Chinese Journal of Tissue Engineering Research ›› 2019, Vol. 23 ›› Issue (33): 5322-5327.doi: 10.3969/j.issn.2095-4344.1825
Previous Articles Next Articles
Human induced pluripotent stem cell transplantation for hypoxic-ischemic encephalopathy in neonatal mice
Gong Jiao, Liu Ming
- Department of Pediatric Surgery, Affiliated Hospital of Southwest Medical University, Luzhou 646000, Sichuan Province, China
-
Revised:2019-05-13Online:2019-11-28Published:2019-11-28 -
Contact:Liu Ming, Master, Department of Pediatric Surgery, Affiliated Hospital of Southwest Medical University, Luzhou 646000, Sichuan Province, China -
About author:Gong Jiao, Master, Department of Pediatric Surgery, Affiliated Hospital of Southwest Medical University, Luzhou 646000, Sichuan Province, China
CLC Number:
Cite this article
Gong Jiao, Liu Ming. Human induced pluripotent stem cell transplantation for hypoxic-ischemic encephalopathy in neonatal mice[J]. Chinese Journal of Tissue Engineering Research, 2019, 23(33): 5322-5327.
share this article

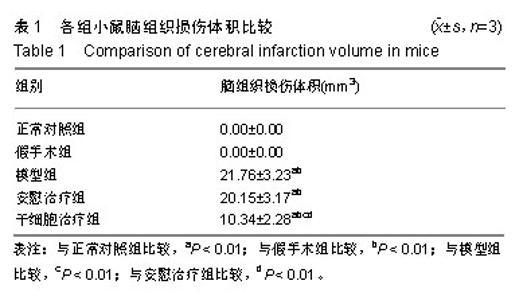
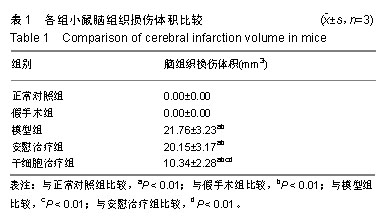
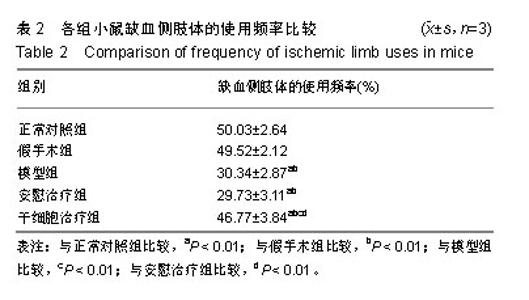
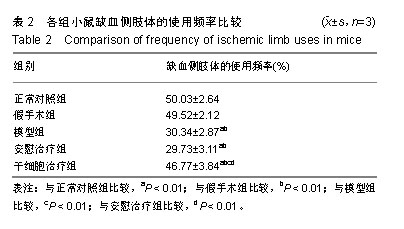
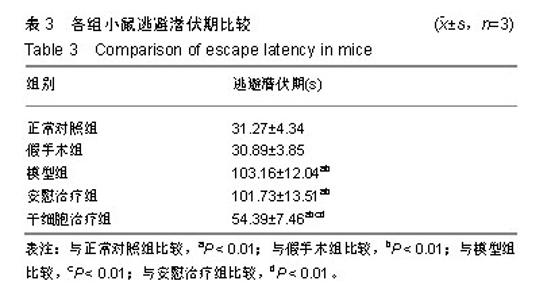
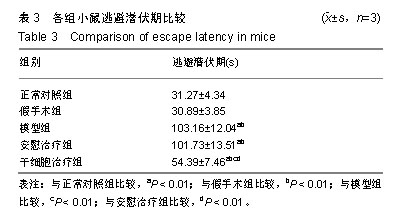
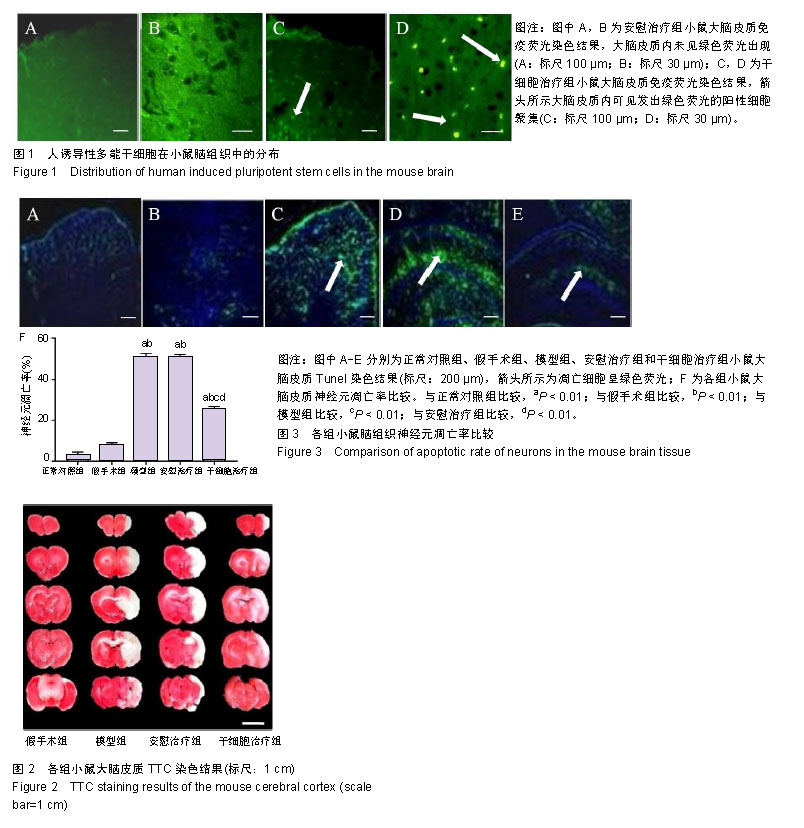
2.1 实验动物数量分析 参加实验的小鼠共60只,实验过程顺利,无死亡动物,60只小鼠的实验数据均进入结果分析。 2.2 人诱导性多能干细胞在小鼠脑组织中的分布 绿色荧光标记的人诱导性多能干细胞散在分布于患侧大脑皮质,颞叶皮质部位较多,提示移植14 d时人诱导性多能干细胞仍在脑组织内存活并移行,见图1。 2.3 各组小鼠大脑损伤体积比较 TTC染色结果显示,假手术组小鼠大脑皮质无苍白区,模型组、安慰治疗组和干细胞治疗组小鼠大脑皮质内可见苍白区,见图2。治疗14 d后,干细胞治疗组小鼠脑组织损伤体积小于模型组和安慰治疗组(P < 0.01),见表1。 2.4 各组小鼠脑组织神经元凋亡率比较 Tunel染色结果显示,正常对照组和假手术组小鼠脑组织内偶见散在分布的凋亡神经元,模型组和安慰治疗组小鼠脑组织内凋亡的神经元较多,见图3A-E,干细胞治疗组小鼠脑组织内神经元凋亡率低于模型组和安慰治疗组(P < 0.01),模型组和安慰治疗组小鼠脑组织内神经元凋亡率高于正常对照组和假手术组(P < 0.01),见图3F。"
| [1]Lemyre B, Chau V. Hypothermia for newborns with hypoxic-ischemic encephalopathy. Paediatr Child Health. 2018;23(4):285-291.[2]Mendler MR, Mendler I, Hassan MA, et al. Predictive Value of Thompson-Score for Long-Term Neurological and Cognitive Outcome in Term Newborns with Perinatal Asphyxia and Hypoxic-Ischemic Encephalopathy Undergoing Controlled Hypothermia Treatment. Neonatology. 2018;114(4):341-347.[3]Chevin M, Guiraut C, Sébire G. Effect of hypothermia on interleukin-1 receptor antagonist pharmacodynamics in inflammatory-sensitized hypoxic-ischemic encephalopathy of term newborns. J Neuroinflammation. 