Chinese Journal of Tissue Engineering Research ›› 2022, Vol. 26 ›› Issue (32): 5229-5235.doi: 10.12307/2022.897
Previous Articles Next Articles
Growth and development characteristics of dental and basal arch in children with skeletal class III malocclusion
Gao Liping1, Tang Li1, Wan Lu1, Liu Yan1, Li Xiaobing2, Zhong Wenyi1
- 1Department of Prevention and Pediatric Dentistry, the Affiliated Stomatological Hospital of Zunyi Medical University, Zunyi 563000, Guizhou Province, China; 2State Key Laboratory of Oral Diseases & National Clinical Research Center for Oral Diseases & Department of Pediatric Dentistry, West China Hospital of Stomatology, Chengdu 610041, Sichuan Province, China
-
Received:2021-12-08Accepted:2022-01-22Online:2022-11-18Published:2022-05-14 -
Contact:Zhong Wenyi, Master, Professor, Department of Prevention and Pediatric Dentistry, the Affiliated Stomatological Hospital of Zunyi Medical University, Zunyi 563000, Guizhou Province, China -
About author:Gao Liping, Master candidate, Department of Prevention and Pediatric Dentistry, the Affiliated Stomatological Hospital of Zunyi Medical University, Zunyi 563000, Guizhou Province, China -
Supported by:China Oral Health Foundation for “Smile Teenagers” Scientific Research Project, No. A2021-093 (to ZWY); Science Foundation Project of Guizhou Provincial Health Commission in 2021, No. gzwkj2021-345 (to ZWY); the Joint Scientific Research and Development Project of Zunyi Municipal Science and Technology Department in 2020, No. (2020)295 (to ZWY); the Science & Technology Plan Projects of Sichuan Province, Nos. 2018ZDYF980 and 2018FZ0099 (to LJQ and LXB)
CLC Number:
Cite this article
Gao Liping, Tang Li, Wan Lu, Liu Yan, Li Xiaobing, Zhong Wenyi. Growth and development characteristics of dental and basal arch in children with skeletal class III malocclusion[J]. Chinese Journal of Tissue Engineering Research, 2022, 26(32): 5229-5235.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
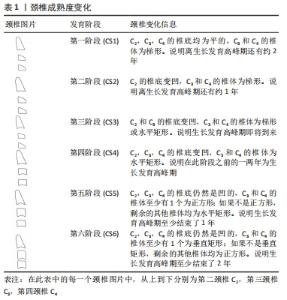
2.1 牙弓和基骨弓的概念 人的牙齿按照一定的顺序、方向和位置排列形成的弓形即为牙弓,位于牙槽骨与颌骨交界处根尖位置形成的弓形即为基骨弓。在研究过程中,由于测量方法、设备和测量标准的不同,对标志点的选取各有不同,但在ANDREWS等[2]出“正常牙牙合六项标准”经典理论后,大多数学者运用临床冠中心的最凸点(FA点)和附着龈与牙槽黏膜交界的软组织带上最凸点(WALA嵴)分别表示牙弓和基骨弓[3]。良好的牙弓形态是维持正畸治疗效果的重要因素,发育异常的牙弓可能会引起对颌牙弓的相应异常,若在正畸的过程中未能解除上、下牙弓的不协调,即使在进入保持阶段,仍有较大的可能性会复发。因此,上、下牙弓形态协调是建立良好咬合的基础。同样,基骨弓在维持正畸治疗的远期效果中发挥重要作用,基骨是正畸牙移动的界限,若超出基骨边界容易引发骨开窗或骨开裂,导致术后唇、颊侧骨板吸收和牙龈退缩,远期的稳定性下降。 2.2 影响牙弓和基骨弓生长发育的因素 牙弓和基骨弓的生长和发育是一个连续而复杂的生物学过程,受遗传和环境等多种因素的相互影响。 2.2.1 遗传因素 通常认为骨性Ⅲ类错牙合畸形大都具有家族遗传史。LAINE等[4]通过研究Y染色体异常的男孩(47,XYY)发现,多余的Y染色体能够促使上颌骨水平向、矢状向以及下颌骨矢状向的过度生长,从而导致畸形。李九军等[5]通过研究发现遗传因素决定上、下颌牙弓形态,尤其对上颌牙弓影响显著,这也在一定程度上证明了骨性Ⅲ类错牙合的遗传特点。 