76,19.92,P=0.67)。按照不同骨水泥螺钉强化方式进行亚组分析,10项研究比较了空心钉骨水泥强化组与传统椎弓根螺钉组的术中出血量[14,17-20,23-24,26-27,29],结果显示两亚组术中出血量比较差异无显著性意义(MD=9.60,95%CI:-4.19,23.39,P=0.17);6项研究比较了空心钉骨水泥强化组与传统椎弓根螺钉组的术中出血量[10,15,21-22,25,28],结果显示两亚组术中出血量比较差异无显著性意义(MD=-20.30,95%CI:-62.79,22.18,P=0.35),见图6。"
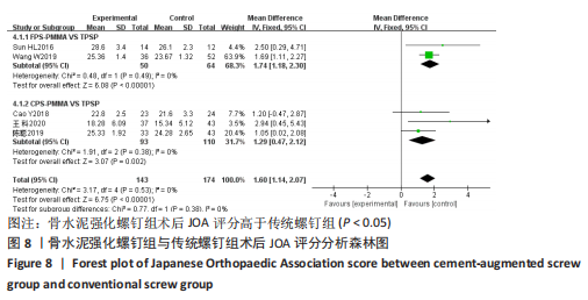
2.2.5 术后JOA评分 5项研究报告了末次随访JOA评分[10,17,20,25,28],共计317例患者,各研究间无明显异质性(I2=0%,P=0.53),故采用固定效应模型,结果显示骨水泥强化螺钉组末次随访JOA评分高于传统螺钉组(MD=1.60,95%CI:1.14,2.07,P < 0.000 01)。按照不同骨水泥螺钉强化方式进行亚组分析,2项研究比较了空心钉水泥强化组与传统椎弓根螺钉组的JOA评分[17,20],结果显示空心钉骨水泥强化组末次随访JOA评分高于传统螺钉组(MD=1.74,95%CI:1.18,2.30,P < 0.000 01);3项研究比较了常规椎弓根螺钉强化组与传统螺钉组的JOA评分[10,25,28],结果显示常规椎弓根螺钉强化组末次随访JOA评分显著高于传统螺钉组(MD=1.29,95%CI:0.47,2.12,P=0.002),见图8。"

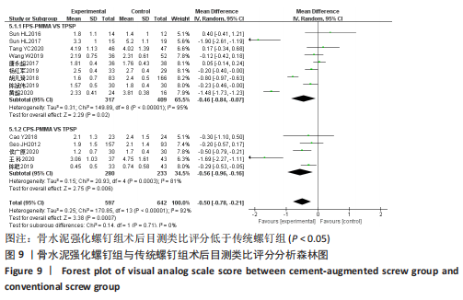
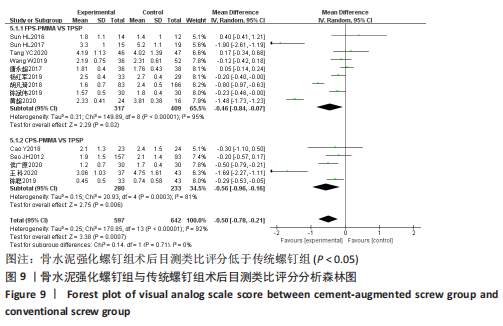
2.2.6 术后目测类比评分 14项研究报告了1 239例患者的末次随访目测类比评分[10,16-20,22-29],各研究间异质性较大(I2=92%,P < 0.000 01),故采用随机效应模型,结果显示骨水泥强化螺钉组末次随访目测类比评分低于传统螺钉组(MD=-0.50,95%CI:-0.78,-0.21,P=0.000 7)。按照不同骨水泥螺钉强化方式进行亚组分析,9项研究比较了空心钉骨水泥强化组与传统螺钉组的目测类比评分[17-20,23-24,26-27,29],结果显示空心钉骨水泥强化末次随访目测类比评分低于传统螺钉组(MD=-0.46,95%CI:-0.84,-0.07,P=0.02);5项研究比较了常规椎弓根螺钉强化组与传统螺钉组的目测类比评分[10,16,22,25,28], 结果显示常规椎弓根螺钉强化组末次随访目测类比评分低于传统螺钉组(MD=-0.56,95%CI:-0.96,-0.16,P=0.006),见图9。"
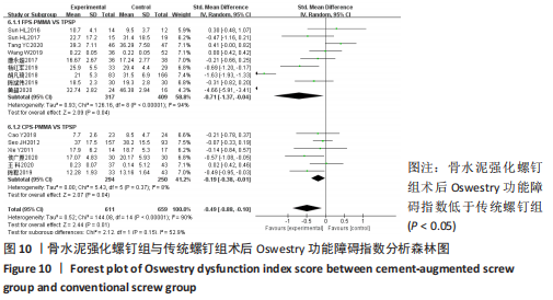
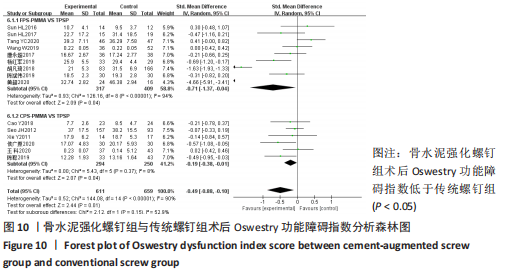
2.2.7 术后Oswestry 功能障碍指数 15项研究报告了1 270例患者的末次随访Oswestry功能障碍指数[10,16-29],各研究间异质性较大(I2=90%,P < 0.000 01),采用随机效应模型,因单位不一致,故采用SMD作为效应量,结果显示骨水泥强化螺钉组末次随访Oswestry功能障碍指数低于传统螺钉组(SMD=-0.49,95%CI:-0.88,-0.10,P=0.01)。按照不同骨水泥螺钉强化方式进行亚组分析,9项研究比较了空心钉骨水泥强化组与传统螺钉组的Oswestry功能障碍指数[17-20,23-24,26-27,29],结果显示空心钉骨水泥强化组末次随访Oswestry功能障碍指数低于传统螺钉组(SMD=-0.71,95%CI:-1.37,-0.04,P=0.04);6项研究比较了常规椎弓根螺钉强化组与传统螺钉组的Oswestry功能障碍指数[10,16,21-22,25,28],结果显示常规椎弓根螺钉强化组末次随访Oswestry功能障碍指数低于传统螺钉组(MD=-0.19,95%CI:-0.38,-0.01,P=0.04),见图10。"
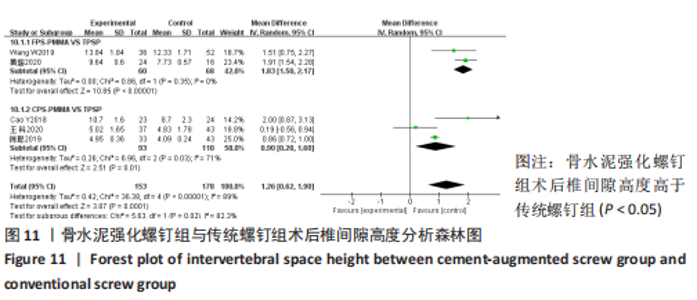
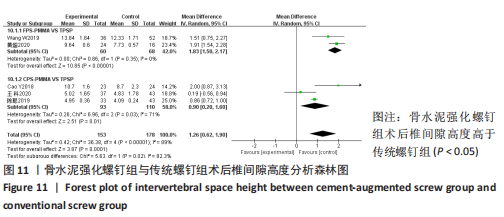
2.2.8 术后椎间隙高度 5项研究报告了末次随访椎间隙高度[10,20,25,28-29],包含331例患者,各研究间异质性较大(I2=89%,P < 0.000 01),故采用随机效应模型,结果显示两组术后椎间隙高度比较差异有显著性意义(MD=1.26,95%CI:0.62,1.90,P=0.000 1)。按照不同骨水泥螺钉强化方式进行亚组分析,2项研究比较了空心钉骨水泥强化组与传统螺钉固定组的椎间隙高度[20,29],结果显示空心钉骨水泥强化组末次随访椎间隙高度大于传统螺钉组(MD=1.83,95%CI:1.50,2.17,P < 0.000 01);3项研究比较了常规椎弓根螺钉强化组与传统螺钉组的椎间隙高度[10,25,28],结果显示常规椎弓根螺钉强化组末次随访椎间隙高度高于传统螺钉组(MD=0.90,95%CI:0.20,1.60,P=0.01),见图11。"