2018;15(1):214.[4]Kushwah S, Kumar A, Verma A, et al. Comparison of fractional anisotropy and apparent diffusion coefficient among hypoxic ischemic encephalopathy stages 1, 2, and 3 and with nonasphyxiated newborns in 18 areas of brain. Indian J Radiol Imaging. 2017;27(4):447-456.[5]Sánchez-Illana Á, Núñez-Ramiro A, Cernada M, et al. Evolution of Energy Related Metabolites in Plasma from Newborns with Hypoxic-Ischemic Encephalopathy during Hypothermia Treatment. Sci Rep. 2017;7(1):17039.[6]Xie B, Gu P, Wang W, et al. Therapeutic effects of human umbilical cord mesenchymal stem cells transplantation on hypoxic ischemic encephalopathy. Am J Transl Res. 2016;8(7):3241-3250.[7]Ji G, Liu M, Zhao XF, et al. NF-κB Signaling is Involved in the Effects of Intranasally Engrafted Human Neural Stem Cells on Neurofunctional Improvements in Neonatal Rat Hypoxic-Ischemic Encephalopathy. CNS Neurosci Ther. 2015;21(12):926-935.[8]Simiyu IN, Mchaile DN, Katsongeri K, et al. Prevalence, severity and early outcomes of hypoxic ischemic encephalopathy among newborns at a tertiary hospital, in northern Tanzania. BMC Pediatr. 2017;17(1):131.[9]Ma J, Wang Y, Yang J, et al. Treatment of hypoxic-ischemic encephalopathy in mouse by transplantation of embryonic stem cell-derived cells. Neurochem Int. 2007;51(1):57-65.[10]Ji G, Liu M, Zhao XF, et al. NF-κB Signaling is Involved in the Effects of Intranasally Engrafted Human Neural Stem Cells on Neurofunctional Improvements in Neonatal Rat Hypoxic-Ischemic Encephalopathy. CNS Neurosci Ther. 2015;21(12):926-935.[11]Park D, Lee SH, Bae DK, et al. Transplantation of Human Adipose Tissue-Derived Mesenchymal Stem Cells Restores the Neurobehavioral Disorders of Rats With Neonatal Hypoxic-Ischemic Encephalopathy. Cell Med. 2013;5(1):17-28.[12]Park WS, Sung SI, Ahn SY, et al. Hypothermia augments neuroprotective activity of mesenchymal stem cells for neonatal hypoxic-ischemic encephalopathy. PLoS One. 2015;10(3):e0120893.[13]Zhang X, Zhang Q, Li W, et al. Therapeutic effect of human umbilical cord mesenchymal stem cells on neonatal rat hypoxic-ischemic encephalopathy. J Neurosci Res. 2014;92(1):35-45.[14]Xie B, Gu P, Wang W, et al. Therapeutic effects of human umbilical cord mesenchymal stem cells transplantation on hypoxic ischemic encephalopathy. Am J Transl Res. 2016;8(7):3241-3250.[15]肖升平,马廉,罗敏洁,等.