2.2.2 年龄和性别因素 在生长发育过程中,儿童牙弓和基骨弓的大小协调性基本一致,与年龄保持着相同的增长趋势,直到12岁,牙弓宽度生长基本完成,在青春发育高峰期后(14-15岁),牙弓前段长度的生长基本完成,青春发育期后(约18岁),牙弓后段长度基本完成,由于上颌结节的生长潜力,上牙弓后段仍有继续生长的潜能,其宽度也相应增加,即牙弓后段的生长较前段停止得更晚一些[6]。一般情况下,男性牙弓与基骨弓较女性大[7],如意大利男性牙弓长度较女性长,而宽度较女性短,沙特阿拉伯人男性的尖牙和磨牙间牙弓宽度较女性宽[8-9]。 2.2.3 种族、地域和民族因素 不同种族、地域及民族之间,其牙弓形态各不相同。研究表明,相同人种、不同地域的人群,牙弓的形态特点各不相同:日本人的下牙弓比高加索人宽,而韩国人的牙弓较北美人的宽[10-11]。黑人牙弓长度较白人长、宽度较白人大,中国南部地区人群的牙弓宽度要明显大于白色人种[12-13]。相同种族,不同民族人群之间牙弓形态也不尽相同,汉族人群的牙弓宽度以及中后段牙弓长度均大于维吾尔族[14]。 2.2.4 饮食习惯和口周肌肉因素 现代饮食结构向软性食物的转变后,导致咀嚼运动的减弱,从而导致牙弓宽度减小[15]。此外,母乳喂养时间不足、口腔呼吸、耳鼻咽喉部问题均可导致牙弓宽度发育不足[16],但经过预防及干预后,上、下牙弓宽度均明显增加[17]。 口周肌群肌一定程度上也能影响牙弓形态。有研究表明,女性上颌牙弓宽度与咬肌的肌力大小呈正相关,短面型者由于肌力大、咬合紧,牙弓宽度较大[18]。 2.3 儿童骨性Ⅲ类错牙合颌骨生长发育特点 儿童颌骨的生长发育对颅颌面部形态的协调及日后咬牙合的建立具有重要意义,颌骨、牙弓、基骨弓作为一个整体,其生长发育相互影响,具有协同性。骨性Ⅲ类错牙合患儿的上、下颌骨生长速率与年龄和骨龄相关,其增长变化具有相同的趋势。研究表明,以年龄作为纵向观察点,骨性Ⅲ类患儿颌骨长度的增长在不同生长高峰期的速率不尽相同,一直到患儿成年,上颌骨平均每年的增长速率(< 1 mm/年)均小于下颌骨(3.0-4.5 mm/年)[19]。与正常牙合相比,骨性Ⅲ类错牙合下颌骨的增长量是正常牙合的两三倍,尤其是在生长发育的后期(第二、三磨牙萌出时),下颌骨的矢状向生长量远远大于正常 牙合,也就是说,骨性Ⅲ类患儿下颌骨的增长速率及生长量均较大,这也就是导致骨性Ⅲ类下颌发育过度的原因,因此,正确预测生长发育高峰期,抑制其下颌骨的生长发育就显得尤为重要。从骨龄的角度讲,使用颈椎成熟的方法预测生长迸发期是可靠的,BACCETTI等[20]提出运用第二到第四颈椎的发育阶段来评估生长发育高峰的方法,该方法将颈椎的变化分为了6个阶段,见表1。"
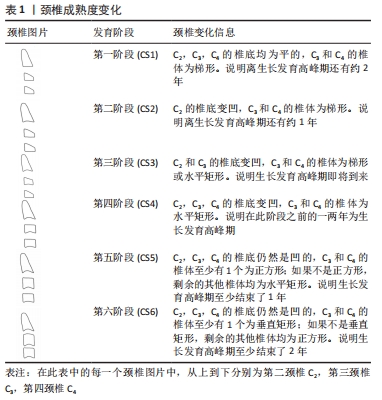
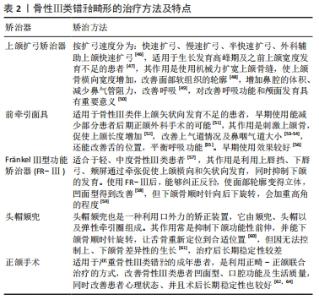
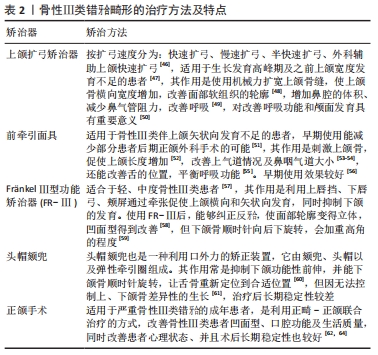
通过上述图表观察颈椎的变化可以发现生长发育高峰期处于第三、四阶段之间,有研究表明下颌骨在CS3和CS4之间增长变化量最大,如若此时不加予干预,骨性Ⅲ类患儿下颌长度与正常牙合的差异最大可达8 mm,因此,将CS3视为开始功能性矫治的理想时间,这对于矫治骨性Ⅲ类错牙合意义重大[21]。 2.4 舌体与牙弓基骨弓的关系 舌体位于固有口腔内,并且时刻与牙弓接触,是参与呼吸、咀嚼、吞咽等功能的重要器官。舌体与口周肌力量的平衡与牙齿在牙弓中的位置排列息息相关。舌头在功能状态下施加的力在引导牙齿萌出、牙弓形成和稳定性方面起着重要作用,如果舌肌和口周肌的动力平衡被打破,上、下颌牙弓及基骨弓的排列将会出现异常,目前大多数学者认为舌体位置、形态大小及运动的异常被认为与牙颌畸形密切相关。因此,舌体与错牙合畸形之间的关系一直以来都是口腔医学界的研究热点问题。但大多数学者们就舌体及口周肌力异常与错牙合畸形之间的关系进行研究,仍未得出一致的结论。 目前大多数研究表明,舌对牙弓及基骨弓的影响毋庸置疑。在吞咽的动态过程中,舌体扮演着重要的解剖结构,涉及到从口腔向胃输送食物、水和唾液的协调活动。LVAREZ等[22]发现骨性Ⅲ类患者吞咽时前后运动及上下运动幅度较骨性Ⅰ、Ⅱ类错牙合大,尤其是前后运动幅度,而左右运动3种错牙合畸形间并无明显异常。在休息时,舌头对硬腭的压力从前到后增加。从端坐位到仰卧位,舌前部压降低,舌后部压略有升高,在吞咽过程中,压力显著增加,吞咽持续时间与体质量呈正相关,与前部腭部长度呈正相关[23]。也就是说腭部长度越长,吞咽持续时间越长,舌肌对牙弓的推力持续时间越长,从而导致前部牙弓、基骨弓宽度越大。此外,骨性Ⅱ类患者的静息舌位更高,在骨性Ⅲ类受试者的舌位置最低,平均舌腭距离较高,其牙弓宽度特征为:与Ⅰ类和Ⅱ类组相比,骨性Ⅲ类上、下颌磨牙间、下颌尖牙间牙弓宽度更大[24]。可能是由于吞咽时舌前伸,导致下颌弓磨牙间宽度、上颌弓总长度、上颌弓周长和后牙弓深度[25]。其中,上颌尖间牙宽度增加的原因可能是为了补偿下颌骨的过长,以掩盖真正的横向骨骼差异。 2.5 儿童骨性Ⅲ类错牙合牙弓及基骨弓的生长发育趋势及特点 对处于生长发育期儿童牙弓和基骨弓骨弓的研究,能够为临床上正确的诊治提供重要理论依据。密切观察和分析儿童时期牙弓及基骨弓的生长变化,及早发现并适时去除影响其正常生长发育的致病因素,不仅对口腔颌面部发育具有重要意义,而且对于指导临床诊断治疗也有一定的作用。目前,对于牙弓及基骨弓生长发育变化的研究方法有2种:一是横向研究,二是纵向研究。 牙弓的三维生长和发展是一种连续和复杂的生物过程,它包括长度、宽度、高度的三维变化,这些生长发育变化各不相同,且变化的大小随着年龄而变化。一般来说,不同年龄段牙弓增长速率及顺序并不相同。通常情况下,牙弓生长发育的顺序为宽度、长度、最后是高度。以往的研究结果表明:牙弓宽度及长度在出生后前2年(6周-2岁)显著增加; 上下牙弓尖牙间/磨牙间宽度的增加,在恒牙列初期前完成(3-13岁),恒牙列萌出后,牙弓宽度稍有缩小(尖牙间宽度减小大于磨牙间宽度);下颌尖牙间宽度在下颌四个切牙萌出后(约8岁),不再增加;由于上颌结节及第二磨牙生长的原因,牙弓后段发育结束较前段晚,其宽度仍会增加。