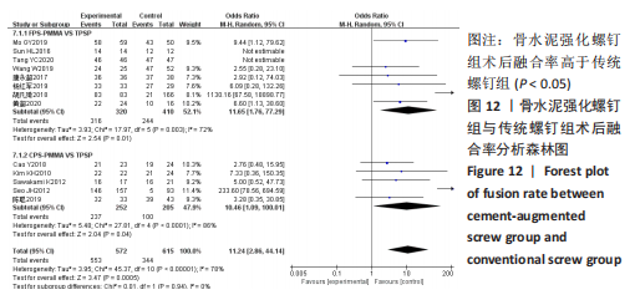
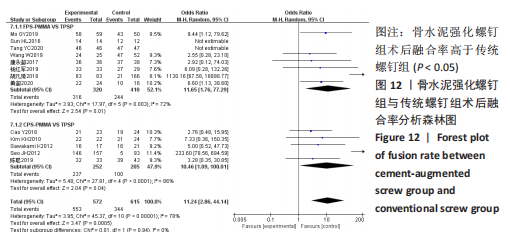
2.2.9 术后融合率 13项研究报告了1 187例患者的末次随访融合率[10,13-17,19-20,23-24,26,28-29],各研究间异质性较大(I2=78%,P < 0.000 01),故采用随机效应模型,分析结果OR=11.24,95%CI:2.86,44.14,P=0.000 5,表明骨水泥强化螺钉组患者末次随访融合率高于传统螺钉组。按照不同骨水泥螺钉强化方式进行亚组分析,8项研究比较了空心钉骨水泥强化组与传统椎弓根螺钉组的融合率[14,17,19-20,23-24,26,29],分析结果表明空心钉骨水泥强化组末次随访融合率高于传统椎弓根螺钉组(OR=11.65,95%CI:1.76,77.29,P=0.01);5项研究比较了常规椎弓根螺钉强化与传统椎弓根螺钉固定的融合率[10,13,15-16,28],分析结果表明常规椎弓根螺钉强化组末次随访融合率高于传统椎弓根螺钉组(OR=10.46,95%CI:1.09,100.01,P=0.04),见图12。"
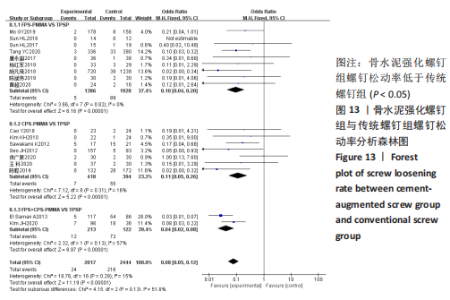
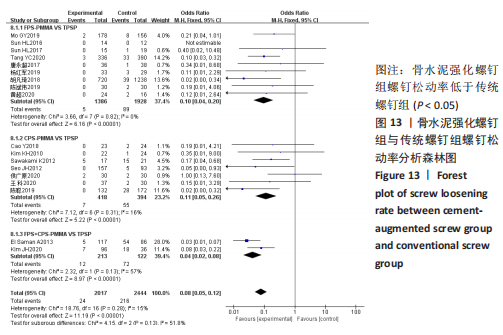
2.2.10 螺钉松动率 18项研究报告了末次随访松钉率[10-19,22-29],共计1 447例患者,各研究间异质性较小(I2=15%,P=0.28),故采用固定效应模型,结果显示骨水泥强化螺钉组末次随访螺钉松动率低于传统螺钉组(OR=0.08,95%CI:0.05,0.12,P < 0.000 01)。按照不同骨水泥螺钉强化方式进行亚组分析,9项研究比较了空心钉骨水泥强化组与传统螺钉组的螺钉松动率[14,17-19,23-24,26-27,29],结果显示空心钉骨水泥强化组末次随访松钉率低于传统螺钉组(OR=0.10,95%CI:0.04,0.20,P < 0.000 01);7项研究比较了常规椎弓根螺钉强化组与传统螺钉组的螺钉松动率[10,13,15-16,22,25,28],结果显示常规椎弓根螺钉强化组末次随访螺钉松动率低于传统螺钉组(OR=0.11,95%CI:0.05,0.26,P < 0.000 01);2项研究比较了椎弓根螺钉混合强化组(包含空心钉强化与常规螺钉强化)与传统螺钉组的螺钉松动率[11-12],结果显示椎弓根螺钉混合强化组末次随访松钉率低于传统螺钉组(OR=0.04,95%CI:0.02,0.08,P < 0.000 01),见图13。"
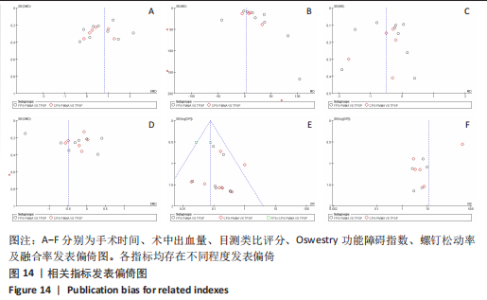
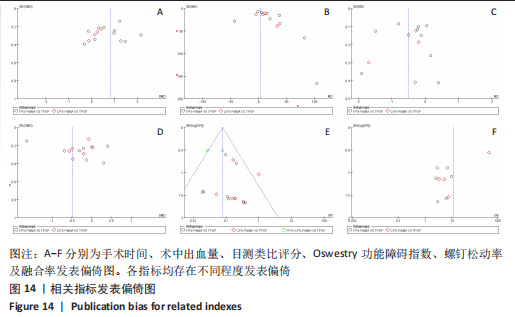
2.3 敏感性分析 对于手术时间进行逐一剔除研究后重新合并分析,发现异质性无明显变化,且两组比较结果与之前一致,提示Meta分析结果相对可靠。考虑不同研究手术节段、手术难度及医生技术水平差异导致研究间异质性较大。 对于住院时间进行逐一剔除研究后重新合并分析,发现异质性无明显变化,且两组比较结果与之前一致,提示Meta分析结果相对可靠。考虑各研究术后干预措施不同、患者经济水平差异导致的研究间异质性较大。 对于目测类比评分、Oswestry 功 能 障 碍 指 数、融合率、椎间隙高度进行逐一剔除研究后重新合并分析,发现异质性无明显变化,且两组比较结果与之前一致,提示Meta分析结果相对可靠。考虑各研究术后随访时长不同导致各研究间异质性较大。 对于术中出血量,敏感性分析提示1项研究可能为异质性来源,剔除该项研究后重新进行合并分析发现异质性明显减少(I2=6%),采用固定效应模型分析,结果表明两组患者术中出血量仍无统计学差异(MD=6.66,95%CI:-0.94,14.26,P=0.09),提示Meta分析结果相对可靠。异质性可能是各研究手术难度不同造成的。 2.4 发表偏倚分析 研究中纳入的手术时间、术中出血量、目测类比评分、Oswestry 功能障碍指数评分、融合率及松钉率的文献均不少于10篇,一般认为10篇文献以上可做漏斗图分析,故对以上指标进行发表偏倚分析,结果显示,各指标均存在不同程度发表偏倚,见图14。"
| [1] TUOMAINEN I, PAKARINEN M, AALTO T, et al. Depression is associated with the long-term outcome of lumbar spinal stenosis surgery: a 10-year follow-up study. Spine J. 2018;18(3):458-463. [2] 中华医学会骨质疏松和骨矿盐疾病分会.中国骨质疏松症流行病学调查及“健康骨骼”专项行动结果发布[J].