[1] BURISCH J, ZHAO M, ODES S, et al. The cost of inflammatory bowel disease in high-income settings: a Lancet Gastroenterology & Hepatology Commission. Lancet Gastroenterol Hepatol. 2023;8(5):458-492.
[2] BUIE MJ, QUAN J, WINDSOR JW, et al. Global Hospitalization Trends for Crohn’s Disease and Ulcerative Colitis in the 21st Century: A Systematic Review With Temporal Analyses. Clin Gastroenterol Hepatol. 2023;21(9):2211-2221.
[3] MASSIRONI S, VIGANÒ C, PALERMO A, et al. Inflammation and malnutrition in inflammatory bowel disease. Lancet Gastroenterol Hepatol. 2023;8(6):579-590.
[4] CRUZ-JENTOFT AJ, SAYER AA. Sarcopenia. Lancet. 2019;393(10191):2636-2646.
[5] ZHANG Y, ZHANG L, GAO X, et al. Impact of malnutrition and sarcopenia on quality of life in patients with inflammatory bowel disease: A multicentre study. J Cachexia Sarcopenia Muscle. 2023;14(6):2663-2675.
[6] VALVANO M, CAPANNOLO A, CESARO N, et al. Nutrition, Nutritional Status, Micronutrients Deficiency, and Disease Course of Inflammatory Bowel Disease. Nutrients. 2023;15(17):3824.
[7] VOEGTLIN M, VAVRICKA SR, SCHOEPFER AM, et al. Prevalence of anaemia in inflammatory bowel disease in Switzerland: a cross-sectional study in patients from private practices and university hospitals. J Crohns Colitis. 2010;4(6):642-648.
[8] GODALA M, GASZYŃSKA E, WALCZAK K, et al. Evaluation of Albumin, Transferrin and Transthyretin in Inflammatory Bowel Disease Patients as Disease Activity and Nutritional Status Biomarkers. Nutrients. 2023;15(15):3479.
[9] ZHENG Y, LIAO Y, OUYANG Y, et al. The effects and predictive value of calcium and magnesium concentrations on nutritional improvement, inflammatory response and diagnosis in patients with Crohn’s disease. J Hum Nutr Diet. 2023;36(5):1649-1660.
[10] ALGIERI F, RODRIGUEZ-NOGALES A, GARRIDO-MESA J, et al. Intestinal anti-inflammatory activity of calcium pyruvate in the TNBS model of rat colitis: Comparison with ethyl pyruvate. Biochem Pharmacol. 2016;103:53-63.
[11] CHA KH, YANG JS, KIM KA, et al. Improvement in host metabolic homeostasis and alteration in gut microbiota in mice on the high-fat diet: A comparison of calcium supplements. Food Res Int. 2020; 136:109495.
[12] OPSTELTEN JL, LEENDERS M, DIK VK, et al. Dairy Products, Dietary Calcium, and Risk of Inflammatory Bowel Disease: Results From a European Prospective Cohort Investigation. Inflamm Bowel Dis. 2016;22(6):1403-1411.
[13] CHEN YH, WANG L, FENG SY, et al. The Relationship between C-Reactive Protein/Albumin Ratio and Disease Activity in Patients with Inflammatory Bowel Disease. Gastroenterol Res Pract. 2020;2020:3467419.
[14] PEDERSEN M, CROMWELL J, NAU P. Sarcopenia is a Predictor of Surgical Morbidity in Inflammatory Bowel Disease. Inflamm Bowel Dis. 2017;23(10):1867-1872.
[15] ZHU Z, HASEGAWA K, CAMARGO CA JR, et al. Investigating asthma heterogeneity through shared and distinct genetics: Insights from genome-wide cross-trait analysis. J Allergy Clin Immunol. 2021;147(3):796-807.
[16] CRUZ-JENTOFT AJ, BAHAT G, BAUER J, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019;48(1):16-31.
