中国组织工程研究 ›› 2016, Vol. 20 ›› Issue (11): 1532-1537.doi: 10.3969/j.issn.2095-4344.2016.11.002
• 皮肤粘膜组织构建 skin and mucosal tissue construction • 上一篇 下一篇
角膜基质内羊膜移植修复大泡性角膜病变
张 枫,孟维哲
- 滨州市人民医院眼科,山东省滨州市 256610
Amniotic membrane implantation into the corneal stroma for the treatment of bullous keratopathy
Zhang Feng, Meng Wei-zhe
- Department of Ophtalmology, Binzhou People’s Hospital, Binzhou 256610, Shandong Province, China
摘要:
文章快速阅读:
.jpg)
羊膜移植:羊膜是一种透明、有韧性、无神经、血管和淋巴管的组织,其厚度为0.02-0.05 mm,是胚胎来源的组织,抗原性甚微。新鲜羊膜因其带有完整的上皮层,可立即重建眼表上皮,防止胶原组织暴露,阻止胶原的溶解。有活性的羊膜上皮还可分泌细胞因子,如β-转化生长因子、干扰素等成分,可在眼表重建过程中发挥积极作用。但羊膜移植并不能改善已经失代偿的角膜内皮。利用羊膜重建瘢痕期睑球粘连的眼表,能提供一个含基底膜和基质成分的胶原支架,以使受体的结膜或角膜表面的上皮细胞扩展及移行于其上,达到真正的结膜及角膜眼表的重建,减少新生血管的形成,阻止假性胬肉的长入,甚至可延长角膜缘的存活,是眼表重建的重要进展。
大泡性角膜病变:是指角膜上皮或上皮下形成水疱的状态,由角膜内皮细胞的异常或破坏引起。正常角膜内皮细胞数量约为3 000个/mm2,减少至500-1 000个/mm2时,即可发生本病。白内障手术后、眼外伤、青光眼晚期、严重的色素膜炎、Fuch角膜营养不良、角膜移植失败等均可能引起角膜内皮细胞破坏和减少,导致大泡性角膜病变。临床表现为角膜上皮水疱形成,出现疼痛、畏光、流泪等严重刺激症状。
背景:大泡性角膜病变发生率逐年升高,但是角膜移植材料来源少,手术费用较高,且有些患者症状严重,恢复机会较小,角膜移植成功率较小。角膜基质内羊膜来源广,费用低,能够有效缓解患者的症状,提高其生活质量。
目的:对比观察角膜基质内羊膜移植治疗大泡性角膜病变的效果。
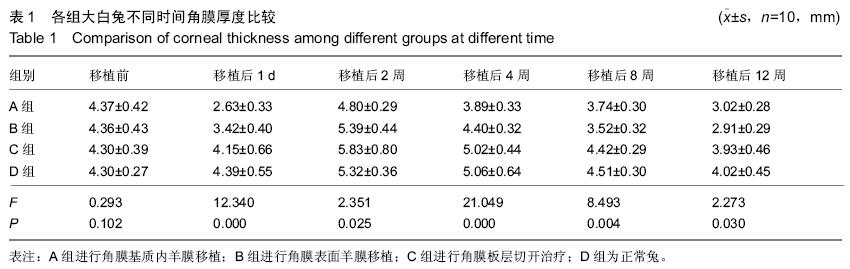
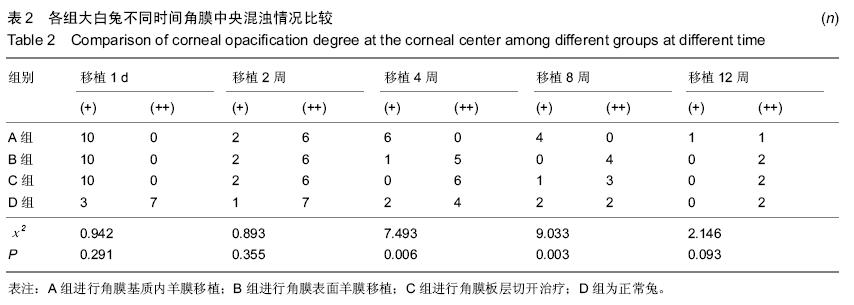
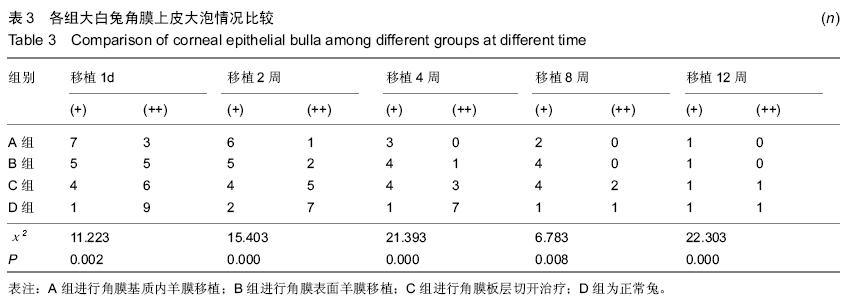
方法:选择40只健康成年新西兰大白兔,雌雄各一半,40只大白兔随机分为4组,各10只。A,B,C组兔建立大泡性角膜病变模型。建模后2周A组进行角膜基质内羊膜移植;B组进行角膜表面羊膜移植;C组进行角膜板层切开治疗,步骤与A组相同,但是不植入羊膜;D组不做手术处理为空白对照。采用固定裂隙灯显微镜的裂隙宽度和光线投射角度,观察各组不同时间大白兔角膜的中央厚度、角膜中央混浊程度及角膜上皮大泡情况。
结果与结论:①移植后1 d、2周时:4组大白兔角膜中央厚度比较差异有显著性意义(P < 0.05);②移植4,8,12周时,角膜基质内羊膜移植组与角膜表面羊膜移植比较差异无显著性意义(P > 0.05),角膜板层切开治疗组与空白对照比较差异无显著性意义(P > 0.05),但与前2组比较差异有统计学意义(P < 0.05);③移植后4,8周时:角膜基质内羊膜移植组角膜混浊程度明显优于其他3组(P < 0.05)。角膜板层切开治疗组切口处形成明显瘢痕,移植后角膜基质内羊膜移植组大泡改善明显高于其他3组(P < 0.05),角膜表面羊膜移植大白兔移植后2周复发,角膜板层切开治疗组、空白对照移植后12周仍然水肿,存在大泡。④结果显示,角膜基质内羊膜移植能够有效帮助大泡性病变大白兔修复角膜内皮细胞,缓解水肿症状,其具体作用机制还需进一步研究。
ORCID: 0000-0003-2439-2785(张枫)