中华骨质疏松和骨矿盐疾病杂志,2019,12(4):317-318. [3] YOUNG JJ, JENSEN RK, HARTVIGSEN J, et al. Prevalence of multimorbid degenerative lumbar spinal stenosis with knee or hip osteoarthritis: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2022;23(1):177. [4] MARIE-HARDY L, PASCAL-MOUSSELLARD H, BARNABA A, et al. Screw Loosening in Posterior Spine Fusion: Prevalence and Risk Factors. Global Spine J. 2020;10(5):598-602. [5] TANDON V, FRANKE J, KALIDINDI KKV. Advancements in osteoporotic spine fixation. J Clin Orthop Trauma. 2020;11(5):778-785. [6] SAKAURA H, IKEGAMI D, FUJIMORI T, et al. Early cephalad adjacent segment degeneration after posterior lumbar interbody fusion: a comparative study between cortical bone trajectory screw fixation and traditional trajectory screw fixation. J Neurosurg Spine. 2019;32(2):155-159. [7] GAZZERI R, PANAGIOTOPOULOS K, GALARZA M, et al. Minimally invasive spinal fixation in an aging population with osteoporosis: clinical and radiological outcomes and safety of expandable screws versus fenestrated screws augmented with polymethylmethacrylate. Neurosurg Focus. 2020;49(2):E14. [8] JANG SH, LEE JH, CHO JY, et al. The efficacy of hydroxyapatite for screw augmentation in osteoporotic patients. Neurol Med Chir. 2013; 53(12):875e881. [9] HOPPE S, KEEL MJ. Pedicle screw augmentation in osteoporotic spine: indications, limitations and technical aspects. Eur J Trauma Emerg Surg. 2017;43(1):3-8. [10] CAO Y, LIANG Y, WAN S, et al. Pedicle Screw with Cement Augmentation in Unilateral Transforaminal Lumbar Interbody Fusion: A 2-Year Follow-Up Study. World Neurosurg. 2018;118:e288-e295. [11] EL SAMAN A, MEIER S, SANDER A, et al. Reduced loosening rate and loss of correction following posterior stabilization with or without PMMA augmentation of pedicle screws invertebral fractures in the elderly. Eur J Trauma Emerg Surg. 2013;39(5):455-460. [12] KIM JH, AHN DK, SHIN WS, et al. Clinical Effects and Complications of Pedicle Screw Augmentation with Bone Cement: Comparison of Fenestrated Screw Augmentation and Vertebroplasty Augmentation. Clin Orthop Surg. 2020;12(2):194-199. [13] KIM KH, LEE SH, LEE DY, et al. Anterior bone cement augmentation in anterior lumbar interbody fusion and percutaneous pedicle screw fixation in patients with osteoporosis. J Neurosurg Spine. 