[17] DENNIS JK, SEALOCK JM, STRAUB P, et al. Clinical laboratory test-wide association scan of polygenic scores identifies biomarkers of complex disease. Genome Med. 2021;13(1):6.
[18] MANOUSAKI D, MITCHELL R, DUDDING T, et al. Genome-wide Association Study for Vitamin D Levels Reveals 69 Independent Loci. Am J Hum Genet. 2020;106(3):327-337.
[19] MBATCHOU J, BARNARD L, BACKMAN J, et al. Computationally efficient whole-genome regression for quantitative and binary traits. Nat Genet. 2021;53(7):1097-1103.
[20] DAVYSON E, SHEN X, GADD DA, et al. Metabolomic Investigation of Major Depressive Disorder Identifies a Potentially Causal Association With Polyunsaturated Fatty Acids. Biol Psychiatry. 2023;94(8):630-639.
[21] PEI YF, LIU YZ, YANG XL, et al. The genetic architecture of appendicular lean mass characterized by association analysis in the UK Biobank study. Commun Biol. 2020; 3(1):608.
[22] JUNG H, JUNG HU, BAEk EJ, et al. Integration of risk factor polygenic risk score with disease polygenic risk score for disease prediction. Commun Biol. 2024;7(1):180.
[23] BULIK-SULLIVAN BK, LOH PR, FINUCANE HK, et al. LD Score regression distinguishes confounding from polygenicity in genome-wide association studies. Nat Genet. 2015; 47(3):291-295.
[24] FINUCANE HK, BULIK-SULLIVAN B, GUSEV A, et al. Partitioning heritability by functional annotation using genome-wide association summary statistics. Nat Genet. 2015;47(11):1228-1235.
[25] AUTON A, BROOKS LD, DURBIN RM, et al. A global reference for human genetic variation. Nature. 2015;526(7571):68-74.
[26] WIELSCHER M, AMARAL AFS, VAN DER PLAAT D, et al. Genetic correlation and causal relationships between cardio-metabolic traits and lung function impairment. Genome Med. 2021; 13(1):104.
[27] ZHU X, FENG T, TAYO BO, et al. Meta-analysis of correlated traits via summary statistics from GWASs with an application in hypertension. Am J Hum Genet. 2015; 96(1):21-36.
[28] PURCELL S, NEALE B, TODD-BROWN K, et al. PLINK: a tool set for whole-genome association and population-based linkage analyses. Am J Hum Genet. 2007;81(3):559-575.
[29] CHOU MH, YANG YK, WANG JD, et al. The Association of Serum and Dietary Magnesium with Depressive Symptoms. Nutrients. 2023;15(3):774.
[30] PIERCE BL, AHSAN H, VANDERWEELE TJ. Power and instrument strength requirements for Mendelian randomization studies using multiple genetic variants. Int J Epidemiol. 2011;40(3):740-752.
[31] LAWLOR DA, HARBORD RM, STERNE JA, et al. Mendelian randomization: using genes as instruments for making causal inferences in epidemiology. Stat Med. 2008;27(8):1133-1163.
[32] BOWDEN J, DAVEY SMITH G, BURGESS S. Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int J Epidemiol. 2015;44(2):512-525.
[33] BOWDEN J, DAVEY SMITH G, HAYCOCK PC, et al. Consistent Estimation in Mendelian Randomization with Some Invalid Instruments Using a Weighted Median Estimator. Genet Epidemiol. 2016; 40(4):304-314.
[34] WEERSMA RK, CRUSIUS JB, ROBERTS RL, et al. Association of FcgR2a, but not FcgR3a, with inflammatory bowel diseases across three Caucasian populations. Inflamm Bowel Dis. 2010;16(12):2080-2089.
[35] RAN Y, WU K, HU C, et al. Downregulated APOD and FCGR2A correlates with immune infiltration and lipid-induced symptoms of irritable bowel syndrome. Sci Rep. 2023; 13(1):14211.