人脐带血间充质干细胞在缺氧缺血性脑病新生鼠脑内的定植[J].实用儿科临床杂志,2007,15(21):1655-1657.[16]李禄全,余加林,官晓清,等.鼠骨髓间充质干细胞在缺氧缺血性脑病新生鼠脑内的分布及分化[J].第三军医大学学报,2005,36(4): 327-330.[17]彭雅南,赵振强.人诱导性多能干细胞源神经元移植治疗帕金森病的现状与未来[J].中国组织工程研究,2016,20(36): 5458-5465.[18]陈旭东,范文娟,袁科理,等.不同培养条件对小鼠诱导性多能干细胞分化为神经元样细胞的影响[J].细胞与分子免疫学杂志, 2015,31(9):1216-1219, 1223.[19]林良烽.虾青素对缺氧缺血性脑损伤新生大鼠模型的神经保护作用[J].中国组织工程研究,2015,19(40):6480-6484.[20]罗梦娇,王贝,郭瑞,等. Olig2对胚胎干细胞向神经前体细胞分化过程中Nestin蛋白表达的影响[J].神经解剖学杂志, 2015, 31(1):91-94.[21]周永新,刘俊,李海英,等.缺氧缺血性脑病新生大鼠海马EphA5受体mRNA表达与神经元凋亡的关系[J].南京医科大学学报(自然科学版),2013, 33(11):1521-1523,1528.[22]朱江.头部亚低温联合鼠神经生长因子治疗新生儿缺氧缺血性脑病的疗效观察[J].现代诊断与治疗,2017,25(12):9-10.[23]袁金晶,李冰,吴德,等.低氧诱导因子-1α基因C1772T/G1790A多态性与HIE及HIE致脑性瘫痪的关系[J].中华实用儿科临床杂志, 2010, 25(19): 1500-1502.[24]王爱,牟青杰,王晓莉,等.牙髓干细胞移植治疗缺氧缺血性脑损伤新生大鼠远期行为学及环磷酸腺苷反应元件结合蛋白的变化[J].中国组织工程研究,2017,21(5): 701-706.[25]Kidani Y, Miki Y, Nomimura N, et al. The therapeutic effect of CD133(+) cells derived from human umbilical cord blood on neonatal mouse hypoxic-ischemic encephalopathy model. Life Sci. 2016;157:108-115.[26]楚冬梅,高心静,温丙友,等.干细胞治疗新生儿缺氧缺血性脑病的研究进展[J].医学综述,2018,24(18):3649-3657.[27]Chaparro-Huerta V, Flores-Soto ME, Merin Sigala ME, et al. Proinflammatory Cytokines, Enolase and S-100 as Early Biochemical Indicators of Hypoxic-Ischemic Encephalopathy Following Perinatal Asphyxia in Newborns. Pediatr Neonatol. 2017;58(1):70-76..[28]Ohshima M, Taguchi A, Sato Y, et al. Evaluations of Intravenous Administration of CD34+ Human Umbilical Cord Blood Cells in a Mouse Model of Neonatal Hypoxic-Ischemic Encephalopathy. Dev Neurosci. 2016;38(5):331-341.[29]Fang C, Xie L, Liu C, et al. Tanshinone IIA improves hypoxic ischemic encephalopathy through TLR?4?mediated NF?κB signal pathway. Mol Med Rep. 2018;18(2):1899-1908.[30]Ten VS, Bradley-Moore M, Gingrich JA, et al. Brain injury and neurofunctional deficit in neonatal mice with hypoxic-ischemic encephalopathy. Behav Brain Res. 2003;145(1-2):209-219.[31]Lv HY, Wu SJ, Wang QL, et al.Effect of erythropoietin combined with hypothermia on serum tau protein levels and neurodevelopmental outcome in neonates with hypoxic-ischemic encephalopathy.Neural Regen Res. 2017;12(10):1655-1663.[32]Reinboth BS, Köster C, Abberger H, et al. Endogenous hypothermic response to hypoxia reduces brain injury: Implications for modeling hypoxic-ischemic encephalopathy and therapeutic hypothermia in neonatal mice. Exp Neurol. 2016;283(Pt A):264-275.[33]Zaitoun IS, Cikla U, Zafer D, et al. Attenuation of Retinal Vascular Development in Neonatal Mice Subjected to Hypoxic-Ischemic Encephalopathy. Sci Rep. 2018;8(1):9166.[34]Moon CJ, Youn YA, Yum SK, et al. Cytokine changes in newborns with therapeutic hypothermia after hypoxic ischemic encephalopathy. J Perinatol. 2016;36(12):1092-1096.[35]Elshorbagy HH, Azab AA, Kamal NM, et al. Value of electroencephalographic monitoring in newborns with hypoxic- ischemic encephalopathy treated with hypothermia. J Pediatr Neurosci. 2016;11(4):309-315.[36]Chalak LF, Zhang R. New Wavelet Neurovascular Bundle for Bedside Evaluation of Cerebral Autoregulation and Neurovascular Coupling in Newborns with Hypoxic-Ischemic Encephalopathy. Dev Neurosci. 2017;39(1-4):89-96.[37]Metzler M, Govindan R, Al-Shargabi T, et al. Pattern of brain injury and depressed heart rate variability in newborns with hypoxic ischemic encephalopathy. Pediatr Res. 2017;82(3):438-443. |
| [1] | Geng Qiudong, Ge Haiya, Wang Heming, Li Nan. Role and mechanism of Guilu Erxianjiao in treatment of osteoarthritis based on network pharmacology [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1229-1236. |
| [2] | Yuan Mei, Zhang Xinxin, Guo Yisha, Bi Xia. Diagnostic potential of circulating microRNA in vascular cognitive impairment [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1299-1304. |
| [3] | Zhu Xuefen, Huang Cheng, Ding Jian, Dai Yongping, Liu Yuanbing, Le Lixiang, Wang Liangliang, Yang Jiandong. Mechanism of bone marrow mesenchymal stem cells differentiation into functional neurons induced by glial cell line derived neurotrophic factor [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1019-1025. |
| [4] | Pei Lili, Sun Guicai, Wang Di. Salvianolic acid B inhibits oxidative damage of bone marrow mesenchymal stem cells and promotes differentiation into cardiomyocytes [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1032-1036. |
| [5] | Wang Feng, Zhou Liyu, Saijilafu, Qi Shibin, Ma Yanxia, Wei Shanwen. CaMKII-Smad1 promotes axonal regeneration of peripheral nerves [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1064-1068. |
| [6] | Li Shibin, Lai Yu, Zhou Yi, Liao Jianzhao, Zhang Xiaoyun, Zhang Xuan. Pathogenesis of hormonal osteonecrosis of the femoral head and the target effect of related signaling pathways [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 935-941. |
