Chinese Journal of Tissue Engineering Research ›› 2018, Vol. 22 ›› Issue (13): 2051-2056.doi: 10.3969/j.issn.2095-4344.0504
Previous Articles Next Articles
MicroRNA-520a-3p induces apoptosis in lung cancer stem cells via modulation of MAP3K2
Yan Jun1, Zhong Zhi-hong2, Shi Hua-qiu1
- 1Department of Oncology, First Affiliated Hospital of Gannan Medical University, Ganzhou 341000, Jiangxi Province, China; 2Rural (Community) Medical Education Research Center, Gannan Medical University, Ganzhou 341000, Jiangxi Province, China
-
Revised:2018-03-29Online:2018-05-08Published:2018-05-08 -
Contact:Shi Hua-qiu, Master, Associate chief physician, Associate professor, Department of Oncology, First Affiliated Hospital of Gannan Medical University, Ganzhou 341000, Jiangxi Province, China -
About author:Yan Jun, Master, Attending physician, Lecturer, Department of Oncology, First Affiliated Hospital of Gannan Medical University, Ganzhou 341000, Jiangxi Province, China -
Supported by:the Scientific Plan of Jiangxi Health Department, No. 20143129
CLC Number:
Cite this article
Yan Jun, Zhong Zhi-hong, Shi Hua-qiu. MicroRNA-520a-3p induces apoptosis in lung cancer stem cells via modulation of MAP3K2[J]. Chinese Journal of Tissue Engineering Research, 2018, 22(13): 2051-2056.
share this article
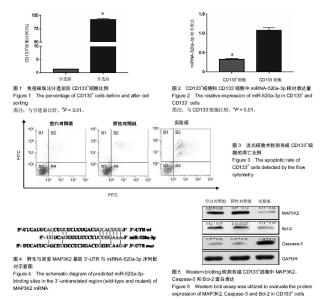
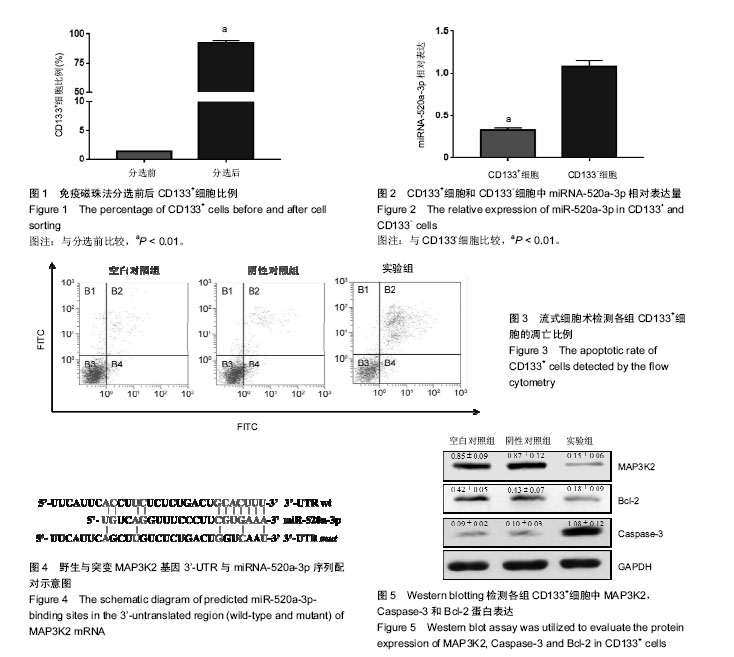
2.1 免疫磁珠细胞分选肺癌干细胞 采用免疫磁珠法在肺腺癌A549细胞系中分离CD133+肺癌干细胞,流式细胞仪检测分选前后CD133+细胞比例。分选后CD133+细胞比例显著高于分选前,差异有显著性意义(t=-45.706,P=0.000),见图1。 2.2 miRNA-520a-3p在CD133+肺癌干细胞中的表达 采用real-time PCR技术检测CD133+细胞中miRNA-520a-3p表达,以CD133-细胞为对照。结果显示,CD133+细胞中miRNA-520a-3p相对表达量显著低于CD133-细胞,差异有显著性意义(t=-9.636,P=0.000),见图2。 2.3 miRNA-520a-3p促进CD133+肺癌干细胞凋亡 转染miRNA-520a-3p mimics至CD133+细胞中48 h后,流式细胞术检测结果显示,实验组细胞的凋亡比例(52.32±4.83)%显著高于空白对照组(18.32±2.84)%和阴性对照组(19.12± 2.99)%,差异均有显著性意义(t=10.510,P=0.000;t=10.123,P=0.000),而空白对照组和阴性对照组之间差异无显著性意义(t=-0.336,P=0.377),见图3。 2.4 MiRNA-520a-3p靶向调节MAP3K2基因表达 HEK-293T细胞中,miRNA-520a-3p mimics+pmirGLO- MAP3K2-3’-UTR wt组的相对荧光强度(0.42±0.08)显著低于miRNA-520a-3p mimics+pmirGLO空载体对照组(1.04±0.13)和miRNA-520a-3p mimics+pmirGLO- MAP3K2-3’-UTR mut组(0.99±0.15),差异均有显著性意义(t=-7.035,P=0.001;t=-5.807,P=0.002),而miRNA-520a- 3p mimics+pmirGLO空载体对照组和miRNA-520a-3p mimics+pmirGLO-MAP3K2-3’-UTR mut组之间差异无显著性意义(t=0.436,P=0.343),见图4。 2.5 miRNA-520a-3p对MAP3K2蛋白及凋亡相关蛋白Bcl-2和Caspase-3表达的影响 Western Blotting检测结果显示,与空白对照组和阴性对照组相比,实验组细胞中的MAP3K2蛋白水平显著降低,差异有显著性意义(t=11.209,P=0.000;t=11.529,P=0.000),空白对照组和阴性对照组之间差异无显著性意义(t=-0.231,P=0.414),见图5;与空白对照组和阴性对照组相比,实验组细胞中的Bcl-2蛋白水平均显著降低,差异有显著性意义(t=4.038,P=0.008;t=3.798,P=0.010),空白对照组和阴性对照组之间差异无显著性意义(t=0.201,P=0.425),见图5;实验组细胞中的Caspase-3蛋白水平(1.08±0.12)显著高于空白对照组(0.09±0.02)和阴性对照组(0.10±0.03),差异有显著性意义(t=14.095,P=0.000;t=13.723,P=0.000),空白对照组和阴性对照组之间差异无显著性意义(t=-0.480,P=0.328),见图5。"
| [1] Sagawa M, Sugawara T, Ishibashi N, et al. Efficacy of low-dose computed tomography screening for lung cancer: the current state of evidence of mortality reduction. Surg Today. 2017;47(7):783-788.[2] Torre LA, Bray F, Siegel RL, et al. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65(2):87-108.[3] Patz EF Jr, Greco E, Gatsonis C, et al. Lung cancer incidence and mortality in National Lung Screening Trial participants who underwent low-dose CT prevalence screening: a retrospective cohort analysis of a randomised, multicentre, diagnostic screening trial. Lancet Oncol. 