| [1] 李钦亮,刘艺,陈鸣,等.颈椎双开门椎管扩大成形同种异体骨植骨治疗脊髓型颈椎病的疗效分析[J].颈腰痛杂志, 2011, 32(4):276-278.
[2] 郑军,申才良.颈椎后纵韧带骨化症后路手术治疗进展[J].颈腰痛杂志,2011,32(1):57-59.
[3] 汤志宏.颈椎双开门棘突植骨造盖术治疗颈椎管狭窄[J].四川医学,2010,31(5):651-652.
[4] 梁博伟,赵劲民,殷国前,等.颈前路分段减压双钢板固定术治疗“跳跃”型脊髓型颈椎病[J].中国修复重建外科杂志,2010,24(12):1480-1484.
[5] 胡祥怀,高宏斌,丁青华,等.颈椎前路手术治疗脊髓型颈椎病的临床应用[J].中国临床研究,2012,25(9):880-881.
[6] Furlan JC, Kalsi-Ryan S, Kailaya-Vasan A, et al. Functional and clinical outcomes following surgical treatment in patients with cervical spondylotic myelopathy: a prospective study of 81 cases.J Neurosurg Spine. 2011;14(3):348-355.
[7] Komura S, Miyamoto K, Hosoe H, et al. Anterior cervical multilevel decompression and fusion using fibular strut as revision surgery for failed cervical laminoplasty. Arch Orthop Trauma Surg. 2011;131(9): 1177-1185.
[8] 王宇,彭雄奇.腰椎椎间植骨融合有限元分析[J].力学学报,2011,43(2):381-389.
[9] 王端勋,闫小磊,朱光,等.101例胸腰椎段脊柱骨折合并脊髓损伤手术治疗[J].中国实用神经疾病杂志,2014,17(5): 91-92.
[10] 左自军,曹永伟,任银祥,等.真假性腰椎滑脱的影像学表现及鉴别价值[J].中国医药导刊,2010,12(10):1701-1702.
[11] 方忠,李锋.退变性腰椎滑脱症的治疗进展[J].生物骨科材料与临床研究,2010,7(4):25-27.
[12] 杜应军,李远洪.椎弓根螺钉内固定联合椎间植骨融合治疗多节段腰椎滑脱[J].现代医药卫生,2010,12(1): 453-454.
[13] 许峰,韦江波.环锯加盖植骨法在腰椎椎间植骨融合中的临床研究[J].昆明医学院学报,2011,22(2):74-75.
[14] 周若南,彭庆州,吴宏伟.后路椎弓根螺钉复位椎间融合内固定治疗腰椎滑脱的临床研究[J].中国实用医药, 2012, 7(5):71-72.
[15] 黄承夸,韦文,陆文忠.椎间植骨Cgae联合椎弓根钉内固定治疗腰椎滑脱症58例分析[J].中国误诊学杂志, 2012, 12(5):1161-1162.
[16] Kasliwal MK, Smith JS, Shaffrey CI, et al. Short-term complications associated with surgery for high-grade spondylolisthesis in adults and pediatric patients: a report from the scoliosis research society morbidity and mortality database. Neurosurgery. 2012;71(1): 109-116.
[17] Martiniani M, Lamartina C, Specchia N. “In situ” fusion or reduction in high-grade high dysplastic developmental spondylolisthesis (HDSS). Eur Spine J. 2012;21(1):S134-140.
[18] 晏雄伟,张洪燕,廉凯,等.两枚椎间融合器及短节段椎弓螺钉内固定治疗腰椎失稳症35例分析[J].中国医药导刊, 2012, 14(2):357.
[19] 陈威,王冰,钟华.不同植骨融合术治疗腰椎滑脱症的疗效比较分析JI].中国骨伤,2011,24(1):11-12.
[20] 武永娟,王大鹏,楚永杰.椎弓根螺钉内固定及经后路椎体间植骨治疗腰椎滑脱[J].中外医疗,2010,42(7):842-843.
[21] 夏世银,王全美,薛治宇.后路减压钉棒固定椎间融合器植骨融合治疗32例腰椎滑脱[J].重庆医学,2010, 39(5):601-602.
[22] Labelle H, Mac-Thiong JM, Roussouly P. Spino-pelvic sagittal balance of spondylolisthesis: a review and classi cation. Eur Spine J. 2011;20(5):641-646.
[23] Karampalis C, Grevitt M, Shafafy M, et al. High-grade spondylolis-thesis: gradual reduction using Magerl’s external xator followed by circumferential fusion technique and long-term results. Eur Spine J. 2012; 21(2):S200-206.
[24] 肖智青,王凤龙,朱锦忠,等.椎间植骨与椎间融合器治疗腰椎滑脱的疗效比较[J].实用中西医结合杂志,2011,11(4): 12-13.
[25] Min K, Liebscher T, Rothenuh D. Sacral dome resection and single-stage posterior reduction in the treatment of high-grade high dysplastic spondylolisthesis in adolescents and young adults. Eur Spine J. 2012;21(6): S785-791.
[26] 贾鹏,赵文国,王勇贵.腰椎滑脱椎弓根螺钉内固定术后临近节段椎间隙变化的相关研究[J].新乡医学院学报,2013, 30(8):632-634.
[27] Bourghli A, Aunoble S, Reebye O, et al. Correlation of clinical outcome and spinopelvic sagittal alignment after surgical treatment of low-grade isthmic spondylolisthesis. Eur Spine J. 2011;20(5):663-668.
[28] 华树良,韦文,陆文忠,等.椎间植骨融合加椎弓根螺钉内固定治疗腰椎滑脱症39例疗效分析[J].广西医学,2012, 34(5):621-622.
[29] Schuller S, Charles YP, Steib JP. Sagittal spinopelvic alignment and body mass index in patients with degenerative spondylolisthesis. Eur Spine J. 2011; 20(5):713-719.
[30] Lamartina C, Berjano P, Petruzzi M, et al. Criteria to restore the sagittal balance in deformity and degenerative spondylolisthesis. Eur Spine J. 2012; 21(1):S27-31.
[31] Imajo Y, Kato Y, Yonemura H, et al.Relative vulnerability of various spinal tracts in C3-4 cervical spondylotic myelopathy: multi-modal spinal cord evoked potentials. Spinal Cord. 2011;49(11):1128-1133.
[32] Lin Q, Zhou X, Wang X, et al. A comparison of anterior cervical discectomy and corpectomy in patients with multilevel cervical spondylotic myelopathy.Eur Spine J. 2012;21(3):474-481. |
.jpg)
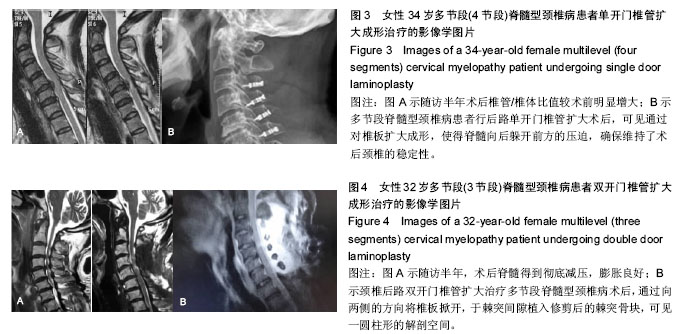
.jpg)
.jpg)
.jpg)