[36] EL YOUSFI M, BREUILLÉ D, PAPET I, et al. Increased tissue protein synthesis during spontaneous inflammatory bowel disease in HLA-B27 rats. Clin Sci (Lond). 2003;105(4):437-446.
[37] KARINEN H, KÄRKKÄINEN P, PIHLAJAMÄKI J, et al. Gene dose effect of the DQB1*0201 allele contributes to severity of coeliac disease. Scand J Gastroenterol. 2006;41(2):191-199.
[38] ROJAS-CRUZ AF, MARTÍN-JIMÉNEZ CA, GONZÁLEZ J, et al. Palmitic Acid Upregulates Type I Interferon-Mediated Antiviral Response and Cholesterol Biosynthesis in Human Astrocytes. Mol Neurobiol. 2023; 60(8):4842-4854.
[39] FAN X, LI Q, WANG Y, et al. Non-canonical NF-κB contributes to endothelial pyroptosis and atherogenesis dependent on IRF-1. Transl Res. 2023;255:1-13.
[40] MA H, HU T, TAO W, et al. A lncRNA from an inflammatory bowel disease risk locus maintains intestinal host-commensal homeostasis. Cell Res. 2023;33(5):372-388.
[41] NOVAKOVA K, TÖRÖK M, PANAJATOVIC M, et al. PGC-1α and MEF2 Regulate the Transcription of the Carnitine Transporter OCTN2 Gene in C2C12 Cells and in Mouse Skeletal Muscle. Int J Mol Sci. 2022;23(20): 12304.
[42] DUTEIL D, CHAMBON C, ALI F, et al. The transcriptional coregulators TIF2 and SRC-1 regulate energy homeostasis by modulating mitochondrial respiration in skeletal muscles. Cell Metab. 2010;12(5):496-508.
[43] PÉREZ-JELDRES T, BUSTAMANTE ML, SEGOVIA-MELERO R, et al. Genotype Prevalence of Lactose Deficiency, Vitamin D Deficiency, and the Vitamin D Receptor in a Chilean Inflammatory Bowel Disease Cohort: Insights from an Observational Study. Int J Mol Sci. 2023;24(19):14866.
[44] TOPALOVA-DIMITROVA A, DIMITROV IV, NIKOLOV R. Lower vitamin D levels are associated with the pathogenesis of inflammatory bowel diseases. Medicine (Baltimore). 2023;102(41):e35505.
[45] SONG F, LU J, CHEN Z, et al. Vitamin D and CRP are associated in hospitalized inflammatory bowel disease (IBD) patients in Shanghai. Asia Pac J Clin Nutr. 2024;33(3):370-380.
[46] LI Y, GUO Y, GENG C, et al. Vitamin D/vitamin D receptor protects intestinal barrier against colitis by positively regulating Notch pathway. Front Pharmacol. 2024;15:1421577.
[47] GAO H, ZHOU H, ZHANG Z, et al. Vitamin D3 alleviates inflammation in ulcerative colitis by activating the VDR-NLRP6 signaling pathway. Front Immunol. 2023; 14:1135930.
[48] WU Z, MA B, XIAO M, et al. Vitamin D Modified DSS-Induced Colitis in Mice via STING Signaling Pathway. Biology (Basel). 2025;14(6):715.
[49] KARIMI S, TABATABA-VAKILI S, YARI Z, et al. The effects of two vitamin D regimens on ulcerative colitis activity index, quality of life and oxidant/anti-oxidant status. Nutr J. 2019;18(1):16.
[50] AHAMED Z R, DUTTA U, SHARMA V, et al. Oral Nano Vitamin D Supplementation Reduces Disease Activity in Ulcerative Colitis: A Double-Blind Randomized Parallel Group Placebo-controlled Trial. J Clin Gastroenterol. 2019;53(10):e409-e415.