而牙弓长度和高度的发育一直持续到青春高峰期,且高度生长较长度生长更持久,其生长主要是在下颌,随面部高度增加,后牙萌出,牙弓高度增加[26-27]。陈栋[28]研究表明,儿童牙弓前段长度的生长主要集中在5-8岁,随后生长速率趋于稳定,牙弓中后段生长趋势主要集中在9-11岁,且随年龄的增长生长速率逐渐下降;而牙弓宽度的生长在替牙初期趋于稳定,其后,随着年龄的增长生长速率逐渐增大,但是,尖牙宽度约在12岁后减小[29-31]。 基骨弓作为牙弓的支撑部分,其生长与牙弓基本一致,其生长发育并非连续, 而是在生长活跃期与稳定期之间相互转换。除8-10岁这年龄阶段外,替牙期正常牙合儿童随着年龄的增长,基骨长度及宽度均呈现出高度显著的增长趋势。12岁男性儿童上、下颌基骨长度及宽度均大于女性。随着生长发育高峰的来临,在替牙期后期,男、女性儿童生长发育时间及速度不同,12岁儿童基骨长度及宽度出现明显的性别差异。而8岁儿童牙弓长度及宽度、基骨长度及宽度的性别差异,可能与男、 女生长发育的时间不同有关,男孩开始生长发育的时间晚于女孩[32]。上颌基骨宽度增大最快的年龄段为 8-10 岁,而上颌基骨长度在7-10岁发育不明显,从10岁以后才开始出现明显增大。 与Ⅰ类错牙合畸形相比,骨性Ⅲ类错牙合患者面下1/3及下颌骨长度均较长,而且随着年龄的增加,越来越明显。上颌骨与颅底结构的位置关系相对稳定,但是骨性Ⅲ类错牙合下颌骨在乳牙列期就可能表现出较上颌骨前突,而且随着生长会加重,随着上、下颌骨差异性生长,从而导致上、下颌骨间的骨骼不调逐渐严重。骨性Ⅲ类错牙合颌面部的生长发育在早期与正常牙合相差并不是很大,其差异的出现主要是在青春期前、后这段时段内骨性Ⅲ类错牙合的异常生长导致的。研究表明,在生长高峰开始和持续的时间段里,下颌骨的快速生长量与持续的时间呈正相关,即生长高峰持续的时间越长,下颌骨发育得越大,最终导致下颌基骨弓越大[21]。 有研究针对不同错牙合畸形的生长发育高峰期做了统计学分析,发现骨性Ⅲ类错牙合、Ⅰ类错牙合、Ⅱ类错牙合生长发育高峰期开始时间虽然没有显着差异,但骨性Ⅲ类错牙合的患儿青春期生长高峰持续时间比Ⅰ类错牙合、Ⅱ类错牙合分别平均长了6,10个月[33-34]。也就是说,骨性Ⅲ类错牙合在发育最迅猛的阶段平均多发育了6,10个月,并且下颌骨长度的显著变化会一直持续至成年早期(约18岁),此外,在生长发育高峰期(尖牙和前磨牙萌出)和发育晚期(第二、三恒磨牙完全萌出),骨性Ⅲ类错牙合患者的垂直向高度也显著增加。这也说明骨性Ⅲ类错牙合下颌骨的过度生长与较长的生长发育高峰持续时间密切相关。若未经治疗,骨性Ⅲ类错牙合随着时间的推移逐渐恶化,并且不会出现自发的改善,特别是女性,其下颌长度增长约在17岁结束,而男性的下颌增长在18岁后仍继续[35]。 对于牙弓和基骨弓,其生长发育变化与颌骨具有协同性,但也有差异。骨性Ⅲ类错牙合畸形是由于上、下颌骨的差异性生长造成的,主要表现为下颌骨相对于上颌骨生长发育过度,伴或不伴有下前牙代偿性舌倾[36-37]。和Ⅰ类错牙合相比,骨性Ⅲ类大多表现为下颌前突,一般情况下,骨性Ⅲ类错牙合上颌牙弓及基骨弓较Ⅰ类短,下颌牙弓较Ⅰ类大[38],双尖牙、磨牙区宽度比Ⅰ类狭窄,上颌基骨弓宽度比Ⅰ类狭窄,这符合骨性Ⅲ类错牙合患者下颌过大、凹面型的侧貌特征。但也有得出相反的结论,有研究通过比较骨性Ⅲ类错牙合畸形与Ⅰ、Ⅱ类错牙合畸形发现,其结论是骨性Ⅲ类错牙合畸形患者上颌牙弓宽度与正常牙合无显著差异 [39-40]。这可能是由于病例选择的差异造成的,因为骨性Ⅲ类错牙合共有3种基本类型:A型为上颌骨正常,下颌前突;B型为上颌发育不足和下颌骨发育过度,但下颌骨生长相对较多的个体;C型为上颌发育不足,下颌骨正常[41]。 骨性Ⅲ类错牙合畸形在垂直方向上可用高角、均角、低角描述,高角是指面型在垂直方向上发育过度,由于上下颌骨的角度较大,咬合力相对较小,面型也偏长;低角是指面型在垂直向面型发育不足,咬合紧,面下1/3较短、面型较短、方。关于牙弓与垂直骨面型的关系,也有研究报道。牙弓形态与垂直面型呈负相关,高角患者的牙弓形态较窄,低角患者的牙弓形态较宽[42]。 此外,有研究表明,骨性Ⅲ类患儿ANB角和Wits值较正常值偏小。在垂直向上,第一前磨牙弓宽度与垂直骨面型相关,且随着下颌平面角增大,牙弓趋于狭窄[43]。骨性Ⅲ类错牙合FA点更偏舌侧,在前牙区,WALA曲线曲率较FA点曲率更大[44]。通过以往研究大致能够发现,骨性Ⅲ类错牙合畸形颌骨生长发育规律及特点,但目前针对这一方面的研究方法主要是不同年龄阶段的患者,并不是同一批患者的连续追踪观察,生长发育对于结果可能会有误差,这主要是由于骨性Ⅲ类错牙合畸形病例的特殊性,因为研究生长发育规律,最好的方法就是收集一批样本连续观察,这不符合伦理道德,因为对于来到医院就诊的患儿,不可能因为研究需要,就不给予患者相应的治疗,相反,一旦开始治疗,其骨性Ⅲ类错牙合畸形的生长发育也就随之中断。此外,对于牙弓/基骨弓的研究,学者们选择的研究标志点也有差异。目前,选用的标志点多为牙尖点、中央窝点或牙冠最突点/牙根根尖水平、上下颌骨向牙槽骨移行处最狭窄的区域、膜龈联合点等,这可能对于结果也有一定的影响。 2.6 儿童骨性Ⅲ类错牙合的治疗 在正畸治疗中,替牙期是进行功能矫治和颌骨矫形治疗的最佳时期,预防性及阻断性矫治能够早期去除干扰,防止错牙合畸形的进一步发展,引导其向正常方向发育,为将来建立正常牙合打下良好基础。目前对于骨性Ⅲ类错牙合的治疗具有一定的挑战性,其成败在很大程度上取决于患者未来的生长潜力。早期矫治的目的是抑制下颌骨的生长或促进上颌骨的发育,从而避免或降低二期手术的难度[31]。早期矫治能为颅颌面的生长发育提供更有利的环境,并提高咬合关系,研究表明早期治疗还能较大程度的发生骨骼改变,减少牙齿代偿。早期矫治中用于治疗Ⅲ类错牙合矫治器有前牵引面具、头帽颏兜、功能矫治器、生物调节器、反式双阻板矫治器及活动性下颌回缩矫治器,Ⅲ类弹性牵引等[45],临床上可以根据不同情况选择不同的矫治方法[45-64],见表2。 "