2010;12(5):525-532. [14] MO GY, GUO HZ, GUO DQ, et al. Augmented pedicle trajectory applied on the osteoporotic spine with lumbar degenerative disease: mid-term outcome. J Orthop Surg Res. 2019; 14(1):170. [15] SAWAKAMI K, YAMAZAKI A, ISHIKAWA S, et al. Polymethylmethacrylate augmentation of pedicle screws increases the initial fixation in osteoporotic spine patients. J Spinal Disord Tech. 2012;25(2):E28-35. [16] SEO JH, JU CI, KIM SW, et al. Clinical efficacy of bone cement augmented screw fixation for the severe osteoporotic spine. Korean J Spine. 2012;9(2):79-84. [17] SUN HL, LI CD, YANG ZC, et al. Polymethylmethacrylate augmentation of bone cement-injectable cannulated pedicle screws for the treatment of degenerative lumbar diseases with osteoporosis. Beijing Da Xue Xue Bao Yi Xue Ban. 2016;48(6):1019-1025. [18] SUN HL, LI CD, LI XW, et al. Polymethylmethacrylate augmentation of bone cement injectable cannulated pedicle screws was used to treat degenerative lumbar scoliosis with osteoporosis. Beijing Da Xue Xue Bao Yi Xue Ban. 2017;49(2):256-261. [19] TANG YC, GUO HZ, GUO DQ, et al. Effect and potential risks of using multilevel cement-augmented pedicle screw fixation in osteoporotic spine with lumbar degenerative disease. BMC Musculoskelet Disord. 2020; 21(1):274. [20] WANG W, LIU C, LI J, et al. Comparison of the fenestrated pedicle screw and conventional pedicle screw in minimally percutaneous fixation for the treatment of spondylolisthesis with osteoporotic spine. Clin Neurol Neurosurg. 2019;183:105377. [21] XIE Y, FU Q, CHEN ZQ, et al. Comparison between two pedicle screw augmentation instrumentations in adult degenerative scoliosis with osteoporosis. BMC Musculoskelet Disord. 2011;12:286. [22] 侯广原,张继学,张志军,等.骨水泥强化椎弓根螺钉内固定治疗伴骨质疏松腰椎退行性疾病的1年随访[J].中国组织工程研究, 2021,25(6):878-883. [23] 唐永超,梁德,陈博来,等.骨水泥钉道强化与否治疗伴骨质疏松的单节段腰椎退行性疾病的临床对照研究[J].中国脊柱脊髓杂志,2017,27(12):1092-1098. [24] 杨红军,苏高建,冯智海,等.新型骨水泥椎弓根螺钉内固定系统治疗重度骨质疏松腰椎退变性疾病的临床研究[J].中国骨与关节杂志,2019,8(9):703-708. [25] 王科,路琪,陆锡平.骨水泥强化椎弓根螺钉内固定治疗骨质疏松伴腰椎退行性疾病效果及影响因素分析[J].河北医学,2020, 26(8):1246-1251. [26] 胡凡琦,胡文浩,张昊,等.骨水泥强化椎弓根螺钉技术治疗合并骨质疏松脊柱疾病的疗效观察[J].解放军医学院学报,2018,39(6):470-476. [27] 陈斌伟,廖壮文,黄帅,等.可注射骨水泥椎弓根钉内固定术治疗伴骨质疏松的多节段腰椎管狭窄症的疗效[J].实用医学杂志, 2019,35(24):3793-3797. [28] 陈聪.骨水泥强化椎弓根螺钉治疗骨质疏松性腰椎退变疾病的疗效观察[D].扬州:扬州大学,2019. [29] 黄超.骨水泥螺钉治疗老年腰椎滑脱患者疗效分析[D].长沙:湖南师范大学,2020. [30] CHIN DK, PARK JY, YOON YS, et al. Prevalence of osteoporosis in patients requiring spine surgery: incidence and significance of osteoporosis in spine disease. Osteoporos Int. 2007;18(9):1219-1224. [31] 高明暄,周胜虎,邓晓文,等.骨质疏松对椎弓根螺钉稳定性影响的实验研究[J].中国骨质疏松杂志,2013,19(1):39-42. [32] WEISER L, SEHMISCH S, LEHMANN W, et al. Techniques to increase pedicle screw stability in osteoporotic vertebrae. Oper Orthop Traumatol. 2019;31(4):284-292. [33] ZHUANG XM, YU BS, ZHENG ZM, et al. Effect of the degree of osteoporosis on the biomechanical anchoring strength of the sacral pedicle screws: an in vitro comparison betweenunaugmented bicortical screws and polymethylmethacrylate aug-mented unicortical screws. Spine (Phila Pa 1976). 2010; 35(19):E925-E931. [34] MCCOY S, TUNDO F, CHIDAMBARAM S, et al. Clinical considerations for spinal surgery in the osteoporotic patient: A comprehensive review. Clin Neurol Neurosurg. 2019;180:40-47. [35] LEHMAN RA JR, KANG DG, WAGNER SC. Management of osteoporosis in spine surgery. J Am Acad Orthop Surg. 2015;23(4):253-263. [36] ERDEM MN, KARACA S, SARı S, et al. Application of cement on strategic vertebrae in the treatment of the osteoporotic spine. Spine J. 2017;17(3):328-337. [37] GIRARDO M, CINNELLA P, GARGIULO G, et al. Surgical treatment of osteo-porotic thoraco -lumbar compressive fractures: the use of pediclescrew with augmentation PMMA. Eur Spine J. 2017;26(Suppl 4):546-551. [38] SHI S, ZHOU Z, NI HJ, et al. Does anxiety influence the prognosis of percutaneous transforaminal endoscopic discectomy in the treatment of lumbar disc herniation? A preliminary propensity score matching analysis. Int Orthop. 2020;44(11):2357-2363. [39] WANG Y, YANG L, LI C, et al. The Biomechanical Properties of Cement-Augmented Pedicle Screws for Osteoporotic Spines. Global Spine J. 2022;12(2):323-332. [40] JANSSEN I, RYANG YM, GEMPT J, et al. Risk of cement leakage and pulmonary embolism by bone cement-augmented pedicle screw fixation of the thoracolumbar spine. Spine J. 2017;17(6):837-844. [41] EHRESMAN J, PENNINGTON Z, ELSAMADICY AA, et al. Fenestrated pedicle screws for thoracolumbar instrumentation in patients with poor bone quality: Case series and systematic review of the literature. Clin Neurol Neurosurg. 2021;206:106675. [42] CHEN LH, TAI CL, LEE DM, et al. Pullout strength of pedicle screws with cement augmentation in severe osteoporosis: a comparative study between cannulated screws with cement injection and solid screws with cement pre-filling. BMC Musculoskelet Disord. 2011;12:33. [43] 郭海威,谢家豪,林燕平,等.骨水泥强化空心侧孔与常规椎弓根螺钉内固定修复骨质疏松椎体效果及安全性Meta分析[J].中国组织工程研究,2021,25(30):4891-4899. |
| [1] | Zhong Jun, Wang Wen. Network meta-analysis of different anatomical repair strategies to improve chronic lateral ankle instability [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1470-1476. |
| [2] | Ouyang Beiping, Ma Xiangyang, Luo Chunshan, Zou Xiaobao, Lu Tingsheng, Chen Qiling. Three-dimensional finite element analysis of a new horizontal screw-screw crosslink in posterior atlantoaxial internal fixation [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1320-1324. |
| [3] | Guo Sutong, Feng Dehong, Guo Yu, Wang Ling, Ding Yujian, Liu Yi, Qian Zhengying, Li Mingyang. Construction and finite element analysis of normal and osteoporotic hip models [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1342-1346. |
| [4] | Niu Hegang, Yang Kun, Zhang Jingjing, Yan Yizhu, Zhang Yinshun. Design of a new posterior atlas fracture reduction and internal fixation system [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1399-1402. |
| [5] | Wang Menghan, Qi Han, Zhang Yuan, Chen Yanzhi. Three kinds of 3D printed models assisted in treatment of Robinson type II B2 clavicle fracture [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1403-1408. |
| [6] | Zhang Xiaoyun, Liu Hua, Chai Yuan, Chen Feng, Zeng Hao, Gao Zhengang, Huang Yourong. Effect of Yishen Gushu Formula on bone metabolic markers and clinical efficacyn in patients with osteoporosis of kidney deficiency and blood stasis type [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(8): 1155-1160. |
| [7] | Dai Yuexing, Zheng Liqin, Wu Minhui, Li Zhihong, Li Shaobin, Zheng Desheng, Lin Ziling. Effect of vessel number on computational fluid dynamics in vascular networks [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(8): 1206-1210. |