| [7] | Xu Yinqin, Shi Hongmei, Wang Guangyi. Effects of Tongbi prescription hot compress combined with acupuncture on mRNA expressions of apoptosis-related genes,Caspase-3 and Bcl-2, in degenerative intervertebral discs [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 713-718. |
| [8] | Zhang Wenwen, Jin Songfeng, Zhao Guoliang, Gong Lihong. Mechanism by which Wenban Decoction reduces homocysteine-induced apoptosis of myocardial microvascular endothelial cells in rats [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 723-728. |
| [9] | Liu Qing, Wan Bijiang. Effect of acupotomy therapy on the expression of Bcl-2/Bax in synovial tissue of collagen-induced arthritis rats [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 729-734. |
| [10] | Xie Chongxin, Zhang Lei. Comparison of knee degeneration after anterior cruciate ligament reconstruction with or without remnant preservation [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 735-740. |
| [11] | Su Liping, Lu Ziyang, Liu Li, Zhang Wei, Su Tianyuan, Hu Xiayun, Pu Hongwei, Han Dengfeng. C-jun, Cytc and Caspase-9 in the apoptosis of cerebellar granule neurons induced by diacetylmorphine in rats [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(25): 3943-3948. |
| [12] | Zuo Zhenkui, Han Jiarui, Ji Shuling, He Lulu. Pretreatment with ginkgo biloba extract 50 alleviates radiation-induced acute intestinal injury in mice [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(23): 3666-3671. |
| [13] | Zhang Liang, Ma Xiaoyan, Wang Jiahong. Regulatory mechanism of Shenshuai Yin on cell apoptosis in the kidney of chronic renal failure rats [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(23): 3672-3677. |
| [14] | Xie Yang, Lü Zhiyu, Zhang Shujiang, Long Ting, Li Zuoxiao. Effects of recombinant adeno-associated virus mediated nerve growth factor gene transfection on oligodendrocyte apoptosis and myelination in experimental autoimmune encephalomyelitis mice [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(23): 3678-3683. |
| [15] | Xu Bin, Yang Xiushu, Liu Xuan, Wang Zhenxing. Changes of intestinal epithelial cells and their apoptotic factors Caspase-3, Bax and Bcl-2 under urinary environment [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(20): 3173-3177. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||