| [1] ORTHOP JO, KUNZ F, PLATTE P, et al. impact of specific orthodontic parameters on the oral health-related quality of life in children and adolescents a prospective interdisciplinary, multicentre, cohort study. Orofac Orthop. 2019;80(4):174-183. [2] ANDREWS LF, ANDREWS WA. The six elements of orofacial harmony. Andews J. 2000;1(1):13-22. [3] BALL RL, MINER RM, WILL LA, et al. Comparison of dental and apical base arch forms in Class II Division 1 and Class I malocclusions. Am J Orthod Dentofacial Orthop. 2010;138(1):41-50. [4] LAINE T, ALVESALO L. Palatal and mandibular arch morphology in 47,SYY mean and in other Sex-chromosome anomalies. Arch Oral Biol. 1993;38(2):101. [5] 李九军,李勤,贺永春,等.遗传因素对同卵双生子颅颌面部软硬组织形态的影响研究[J].同济大学学报(医学版),2009,30(3):70-73. [6] 李小兵.牙弓/牙槽骨弓的塑形矫治——基于牙弓形态发育不良的儿童错牙合畸形诊断与阻断治疗[J].华西口腔医学杂志,2016,34(6): 556-563. [7] 盛丽,李桃,吾尔肯·卡满别克,等.混合牙列期下前牙拥挤与牙弓、基骨弓相关性研究[J].口腔医学研究,2019,35(11):1057-1061. [8] OLIVA B, SFERRA S, GRECO LG, et al. Three-dimensional analysis of dental arch forms in Italian population. Prog Orthod. 2018;19(1):34. [9] OMAR H, ALHAJRASI M, FELEMBAN N, et al. Dental arch dimensions, form and tooth size ratio among a Saudi sample. Saudi Med J. 2018; 39(1):86. [10] NOJIMA K, MCLAUGHLIN RP, ISSHIKI Y, et al. A comparative study of Caucasian and Japanese mandibular clinical arch forms. Angle Orthod. 2001;71(3):195-200. [11] KOOK YA, NOJIMA K, MOON HB, et al. Comparison of arch forms between Korean and North American white populations. Am J Orthod Dentofacial Orthop 2004;126(6):680-686. [12] BURRIS BG, HARRIS EF. Maxillary arch size and shape in American blacks and whites. Angle Orthodontist. 2000;70(4):297. [13] LING J, WONG R. Dental arch widths of Southern Chinese. Angle Orthod. 2009;79(1):54-63. [14] 刘敏.维吾尔族与汉族正常(牙合)牙弓与基骨形态对比研究[D].兰州:兰州大学,2018. [15] Negishi S, Richards LC, Kasai K. Relation of dietary preference to masticatory movement and masticatory exercises in Japanese children. Arch Oral Biol. 2019;13(108):104540. [16] MUTLU E, PARLAK B, KURU S, et al. Evaluation of crossbites in relation with dental arch widths, occlusion type, nutritive and non-nutritive sucking habits and respiratory factors in the early mixed dentition. Oral Health Prev Dent. 2019;17(5):447-455. [17] 马梦婷,吕大梅.儿童口腔不良习惯预防管理联合咬合诱导治疗错畸形效果[J].现代医学与健康研究电子杂志,2019,3(4):20-21, 25. [18] MASUMOTO T, HAYASHI I, KAWAMURA A, et al. Relationships among facial type, buccolingual molar inclination, and cortical bone thickness of the mandible. Eur J Orthod. 2001;23(1):15-23. [19] WESTWOOD PV, MCNAMARA JA JR, BACCETTI T, et al. Long-term effects of Class III treatment with rapid maxillary expansion and facemask therapy followed by fixed appliances. Am J Orthod Dentofacial Orthop 2003;123(3):306-320. [20] BACCETTI T, FRANCHI L, MCNAMARA JA. An improved version of the cervical vertebral maturation (CVM) method for the assessment of mandibular growth. Angle Orthod. 