| [1] Qi QY, Chen W, Li XL, et al.H?S protecting against lung injury following limb ischemia-reperfusion by alleviating inflammation and water transport abnormality in rats.Biomed Environ Sci.2014;27(6):410-418.
[2] Aydin MS, Caliskan A, Kocarslan A, et al.Intraperitoneal curcumin decreased lung, renal and heart injury in abdominal aorta ischemia/reperfusion model in rat.Int J Surg.2014;12(6): 601-605.
[3] Cao HB, Zhang LY.Effect of ischemic preconditioning on the expression of P-selectin in the lung injury following ischemia/reperfusion in the hind limbs of rats.Zhongguo Ying Yong Sheng Li Xue Za Zhi.2013;29(3):237-238, 250.
[4] Chen LN, Yang XH, Nissen DH, et al.Dysregulated renin-angiotensin system contributes to acute lung injury caused by hind-limb ischemia-reperfusion in mice.Shock. 2013;40(5):420-429.
[5] Duehrkop C, Banz Y, Spirig R, et al.C1 esterase inhibitor reduces lower extremity ischemia/reperfusion injury and associated lung damage.PLoS One.2013;8(8):e72059.
[6] Murry CE, Jennings RB, Reimer KA. Preconditioning with ischemia: a delay of lethal cell injury in ischemic myocardium.Circulation.1986;74(5):1124-1136.
[7] Saad MA, Abdelsalam RM, Kenawy SA, et al.Ischemic preconditioning and postconditioning alleviates hippocampal tissue damage through abrogation of apoptosis modulated by oxidative stress and inflammation during transient global cerebral ischemia-reperfusion in rats.Chem Biol Interact.2015; 232:21-29.
[8] Costa FL, Yamaki VN, Gonçalves TB, et al.Combined remote ischemic perconditioning and local postconditioning on liver ischemia-reperfusion injury.J Surg Res.2014;192(1):98-102.
[9] Lu YZ, Wang J, Song J, et al.Effect of ischemic postconditioning on the expression of myocardium matris metalloproteinase-2 induced by ischemia/reperfusion in rats.Zhongguo Ying Yong Sheng Li Xue Za Zhi.2014;30(1): 81-84.
[10] Zhang Q, Yan S, Tian Y, et al. Ischemic preconditioning improves liver tolerance to congestion-reperfusion injury in mice.J Surg Res.2014;189(1):152-158.
[11] Cao C, Wang S, Fan L, et al. Renal protection by ischemic preconditioning is associated with p50/p50 homodimers.Am J Nephrol.2010;31(2):1-8.
[12] Xia DY, Li W, Qian HR, et al. Ischemia preconditioning is neuroprotective in a rat cerebral ischemic injury model through autophagy activation and apoptosis inhibition.Braz J Med Biol Res.2013;46(7):580-588.
[13] Mansour Z,Bouitbir J,Charles AL,et al.Remote and local ischemic preconditioning equivalently protects rat skeletal muscle mitochondrial function during experimental aortic cross-clamping.J Vascul surg.2012;55(2):497-505.
[14] Eppinger MJ, Jones ML, Deeb GM, et al.Pattern of injury and the role of neutrophils in reperfusion injury of rat lung.J Surg Res.1995;58(6):713-718.
[15] Fukahori M, Murata T, Mohammed MU, et al.Early reperfusion induces alveolar injury in pulmonary embolism.Chest.1997; 111(1):198-203.
[16] Fadel E, Riou JY, Mazmanian M, et al.Pulmonary thromboendarterectomy for chronic thromboembolic obstruction of the pulmonary artery in piglets.J Thorac Cardiovasc Surg.1999;117(4):787-793.
[17] Li C, Xu M, Wu Y, et al.Limb remote ischemic preconditioning attenuates lung injury after pulmonary resection under propofol-remifentanil anesthesia: a randomized controlled study. Anesthesiology.2014;121(2):249-259.
[18] Geng ZL, Wu JW, Ma HL, et al.Effects of limb ischemia precondition on pulmonary free radicals and cytokine levels in a rabbit model of lung ischemia-reperfusion injury.Zhonghua Wai Ke Za Zhi.2010;48(13):1009-1012.
