中国组织工程研究 ›› 2015, Vol. 19 ›› Issue (11): 1732-1738.doi: 10.3969/j.issn.2095-4344.2015.11.018
• 肌肉肌腱韧带组织构建 tissue construction of the muscle, tendon and ligament • 上一篇 下一篇
以解剖学定位Lisfranc韧带损伤的植入物内固定修复
郭洪亮1,伊力哈木•托合提1,李山珠2,俞光荣2,王治洲1,甘子明3
- 1新疆医科大学第二附属医院骨科,新疆维吾尔自治区乌鲁木齐市 830063;2上海同济大学附属同济医院骨科,上海市 200065;3新疆医科大学解剖教研室,新疆维吾尔自治区乌鲁木齐市 830000
Internal fixation implants for Lisfranc ligament injury based on anatomical location
Guo Hong-liang1, Yilihamu Tuoheti1, Li Shan-zhu2, Yu Guang-rong2, Wang Zhi-zhou1, Gan Zi-ming3
- 1Department of Orthopedics, the Second Affiliated Hospital of Xinjiang Medical University, Urumqi 830063, Xinjiang Uygur Autonomous Region, China; 2Department of Orthopedics, Tongji Hospital, Tongji University, Shanghai 200065, China; 3Division of Anatomy, Xinjiang Medical University, Urumqi 830000, Xinjiang Uygur Autonomous Region, China
摘要:
背景:跖跗关节(Lisfranc关节)结构复杂、常规X射线片骨关节面重叠,对其诊断较困难。目前对Lisfranc韧带的解剖学研究较少,缺乏相应的形态学资料,导致在相关修复手术中没有该部位的准确解剖参考值。