2002;72(4):316-323. [21] SALAZAR-LAZO R, ARRIOLA-GUILLÉN LE, FLORES-MIR C. Duration of the peak of adolescent growth spurt in class i and ii malocclusion subjects using a cervical vertebrae maturation analysis. Acta Odontol Latinoam. 2014;27(2):96-101. [22] LVAREZ G, FJ DÍAS, LEZCANO F, et al. Description of tongue movements on swallowing patterns. Arch Oral Biol. 2020;113(5):104706. [23] YU M, GAO X. Tongue pressure distribution of individual normal occlusions and exploration of related factors. J Oral Rehabil. 2018;46(3):249-256. [24] FARHEEN, FATIMA, MUBASSAR, et al. The assessment of resting tongue posture in different sagittal skeletal patterns. Dent Press J Orthod. 2019;24(3):55-63. [25] GUTIÉRREZ DAR, GARZÓN JS, FRANCO JQ, et al. Anterior open bite and its relationship with dental arch dimensions and tongue position during swallowing and phonation in individuals aged 8–16 years: a retrospective case–control study. Int Orthod. 2021;19(1):107-116. [26] YANG D, LIANG S, ZHANG K, et al. Evaluation of growth and development of late mixed dentition upper dental arch with normal occlusion using 3-dimensional digital models. J Health Eng. 2019; 2019(5):1-8. [27] BISHARA SE, JAKOBWEN JR, TREDER J, et al. Arch width changes from 6 weeks to 45 years of age. Am J Orthod Dentofacial Orthop. 1997;111(4):401-409 [28] 陈栋.福建省政和县儿童牙弓和腭穹发育的六年纵向研究[D].福州:福建医科大学,2011. [29] TSUJINO K, MACHIDA Y. A longitudinal study of the growth and development of the dental arch width from childhood to adolescence in Japanese. Bullet Tokyo Dent Coll. 1998;39(2):75-89. [30] WEN YF, WONG HM, PEI T, et al. Adolescent dental arch development among Southern Chinese in Hong Kong: a geometric morphometric approach. Sci Rep. 2019;9(1):18526-18526. [31] 李小兵.基于牙弓形态大小发育的青少年隐形矫治[J].中国实用口腔科杂志,2019,12(8):449-454. [32] 张昆,陈远萍,闫翔,等.120例替牙期正常牙合儿童牙弓及基骨测量分析[J].宁夏医科大学学报,2018,40(4):398-402. [33] WAQAR J, MUBASSAR F, ATTIVA S. The duration of pubertal growth peak among three skeletal classes. Dent Press J Orthod. 2016;21(5): 67-74. [34] SZEMRAJ-FOLMER A, WOJTASZEK-SOMINSKA A, RACKA-PILSZAK B, et al. Duration of the pubertal growth spurt in patients with increased craniofacial growth component in sagittal and vertical planes-retrospective and cross-sectional study. Clin Oral Invest. 2021; 25(8):4907-4914. [35] RUTILI V, NIERI M, GIUNTINI V, et al. A multilevel analysis of craniofacial growth in subjects with untreated Class III malocclusion. Orthod Craniofac Res. 2020;23(2):181-191. [36] 贺泽群,曾欢,唐欢,等.替牙列期儿童错颌畸形颅-颌骨及牙弓的测量分析[J].