| [8] | Ma Shuwei, He Sheng, Han Bing, Zhang Liaoyun. Exosomes derived from mesenchymal stem cells in treatment of animals with acute liver failure: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(7): 1137-1142. |
| [9] | Wang Qiang, Li Shiyun, Xiong Ying, Li Tiantian. Biomechanical changes of the cervical spine in internal fixation with different anterior cervical interbody fusion systems [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 821-826. |
| [10] | Zhang Min, Peng Jing, Zhang Qiang, Chen Dewang. Mechanical properties of L3/4 laminar decompression and intervertebral fusion in elderly osteoporosis patients analyzed by finite element method [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 847-851. |
| [11] | Xue Xiaofeng, Wei Yongkang, Qiao Xiaohong, Du Yuyong, Niu Jianjun, Ren Lixin, Yang Huifeng, Zhang Zhimin, Guo Yuan, Chen Weiyi. Finite element analysis of osteoporosis in proximal femur after cannulated screw fixation for femoral neck fracture [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 862-867. |
| [12] | Zheng Jiafa, Song Xiufeng, Li Hongzhi, Zhou Jinming, Guan Shengyi, Yu He. Open reduction and internal fixation via the para-Achilles tendon approach for the treatment of posterior malleolus sandwich fractures [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 934-938. |
| [13] | Kaiyisaier•Abudukelimu, Maimaitimin•Abulimiti, Li Lei, Yang Xiaokai, Zhang Yukun, Liu Shuai. Effect of lumbar CT values in the diagnosis of osteoporosis in women patients with lumbar degenerative diseases [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 945-949. |
| [14] | Wang Liping, Lian Tianxing, Hu Yongrong, Yang Hongsheng, Zeng Zhimou, Liu Hao, Qu Bo. HU value of chest CT vertebral body in the opportunistic screening of type 2 diabetes mellitus osteoporosis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 950-954. |
| [15] | Zhang Zeyi, Yang Yimin, Li Wenyan, Zhang Meizhen. Effect of foot progression angle on lower extremity kinetics of knee osteoarthritis patients of different ages: a systematic review and meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 968-975. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||