2016;17(5):590-599. [4] Chen W, Liu X, Yuan S, et al. HSPA12B overexpression induces cisplatin resistance in non-small-cell lung cancer by regulating the PI3K/Akt/NF-κB signaling pathway. Oncol Lett. 2018;15(3):3883-3889.[5] Hochmair MJ, Schwab S, Prosch H. Complete remission of intrathecal metastases with lorlatinib therapy in a heavily pretreated ALK-positive lung cancer patient. Anticancer Drugs. 2017;28(8):928-930.[6] Liu K, Zheng D, Xu G, et al. Local thoracic therapy improve prognosis for stage IV non-small cell lung cancer patients combined with chemotherapy: A Surveillance, Epidemiology, and End Results database analysis. PLoS One. 2017;12(11): e0187350.[7] Lo PK, Wolfson B, Zhou Q. Cancer stem cells and early stage basal-like breast cancer. World J Obstet Gynecol. 2016;5(2): 150-161. [8] Polyak K, Haviv I, Campbell IG. Co-evolution of tumor cells and their microenvironment. Trends Genet. 2009;25(1):30-38.[9] Batlle E, Clevers H. Cancer stem cells revisited. Nat Med. 2017;23(10):1124-1134. [10] Zhang L, Guo X, Zhang L, et al. SLC34A2 regulates miR-25-Gsk3β signaling pathway to affect tumor progression in gastric cancer stem cell-like cells. Mol Carcinog. 2018; 57(3):440-450.[11] Sun Y, Yoshida T, Okabe M, et al. Isolation of Stem-Like Cancer Cells in Primary Endometrial Cancer Using Cell Surface Markers CD133 and CXCR4. Transl Oncol. 2017; 10(6):976-987.[12] Zhang CL, Huang T, Wu BL, et al. Stem cells in cancer therapy: opportunities and challenges. Oncotarget. 2017; 8(43):75756-75766.[13] Chatterjee N, Rana S, Espinosa-Diez C, et al. MicroRNAs in Cancer: challenges and opportunities in early detection, disease monitoring, and therapeutic agents. Curr Pathobiol Rep. 2017;5(1):35-42.[14] Petrovic N, Ergün S, Isenovic ER. Levels of MicroRNA Heterogeneity in Cancer Biology. Mol Diagn Ther. 2017;21(5): 511-523.[15] Zhang C, Song G, Ye W, et al. MicroRNA-302a inhibits osteosarcoma cell migration and invasion by directly targeting IGF-1R. Oncol Lett. 2018;15(4):5577-5583.[16] Yu X, Ma C, Fu L, et al. MicroRNA-139 inhibits the proliferation, migration and invasion of gastric cancer cells by directly targeting ρ-associated protein kinase 1. Oncol Lett. 2018;15(4):5977-5982.[17] Tao ZQ, Shi AM, Li R, et al. Role of microRNA in prostate cancer stem/progenitor cells regulation. Eur Rev Med Pharmacol Sci. 2016;20(14):3040-3044.[18] Huang Y, Davidson NE. Targeting tumorigenicity of breast cancer stem-like cells using combination epigenetic therapy: something old and something new. J Thorac Dis. 2016;8(11): 2971-2974. [19] Moreb JS, Ucar-Bilyeu DA, Khan A. Use of retinoic acid/aldehyde dehydrogenase pathway as potential targeted therapy against cancer stem cells. Cancer Chemother Pharmacol. 2017;79(2):295-301.[20] Lin X, Chen W, Wei F, et al. Nanoparticle Delivery of miR-34a Eradicates Long-term-cultured Breast Cancer Stem Cells via Targeting C22ORF28 Directly. Theranostics. 2017;7(19): 4805-4824.[21] Wang J, Wu Y, Gao W, et al. Identification and characterization of CD133+CD44+ cancer stem cells from human laryngeal squamous cell carcinoma cell lines. J Cancer. 2017;8(3):497-506.[22] Crous AM, Abrahamse H. Lung cancer stem cells and low-intensity laser irradiation: a potential future therapy. Stem Cell Res Ther. 2013;4(5):129.