重庆医科大学学报,2018;43(10):82-87. [37] AUCONI P, SCAZZOCCHIO M, CALDARELLI G, et al. Understanding interactions among cephalometrics variables during growth in untreated Class III subjects. Eur J Orthod. 2017;39(4):1-7. [38] YUN-JIN K, SUNG-HWAN C, BYEONG-TAK K, et al. Maxillomandibular arch width differences at estimated centers of resistance: comparison between normal occlusion and skeletal Class III malocclusion. Korean J Orthod. 2017;47(3):167-175. [39] 林思豆,吴补领,孙风阳,等.三类骨性错牙合下颌牙弓和基骨弓的测量及相关性分析[J].中国临床解剖学杂志,2016,34(2):171-175. [40] 刘颖,肖丹娜,孙留振,等.骨性Ⅲ类错牙合牙弓,基骨弓宽度及协调性分析[J].中华口腔正畸学杂志,2013,20(2):81-84. [41] PARK JU, BAIK SH. Classification of Angle Class III malocclusion and its treatment modalities. Int J Adult Orthodon Orthognath Surg. 2001; 16(1):19-29. [42] SHARMA A, PHOR D, UPADHYAY S, et al. Correlation between vertical facial patterns and dental arch forms in different types of skeletal malocclusions. J Dent Med Sci. 2018;17(9):67-88. [43] 金超超,邵玶.Ⅲ类错牙合垂直骨面型与牙弓宽度关系的研究[J].口腔医学,2018,38(1):52-54. [44] ZUU W, JIAN JH, XU TM, et al. Relationship between mandibular dental and basal bone arch forms for severe skeletal Class III patients. Am J Orthod Dent Orthop. 2015;147(1):37-44. [45] WOON SC, THIRUVENKATACHARI B. Early orthodontic treatment for Class III malocclusion: a systematic review and meta-analysis. Am J Orthod Dentofacial Orthop. 2017;151(1):28-52. [46] MCNAMARA JA JR, FRANCHI L, MCCLATCHEY LM. Orthodontic and orthopedic expansion of the transverse dimension: a four decade perspective. Semin Orthod. 2019;25(1):3-15. [47] MOAWAD SG, BOUSERHAL J, Al-MUNAJED MK. Assessment of the efficiency of Erbium-YAG laser as an assistant method to rapid maxillary expansion: an in vivo study. Int Orthod. 2016;14(4):462-475. [48] OZZEYBKE CFS, TURKKAHRAMAN H. Effects of rapid maxillary expansion and facemask therapy on the soft tissue profiles of class III patients at different growth stages. Eur J Dent. 2019;13(2):143-149. [49] ALYESSARY AS, OTHMAN SA, YAP AUJ, et al. Effects of non-surgical rapid maxillary expansion on nasal structures and breathing: a systematic review. Int Orthod. 2019;17(1):12-19. [50] CAPPELLETTE MJR, NAGAI LHY, GONCALVES RM, et al. Skeletal effects of RME in the transverse and vertical dimensions of the nasal cavity in mouth-breathing growing children. Dental Press J Orthod. 2017;22(4):61-69. [51] MANDALL N, COUSLEY R, DIBIASE A, et al. Early class III protraction facemask treatment reduces the need for orthognathic surgery: a multi-centre, two-arm parallel randomized, controlled trial. J Orthod. 2016;43(3):164-175. [52] ZHANG YW, SHEN G. The effects of maxillary protraction treatment with rapid maxillary expansion for skeletal Class Ⅲ malocclusion. Shanghai Kou Qiang Yi Xue. 2016;25(3):327-333. [53] DAKHLAOUI H, BEN El KAHLA R, GMATI H, et al. Early treatment of Class III malocclusion by maxillary protraction facial mask: effects on craniofacial structures and upper airway dimensions. Orthod Fr. 2020;91(3):239-248. [54] DANAEI SM, AJAMI S, ETEMADI H, et al. Assessment of the effect of maxillary protraction appliance on pharyngeal airway dimensions in relation to changes in tongue posture. Dent Res J. 2018;15(3):208-214. [55] HWABG DM, LEE JY, CHOI YJ, et al. Evaluations of the tongue and hyoid bone positions and pharyngeal airway dimensions after maxillary protraction treatment. Cranio. 2019;37(4):214-222. [56] SMYTH RSD, RYAN FS. Early treatment of class Ⅲ malocclusion with facemask. Evid Based Dent. 2017;18(4):107-108. [57] DU Y, HUANG S, RAO N, et al. Skeletal Class Ⅲ patients treated with Fränkel function regulator type Ⅲ in the early and late mixed dentition. Zhonghua Kou Qiang Yi Xue Za Zhi. 2016;51(5):257-262. [58] 张楠,汪隼,樊林峰,等.FRⅢ矫治功能性和早期骨性安氏Ⅲ类错 牙合的软组织变化[J].上海口腔医学,2017,26(6):658-661. [59] 张楠,汪隼,郑为,等.FRⅢ矫治功能性和早期骨性安氏Ⅲ类错牙合的硬组织变化[J].上海口腔医学,2016,25(6):725-728. [60] AKIN M, UCAR FI, CHOUSEIN C, et al. Effects of chincup or facemask therapies on the orofacial airway and hyoid position in Class III subjects. J Orofac Orthop. 2015;76(6):520-530. [61] STAMPFL M, MUCHITSCH AP, et al. Long-term skeletal and dental effects of facemask versus chincup treatment in Class III patients. J Orofac Orthop. 2017;78(4):1-7. [62] MIURA KI, YAMAOKA S, ARIZONO K, et al. Long-term skeletal stability in the treatment of mandibular prognathism with a physiological positioning strategy. Br J Oral Maxillofac Surg. 2019;57(6):529-535. [63] REZAEI F, MASALEHI H, GOLSHAH A, et al. Oral health related quality of life of patients with class III skeletal malocclusion before and after orthognathic surgery. BMC Oral Health. 2019;19(9):93-97. [64] HWANG HS, OH MH, OH HK, et al. Surgery-first approach in correcting skeletal Class III malocclusion with mandibular asymmetry. Am J Orthod Dentofacial Orthop. 2017;152(2):255-267. |
| [1] | Nong Fuxiang, Jiang Zhixiong, Li Yinghao, Xu Wencong, Shi Zhilan, Luo Hui, Zhang Qinglang, Zhong Shuang, Tang Meiwen. Bone cement augmented proximal femoral nail antirotation for type A3.3 intertrochanteric femoral fracturalysis [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(在线): 1-10. |
| [2] | Pan Zhongjie, Qin Zhihong, Zheng Tiejun, Ding Xiaofei, Liao Shijie. Targeting of non-coding RNAs in the pathogenesis of the osteonecrosis of the femoral head [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(9): 1441-1447. |
| [3] | Cai Zhihao, Xie Zhaoyong. Femoral neck anteversion measurement assessment: how to establish a unified method and standard [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(9): 1448-1454. |
| [4] | Dang Yi, Du Chengyan, Yao Honglin, Yuan Nenghua, Cao Jin, Xiong Shan, Zhang Dingmei, Wang Xin. Hormonal osteonecrosis and oxidative stress [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(9): 1469-1476. |
| [5] | Wang Ji, Zhang Min, Yang Zhongya, Zhang Long. A review of physical activity intervention in type 2 diabetes mellitus with sarcopenia [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(8): 1272-1277. |
| [6] | Nie Chenchen, Su Kaiqi, Gao Jing, Fan Yongfu, Ruan Xiaodi, Yuan Jie, Duan Zhaoyuan, Feng Xiaodong. The regulatory role of circular RNAs in cerebral ischemia-reperfusion injury [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(8): 1286-1291. |
| [7] | Gao Yu, Han Jiahui, Ge Xin. Immunoinflammatory microenvironment after spinal cord ischemia-reperfusion injury [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(8): 1300-1305. |
| [8] | Zhu Lin, Gu Weiping, Wang Can, Chen Gang. Biomechanical analysis of All-on-Four and pterygomaxillary implants under different maxillary bone conditions [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(7): 985-991. |
| [9] | Xu Xingxing, Wen Chaoju, Meng Maohua, Wang Qinying, Chen Jingqiao, Dong Qiang. Carbon nanomaterials in oral implant [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(7): 1062-1070. |
| [10] | Li Cheng, Zheng Guoshuang, Kuai Xiandong, Yu Weiting. Alginate scaffold in articular cartilage repair [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(7): 1080-1088. |
| [11] | Chen Shisong, Liu Xiaohong, Xu Zhiyun. Current status and prospects of bioprosthetic heart valves [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(7): 1096-1102. |
| [12] | Lu Di, Zhang Cheng, Duan Rongquan, Liu Zongxiang. Osteoinductive properties of calcium phosphate ceramic bone repair materials [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(7): 1103-1109. |
| [13] | Shi Yehong, Wang Cheng, Chen Shijiu. Early thrombosis and prevention of small-diameter blood vessel prosthesis [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(7): 1110-1116. |
| [14] | Tang Haotian, Liao Rongdong, Tian Jing. Application and design of piezoelectric materials for bone defect repair [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(7): 1117-1125. |
| [15] | Bai Siqi, Xiao Zhen, Liu Jing. Application potential of adipose-derived stem cells in female pelvic floor dysfunction diseases [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(6): 921-927. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||