| [1] Tissue plasminogen activator for acute ischemic stroke. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group.N Engl J Med. 1995;333(24): 1581-1587.
[2] Babikian VL, Kase CS, Pessin MS,et al. Intracerebral hemorrhage in stroke patients anticoagulated with heparin. Stroke. 1989;20(11):1500-1503.
[3] Rosenberg GA.Matrix metalloproteinases in brain injury.J Neurotrauma. 1995;12(5):833-842.
[4] Rosenberg GA. Matrix metalloproteinases in neuroinflammation. Glia. 2002;39(3):279-291.
[5] 李国忠,尹燕红,王德生.出血性转化的研究进展[J].国外医学:脑血管疾病分册,2004,12(12):907-910.
[6] 盛文利,黄如训.重视脑梗死的出血性转化[J].中国神经精神疾病杂志,2012,38(2): 126-128.
[7] Romanic AM, White RF, Arleth AJ, et al. Matrix metalloproteinase expression increases after cerebral focal ischemia in rats: inhibition of matrix metalloproteinase-9 reduces infarct size.Stroke. 1998;29(5):1020-1030.
[8] Lu A, Clark JF, Broderick JP,et al. Reperfusion activates metalloproteinases that contribute to neurovascular injury.Exp Neurol. 2008;210(2):549-559.
[9] Kuluz JW, Gregory GA, Han Y, et al. Fructose-1, 6-bisphosphate reduces infarct volume after reversible middle cerebral artery occlusion in rats.Stroke.1993;24(10): 1576-1583.
[10] 王伟.严格控制实验条件,建立标准化脑缺血动物模型[J].中华神经科杂志,1998,31(5):261-263.
[11] 卜碧涛,王伟,张苏明.大鼠脑缺血模型制作过程中麻醉方法的选择与应用[J].同济医科大学学报,1998,27(3):202-205.
[12] Koizumi J,Yoshida Y,Nakazawa T.Experimental studies of ischemic brain edema:1.A new experimental model of cerebral embolism in rats in which recirculation can be introduced in the ischemic area. Jan J Stroke.1986; 8(5): 1-8.
[13] Longa EZ, Weinstein PR, Carlson S,et al.Reversible middle cerebral artery occlusion without craniectomy in rats.Stroke. 1989;20(1):84-91.
[14] Minematsu K, Li L, Fisher M, et al.Diffusion-weighted magnetic resonance imaging: rapid and quantitative detection of focal brain ischemia.Neurology. 1992;42(1):235-240.
[15] Nagasawa H, Kogure K.Correlation between cerebral blood flow and histologic changes in a new rat model of middle cerebral artery occlusion.Stroke. 1989;20(8): 1037-1043.
[16] Kuge Y, Minematsu K, Yamaguchi T,et al. Nylon monofilament for intraluminal middle cerebral artery occlusion in rats.Stroke. 1995;26(9):1655-1657.
[17] Markgraf CG, Velayo NL, Johnson MP,et al.Six-hour window of opportunity for calpain inhibition in focal cerebral ischemia in rats.Stroke. 1998;29(1):152-158.
[18] Young AR, Touzani O, Derlon JM,et al.Early reperfusion in the anesthetized baboon reduces brain damage following middle cerebral artery occlusion: a quantitative analysis of infarction volume.Stroke. 1997;28(3):632-637.
[19] Nishimura MC, Davis RL, Bartkowski H.Rat middle cerebral artery occlusion: evaluation of the model and development of a neurologic examination.Stroke. 1986; 17(3):472-476.
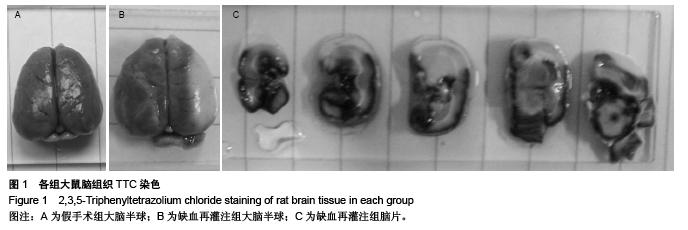
[20] Bederson JB, Pitts LH, Germano SM, et al.Evaluation of 2,3,5-triphenyltetrazolium chloride as a stain for detection and quantification of experimental cerebral infarction in rats.Stroke. 1986;17(6):1304-1308.
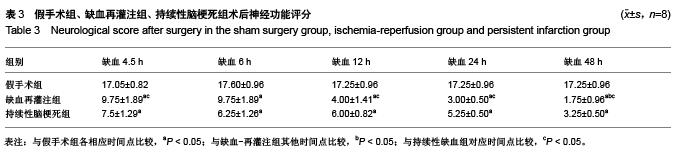
[21] Garcia JH, Wagner S, Liu KF,et al. Neurological deficit and extent of neuronal necrosis attributable to middle cerebral artery occlusion in rats. Statistical validation.Stroke. 1995; 26(4):627-634.