[23] Mei D, Lv B, Chen B, et al. All-trans retinoic acid suppresses malignant characteristics of CD133-positive thyroid cancer stem cells and induces apoptosis. PLoS One. 2017;12(8): e0182835.[24] Sun Y, Yoshida T, Okabe M, et al. Isolation of Stem-Like Cancer Cells in Primary Endometrial Cancer Using Cell Surface Markers CD133 and CXCR4. Transl Oncol. 2017; 10(6):976-987.[25] Eramo A, Lotti F, Sette G, et al. Identification and expansion of the tumorigenic lung cancer stem cell population. Cell Death Differ. 2008;15(3):504-514.[26] Ho MM, Ng AV, Lam S, et al. Side population in human lung cancer cell lines and tumors is enriched with stem-like cancer cells. Cancer Res. 2007;67(10):4827-4833.[27] Wu N, Song Y, Pang L, et al. CRCT1 regulated by microRNA-520 g inhibits proliferation and induces apoptosis in esophageal squamous cell cancer. Tumour Biol. 2016; 37(6):8271-8279.[28] Keklikoglou I, Koerner C, Schmidt C, et al. MicroRNA-520/373 family functions as a tumor suppressor in estrogen receptor negative breast cancer by targeting NF-κB and TGF-β signaling pathways. Oncogene. 2012;31(37):4150-4163.[29] Liu Y, Miao L, Ni R, et al. microRNA-520a-3p inhibits proliferation and cancer stem cell phenotype by targeting HOXD8 in non-small cell lung cancer. Oncol Rep. 2016;36(6): 3529-3535.[30] Esser JS, Saretzki E, Pankratz F, et al. Bone morphogenetic protein 4 regulates microRNAs miR-494 and miR-126-5p in control of endothelial cell function in angiogenesis. Thromb Haemost. 2017;117(4):734-749.[31] Zhu Y, Peng Q, Lin Y, et al. Identification of biomarker microRNAs for predicting the response of colorectal cancer to neoadjuvant chemoradiotherapy based on microRNA regulatory network. Oncotarget. 2017;8(2):2233-2248.[32] Zhang R, Liu R, Liu C, et al. A Novel Role for MiR-520a-3p in Regulating EGFR Expression in Colorectal Cancer. Cell Physiol Biochem. 2017;42(4):1559-1574. [33] Li J, Wei J, Mei Z, et al. Suppressing role of miR-520a-3p in breast cancer through CCND1 and CD44. Am J Transl Res. 2017;9(1):146-154.[34] Huang T, She K, Peng G, et al. MicroRNA-186 suppresses cell proliferation and metastasis through targeting MAP3K2 in non-small cell lung cancer. Int J Oncol. 2016;49(4): 1437-1444. [35] Wu J, Li WZ, Huang ML, et al. Regulation of cancerous progression and epithelial-mesenchymal transition by miR-34c-3p via modulation of MAP3K2 signaling in triple-negative breast cancer cells. Biochem Biophys Res Commun. 2017;483(1):10-16.[36] Qiu J, Thorley-Lawson DA. EBV microRNA BART 18-5p targets MAP3K2 to facilitate persistence in vivo by inhibiting viral replication in B cells. Proc Natl Acad Sci U S A. 2014; 111(30):11157-11162.[37] Zhang X, Song H, Qiao S, et al. MiR-17-5p and miR-20a promote chicken cell proliferation at least in part by upregulation of c-Myc via MAP3K2 targeting. Sci Rep. 2017; 7(1):15852. [38] Mazur PK, Reynoird N, Khatri P, et al. SMYD3 links lysine methylation of MAP3K2 to Ras-driven cancer. Nature. 2014; 510(7504):283-287. |
| [1] | Zhang Tongtong, Wang Zhonghua, Wen Jie, Song Yuxin, Liu Lin. Application of three-dimensional printing model in surgical resection and reconstruction of cervical tumor [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1335-1339. |