[51] VALVANO M, MAGISTRONI M, CESARO N, et al. Effectiveness of Vitamin D Supplementation on Disease Course in Inflammatory Bowel Disease Patients: Systematic Review With Meta-Analysis. Inflamm Bowel Dis. 2024;30(2):281-291.
[52] WALLACE C, GORDON M, SINOPOULOU V, et al. Vitamin D for the treatment of inflammatory bowel disease. Cochrane Database Syst Rev. 2023;10(10):CD011806.
[53] GIUSTINA A, BILEZIKIAN JP, ADLER RA, et al. Consensus Statement on Vitamin D Status Assessment and Supplementation: Whys, Whens, and Hows. Endocr Rev. 2024;45(5):625-654.
[54] HAMILTON FW, HUGHES DA, SPILLER W, et al. Non-linear Mendelian randomization: detection of biases using negative controls with a focus on BMI, Vitamin D and LDL cholesterol. Eur J Epidemiol. 2024;39(5):451-465.
[55] GRANT RK, JONES GR, PLEVRIS N, et al. Validation of the ACE [Albumin, CRP, and Endoscopy] Index in Acute Colitis: Analysis of the CONSTRUCT dataset. J Crohns Colitis. 2024;18(2):286-290.
[56] ZHENG J, FAN Z, LI C, et al. Predictors for colectomy in patients with acute severe ulcerative colitis: a systematic review and meta-analysis. BMJ Open Gastroenterol. 2024;11(1):e001587.
[57] MUNDHRA SK, MADAN D, GOLLA R, et al. Intravenous Albumin Infusion Does not Augment the Response Rate to a Combination of Exclusive Enteral Nutrition and Intravenous Steroids in Acute Severe Ulcerative Colitis: A Randomised Controlled Trial. J Crohns Colitis. 2024;18(11):1870-1878.
[58] SUN Q, YU Z, LUO L, et al. Modulation of Inflammation Levels and the Gut Microbiota in Mice with DSS-Induced Colitis by a Balanced Vegetable Protein Diet. Plant Foods Hum Nutr. 2024;80(1):19.
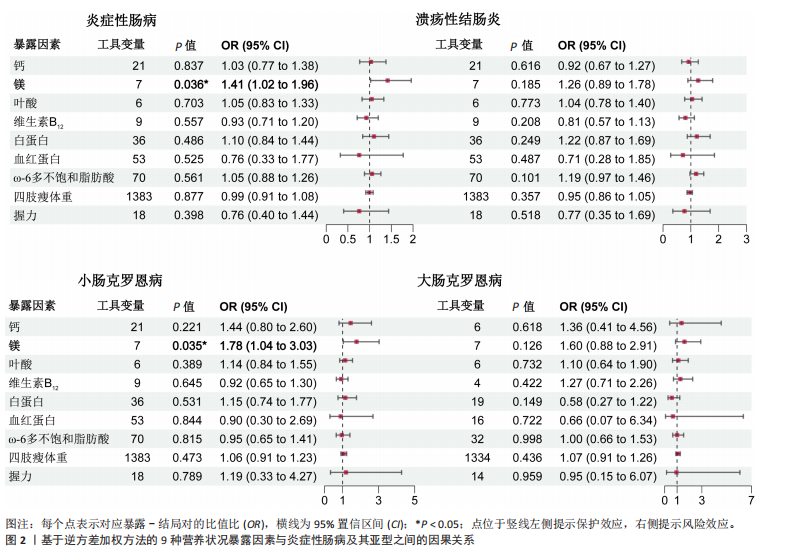
[59] CHEN J, RUAN X, YUAN S, et al. Antioxidants, minerals and vitamins in relation to Crohn’s disease and ulcerative colitis: A Mendelian randomization study. Aliment Pharmacol Ther. 2023;57(4):399-408.
[60] CUI J, LI Y, JIAO C, et al. Improvement of magnesium isoglycyrrhizinate on DSS-induced acute and chronic colitis. Int Immunopharmacol. 2021;90:107194.