[22] Persson L, Hårdemark HG, Bolander HG,et al.Neurologic and neuropathologic outcome after middle cerebral artery occlusion in rats.Stroke. 1989;20(5):641-645.
[23] Germano IM, Bartkowski HM, Cassel ME,et al.The therapeutic value of nimodipine in experimental focal cerebral ischemia. Neurological outcome and histopathological findings. J Neurosurg. 1987;67(1):81-87.
[24] Nagasawa H, Kogure K.Correlation between cerebral blood flow and histologic changes in a new rat model of middle cerebral artery occlusion.Stroke. 1989;20(8): 1037-1043.
[25] Millikan C.Animal stroke models.Stroke. 1992;23(6): 795-797.
[26] Bederson JB, Pitts LH, Tsuji M,et al.Rat middle cerebral artery occlusion: evaluation of the model and development of a neurologic examination.Stroke. 1986;17(3):472-476.
[27] Ginsberg MD.The validity of rodent brain-ischemia models is self-evident.Arch Neurol. 1996;53(10):1065-1067.
[28] Petty MA, Wettstein JG.Elements of cerebral microvascular ischaemia.Brain Res Brain Res Rev. 2001; 36(1):23-34.
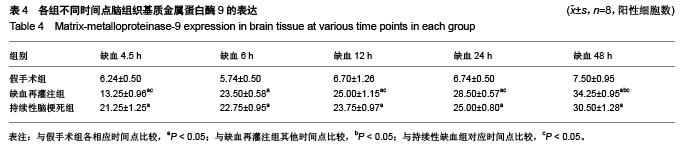
[29] Fujimura M, Gasche Y, Morita-Fujimura Y,et al.Early appearance of activated matrix metalloproteinase-9 and blood-brain barrier disruption in mice after focal cerebral ischemia and reperfusion.Brain Res.1999;842(1):92-100.
[30] Romanic AM, White RF, Arleth AJ,et al.Matrix metalloproteinase expression increases after cerebral focal ischemia in rats: inhibition of matrix metalloproteinase-9 reduces infarct size.Stroke. 1998; 29(5):1020-1030.
[31] Rosenberg GA.Growth and bleeding in BAVM: another role for MMPs.Stroke. 2003;34(4):925-931.
[32] Colton CA, Keri JE, Chen WT,et al.Protease production by cultured microglia: substrate gel analysis and immobilized matrix degradation.J Neurosci Res. 1993;35(3):297-304.
[33] 许宏伟,杨期东,刘晓英,等.MMP-2/9与脑出血后脑水肿的关系探讨[J].中风与神经疾病杂志,2004,21(4):295-297.
[34] Hou HL, Zhang HG, Gong HL, et al. High matrix metalloproteinase-9 expression induces angiogenesis and basement membrane degradation in stroke-prone spontaneously hypertensive rats after cerebral infarction. Neural Regen Res. 2014;9 (11): 1154-1162
[35] Heo JH, Lucero J, Abumiya T,et al.Matrix metalloproteinases increase very early during experimental focal cerebral ischemia.J Cereb Blood Flow Metab. 1999;19(6):624-633.
[36] Lapchak PA, Chapman DF, Nunez SY,et al. Dehydroepiandrosterone sulfate is neuroprotective in a reversible spinal cord ischemia model: possible involvement of GABA(A) receptors.Stroke. 2000;31(8):1953-1956.
[37] Choi ET, Collins ET, Marine LA,et al. Matrix metalloproteinase-9 modulation by resident arterial cells is responsible for injury-induced accelerated atherosclerotic plaque development in apolipoprotein E-deficient mice.Arterioscler Thromb Vasc Biol. 2005;25(5): 1020-1025.
[38] Matter K, Balda MS.Functional analysis of tight junctions. Methods. 2003;30(3):228-234.
[39] Asahi M, Wang X, Mori T,et al. Effects of matrix metalloproteinase-9 gene knock-out on the proteolysis of blood-brain barrier and white matter components after cerebral ischemia.J Neurosci. 2001;21(19):7724-7732.
[40] Rosell A, Cuadrado E, Ortega-Aznar A, et al. MMP-9-positive neutrophil infiltration is associated to blood-brain barrier breakdown and basal lamina type IV collagen degradation during hemorrhagic transformation after human ischemic stroke.Stroke. 2008;39(4):1121-1126.
[41] Kim GW, Gasche Y, Grzeschik S,et al. Neurodegeneration in striatum induced by the mitochondrial toxin 3-nitropropionic acid: role of matrix metalloproteinase-9 in early blood-brain barrier disruption.J Neurosci. 2003; 23(25): 8733-8742.
[42] Gursoy-Ozdemir Y, Qiu J, Matsuoka N,et al.Cortical spreading depression activates and upregulates MMP-9.J Clin Invest. 2004;113(10):1447-1455. |
.jpg)
.jpg)