[19] Yu L, Luo Q, Fang H.Mechanism of ulinastatin protection against lung injury caused by lower limb ischemia-reperfusion. Panminerva Med.2014;56(1):49-55.
[20] Dong LY,Zheng JH, Qiu XX, et al.Ischemic preconditioning reduces deep hypothermic circulatory arrest cardiopulmonary bypass induced lung injury.Eur Rev Med Pharmacol Sci.2013; 17(13):1789-1799.
[21] Gyurkovics E,Aranyi P,Stangl R,et al.Postconditioning of the lower limb--protection against the reperfusion syndrome.J Surg Res.2011;169(1):139-147.
[22] Ren C, Yan Z, Wei D, et al.Limb remote ischemic postconditioning protects against focal ischemia in rats.Brain Res.2009;1288:88-94.
[23] Garbaisz D, Turóczi Z, Fülöp A, et al.Postconditioning can reduce long-term lung injury after lower limb ischemia-reperfusion.Magy Seb.2013;66(3):146-154.
[24] van den Berg E, Bem RA, Bos AP, et al.The effect of TIP on pneumovirus-induced pulmonary edema in mice.PLoS One. 2014;9(7):e102749.
[25] Park JW, Kang JW, Jeon WJ, et al. Postconditioning protects skeletal muscle from ischemia-reperfusion injury. Microsurgery. 2010;30(3): 223-229.
[26] Smith JK, Grisham MB, Granger DN, et al. Free radical defense mechanisms and neutrophil infiltration in postischemic skeletal muscle. Am J Physiol.1989;256(3 Pt 2):H789-93.
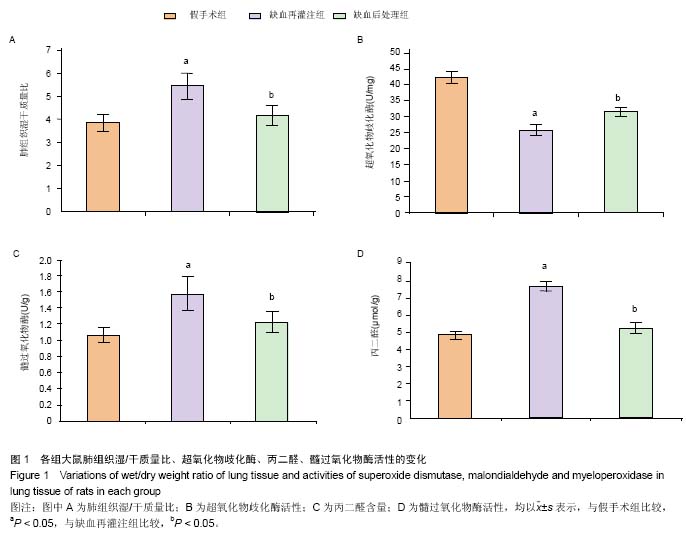
[27] Zheng W,Huang LZ,Zhao L,et al.Superoxide dismutase activity and malondialdehyde level in plasma and morphological evaluation of acute severe hemorrhagic shock in rats. Am J Emerg Med.2008;26(1): 54-58.
[28] Charles AL, Guilbert AS, Bouitbir J, et al. Effect of postconditioning on mitochondrial ysfunction in experimental aortic cross-clamping. Bri J Surg.2011; 98(4): 511-516.
[29] 姚树桐,桑慧,商战平,等.缺血后处理抑制大鼠肠缺血再灌注后肺组织核因子-κB活化及ICAM-1的表达[J].中国病理生理杂志, 2010,26(8):1570-1574.
[30] 许志扬,许建新,康明强. NF-κB抑制剂对大鼠移植肺缺血再灌注损伤的保护作用[J].中国现代医学杂志,2014,24(25):11-15.
[31] Cao QF,Qu MJ,Yang WQ,et al.schemia postconditioning preventing lung ischemia-reperfusion injury.Gene.2015; 554(1):120-124.
[32] Wu H, Lei S, Yuan J, et al.Ischemic postconditioning downregulates Egr-1 expression and attenuates postischemic pulmonary inflammatory cytokine release and tissue injury in rats.Surg Res.2013;181(2):204-212.
[33] 陈海娥,马迎春,何金波,等.缺血后处理对肺缺血/再灌注损伤的保护作用及其机制[J].中国应用生理学杂志,2014,30(3): 251-256. |