[61] DEL CHIERICO F, TRAPANI V, PETITO V, et al. Dietary Magnesium Alleviates Experimental Murine Colitis through Modulation of Gut Microbiota. Nutrients. 2021;13(12):4188.
[62] JAHNEN-DECHENT W, KETTELER M. Magnesium basics. Clin Kidney J. 2012; 5(Suppl 1):i3-i14.
[63] DUNCAN A, TALWAR D, MCMILLAN DC, et al. Quantitative data on the magnitude of the systemic inflammatory response and its effect on micronutrient status based on plasma measurements. Am J Clin Nutr. 2012;95(1):64-71.
[64] CHO JM, YANG HR. Hair Mineral and Trace Element Contents as Reliable Markers of Nutritional Status Compared to Serum Levels of These Elements in Children Newly Diagnosed with Inflammatory Bowel Disease. Biol Trace Elem Res. 2018; 185(1):20-29.
[65] JIN L, CHEN C, LI Y, et al. A Biodegradable Mg-Based Alloy Inhibited the Inflammatory Response of THP-1 Cell-Derived Macrophages Through the TRPM7-PI3K-AKT1 Signaling Axis. Front Immunol. 2019; 10:2798.
[66] FENG Y, FENG W, XU M, et al. Sarcopenia and treatment failure in inflammatory bowel disease: a systematic review and meta-analysis. Rev Esp Enferm Dig. 2024;116(2):68-76.
[67] KOHLI I, THIND N, BHALLA A, et al. Sarcopenia is associated with worse outcomes in patients with inflammatory bowel disease: insights from US national hospitalization data. Eur J Gastroenterol Hepatol. 2025;37(1):55-61.
[68] CHAVEZ C, LIN K, MALVEAUX A, et al. IRF1 cooperates with ISGF3 or GAF to form innate immune de novo enhancers in macrophages. Sci Signal. 2025;18(868): eado8860.
[69] RAVI SUNDAR JOSE GEETHA A, FISCHER K, BABADEI O, et al. Dynamic control of gene expression by ISGF3 and IRF1 during IFNβ and IFNγ signaling. EMBO J. 2024;43(11):2233-2263.
[70] TAN G, HUANG C, CHEN J, et al. An IRF1-dependent Pathway of TNFα-induced Shedding in Intestinal Epithelial Cells. J Crohns Colitis. 2022;16(1):133-142.
[71] XU X, LV X, ZENG R, et al. Elevated levels of IRF1 and CASP1 as pyroptosis-related biomarkers for intestinal epithelial cells in Crohn’s disease. Front Immunol. 2025; 16:1551547.
[72] PINTO-SANCHEZ MI, BLOM JJ, GIBSON PR, et al. Nutrition Assessment and Management in Celiac Disease. Gastroenterology. 2024; 167(1):116-131.e1.
[73] DE LA CONCHA EG, FERNANDEZ-ARQUERO M, SANTA-CRUZ S, et al. Positive and negative associations of distinct HLA-DR2 subtypes with ulcerative colitis (UC). Clin Exp Immunol. 1997;108(3):392-395.
[74] WANG Y, ZHANG F, YAO B,et al. Notch4 participates in mesenchymal stem cell-induced differentiation in 3D-printed matrix and is implicated in eccrine sweat gland morphogenesis. Burns Trauma. 2023;11:tkad032.
[75] SHEKHAWAT PS, SRINIVAS SR, MATERN D, et al. Spontaneous development of intestinal and colonic atrophy and inflammation in the carnitine-deficient jvs (OCTN2(-/-)) mice. Mol Genet Metab. 2007;92(4):315-324.
[76] MULLANY LK, LONARD DM, O’MALLEY BW. Wound Healing-related Functions of the p160 Steroid Receptor Coactivator Family. Endocrinology. 2021;162(3):bqaa232.
|