| [2] | Geng Qiudong, Ge Haiya, Wang Heming, Li Nan. Role and mechanism of Guilu Erxianjiao in treatment of osteoarthritis based on network pharmacology [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1229-1236. |
| [3] | Pei Lili, Sun Guicai, Wang Di. Salvianolic acid B inhibits oxidative damage of bone marrow mesenchymal stem cells and promotes differentiation into cardiomyocytes [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1032-1036. |
| [4] | Zeng Yanhua, Hao Yanlei. In vitro culture and purification of Schwann cells: a systematic review [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1135-1141. |
| [5] | Li Shibin, Lai Yu, Zhou Yi, Liao Jianzhao, Zhang Xiaoyun, Zhang Xuan. Pathogenesis of hormonal osteonecrosis of the femoral head and the target effect of related signaling pathways [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 935-941. |
| [6] | Xu Yinqin, Shi Hongmei, Wang Guangyi. Effects of Tongbi prescription hot compress combined with acupuncture on mRNA expressions of apoptosis-related genes,Caspase-3 and Bcl-2, in degenerative intervertebral discs [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 713-718. |
| [7] | Zhang Wenwen, Jin Songfeng, Zhao Guoliang, Gong Lihong. Mechanism by which Wenban Decoction reduces homocysteine-induced apoptosis of myocardial microvascular endothelial cells in rats [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 723-728. |
| [8] | Liu Qing, Wan Bijiang. Effect of acupotomy therapy on the expression of Bcl-2/Bax in synovial tissue of collagen-induced arthritis rats [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 729-734. |
| [9] | Xie Chongxin, Zhang Lei. Comparison of knee degeneration after anterior cruciate ligament reconstruction with or without remnant preservation [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 735-740. |
| [10] | Xu Dongzi, Zhang Ting, Ouyang Zhaolian. The global competitive situation of cardiac tissue engineering based on patent analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 807-812. |
| [11] | Wu Zijian, Hu Zhaoduan, Xie Youqiong, Wang Feng, Li Jia, Li Bocun, Cai Guowei, Peng Rui. Three-dimensional printing technology and bone tissue engineering research: literature metrology and visual analysis of research hotspots [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 564-569. |
| [12] | Chang Wenliao, Zhao Jie, Sun Xiaoliang, Wang Kun, Wu Guofeng, Zhou Jian, Li Shuxiang, Sun Han. Material selection, theoretical design and biomimetic function of artificial periosteum [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 600-606. |
| [13] | Liu Fei, Cui Yutao, Liu He. Advantages and problems of local antibiotic delivery system in the treatment of osteomyelitis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 614-620. |
| [14] | Li Xiaozhuang, Duan Hao, Wang Weizhou, Tang Zhihong, Wang Yanghao, He Fei. Application of bone tissue engineering materials in the treatment of bone defect diseases in vivo [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 626-631. |
| [15] | Zhang Zhenkun, Li Zhe, Li Ya, Wang Yingying, Wang Yaping, Zhou Xinkui, Ma Shanshan, Guan Fangxia. Application of alginate based hydrogels/dressings in wound healing: sustained, dynamic and sequential release [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 638-643. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||