目的:测量Lisfranc韧带的静态稳定结构,为Lisfranc关节损伤的修复提供临床解剖学基础。
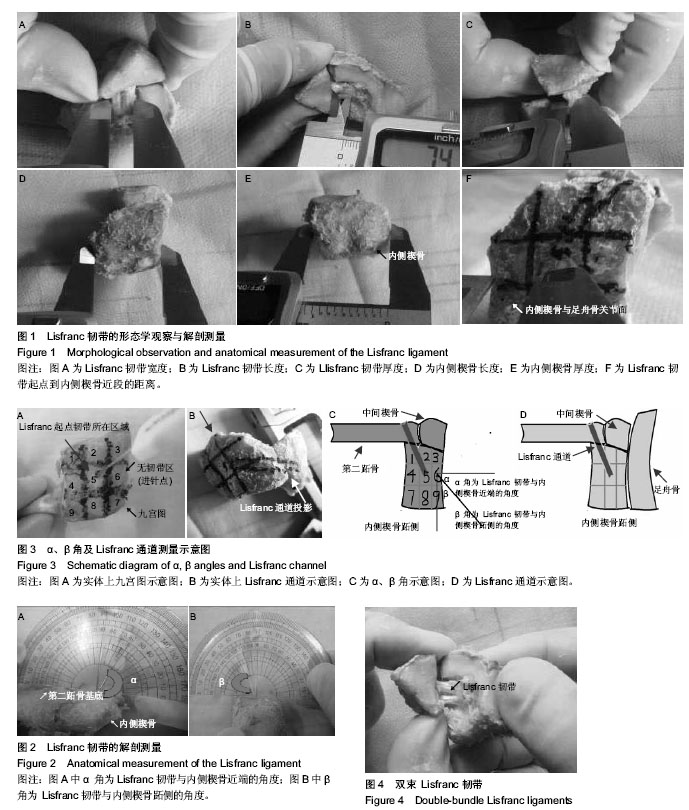
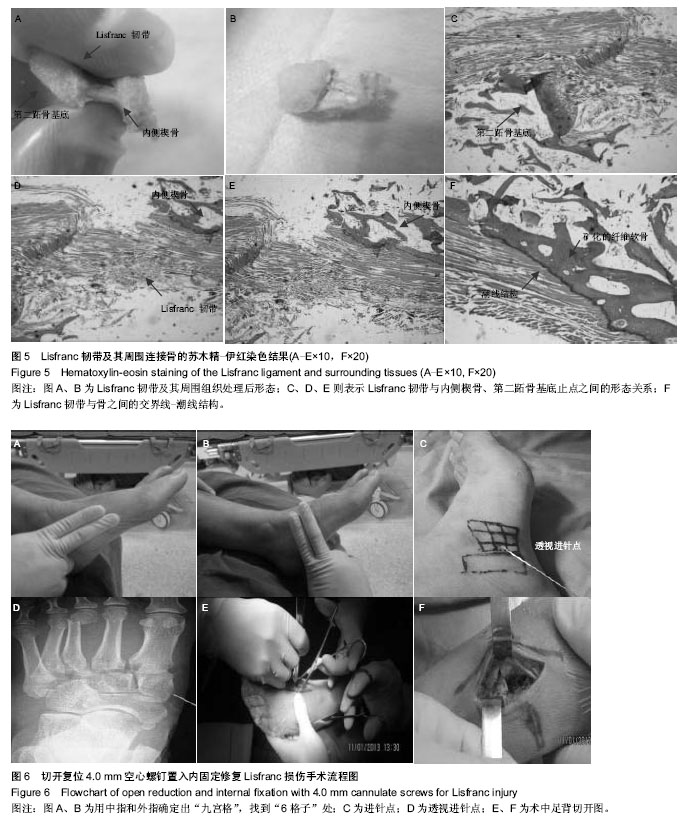
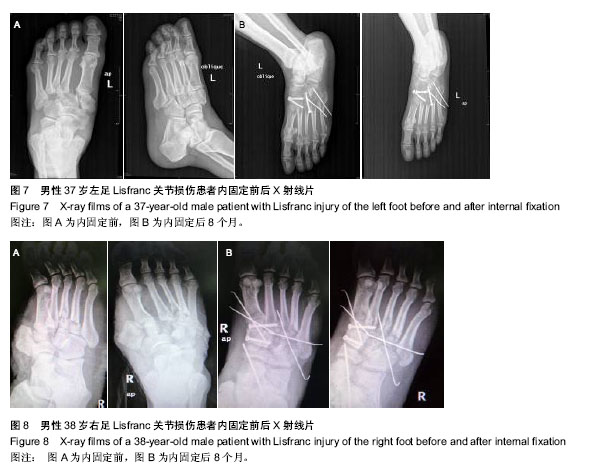
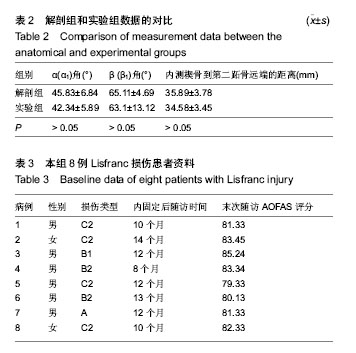
方法:①对18侧成人尸体标本进行解剖,观察Lisfranc韧带的组织形态并进行测量,得到Lisfranc韧带的详细形态参数,作为解剖组,确定Lisfranc韧带的走行和骨性标志;其余14侧成人尸体标本按以上参数用导针固定得出相应Lisfranc韧带相关数据,作为实验组,对比两组测量角度与内侧楔骨到第二跖骨基底长度。②对8例临床上确认的Lisfranc 损伤患者应用解剖学获得的参数和定位法行切开复位螺钉置入内固定治疗,内固定后随访8-14个月,采用美国足踝外科学会踝-后足评分进行功能评估。
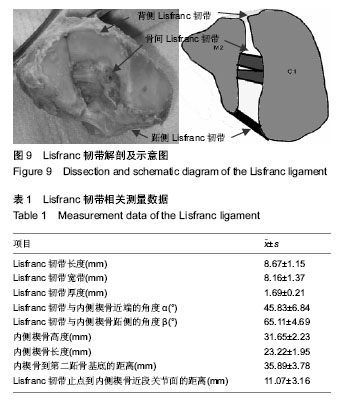
结果与结论:①通过解剖观察得出,解剖出的Lisfranc韧带均为2束。解剖组及实验组形态学测量结果比较差异无显著性意义(P > 0.05)。为了方便临床应用,作者提出“Lisfranc通道”这一概念,将Lisfranc通道定义为内侧楔骨(无韧带区)到第二跖骨基底部长(31.65±2.23) mm、宽(8.16±1.37) mm、高(1.69±0.21) mm、与内侧楔骨近端成(45.83±6.84)°角、与内侧楔骨跖侧成(65.11±4.69)°角的一条通道。通过做苏木精-伊红染色后,了解到Lisfranc韧带与周围组织的组织学特性:从层次上分为Lisfranc肌腱、潮线、矿化纤维软骨、骨等4层结构。②8例Lisfranc损伤患者应用解剖学获得的参数和定位法进行切开复位内固定后均获得较高的美国足踝外科学会踝-后足评分,为(80.30±4.85)分。解剖实验获得了Lisfranc关节及韧带详细的形态学参数,为该部位修复提供了解剖学资料,避免盲目置入内固定物,造成Lisfranc韧带起点的损伤,影响Lisfranc韧带修复效果。
中图分类号: