[1] RAHMATI M, MILLS DK, URBANSKA AM,
et al. Electrospinning for tissue engineering applications. Progress Mater Sci. 2021;117: 100721.
[2] GUO L, LIANG Z, YANG L, et al. The role of natural polymers in bone tissue engineering. J Control Release. 2021;338:571-582.
[3] LI Q, CHANG B, DONG H, et al. Functional microspheres for tissue regeneration. Bioact Mater. 2023;25:485-499.
[4] GONG M, SUN J, LIU G, et al. Graphene oxide‑modified 3D acellular cartilage extracellular matrix scaffold for cartilage regeneration. Mater Sci Eng C Mater Biol Appl. 2021:119:111603.
[5] ZHANG X, CHEN X, HONG H, et al. Decellularized extracellular matrix scaffolds: Recent trends and emerging strategies in tissue engineering. Bioact Mater. 2022;10: 15-31.
[6] MOUSAVI MS, AMOABEDINY G, MAHFOUZI SH, et al. Enhanced articular cartilage decellularization using a novel perfusion-based bioreactor method. J Mech Behav Biomed Mater. 2021:119:104511.
[7] COLLINS MN, REN G, YOUNG K, et al. Scaffold Fabrication Technologies and Structure/Function Properties in Bone Tissue Engineering. Adv Funct Mater. 2021; 31(21):2010609.
[8] BROWN M, LI J, MORAES C, et al. Decellularized extracellular matrix: New promising and challenging biomaterials for regenerative medicine. Biomaterials. 2022; 289:121786.
[9] BILODEAU C, SHOJAIE S, GOLTSIS O, et al. TP63 basal cells are indispensable during endoderm differentiation into proximal airway cells on acellular lung scaffolds. NPJ Regen Med. 2021;6(1):12.
[10] TALLAPANENI V, KALAIVANI C, PAMU D, et al. Acellular Scaffolds as Innovative Biomaterial Platforms for the Management of Diabetic Wounds. Tissue Eng Regen Med. 2021;18(5):713-734.
[11] GOLEBIOWSKA AA, INTRAVAIA JT, SATHE VM, et al. Decellularized extracellular matrix biomaterials for regenerative therapies: Advances, challenges and clinical prospects. Bioact Mater. 2024;32:98-123.
[12] MAHARA A, KOJIMA K, YAMAMOTO M, et al. Accelerated tissue regeneration in decellularized vascular grafts with a patterned pore structure. J Mater Chem B. 2022;10(14):2544-2550.
[13] MENG H, LIU X, LIU R, et al. Decellularized laser micro-patterned osteochondral implants exhibit zonal recellularization and self-fixing for osteochondral regeneration in a goat model. J Orthop Translat. 2024:46: 18-32.
[14] ZHANG Y, FENG G, XU G, et al. Microporous acellular extracellular matrix combined with adipose-derived stem cell sheets as a promising tissue patch promoting articular cartilage regeneration and interface integration. Cytotherapy. 2019;21(8):856-869.
[15] DASKALOVA A, ANGELOVA LJI. Ultra‑short laser patterning of silk fibroin thin films–a potential scaffold platform in tissue engineering applications. Industry 4.0. 2022;7(1):14-17.
[16] NüRNBERGER S, SCHNEIDER C, KEIBL C,
et al. Repopulation of decellularised articular cartilage by laser-based matrix engraving. EBioMedicine. 2021;64:103196.
[17] MOON HI, KIM S, BYUN JE, et al. Facile and rapid fabrication of wearable biosensors via femtosecond laser-directed micro-patterning with large-sized reduced graphene oxide for physiological monitoring. Chem Eng J. 2024;479:147819.
[18] NASIM H, JAMIL Y. Diode lasers: From laboratory to industry. Optics Laser Technol. 2014;56:211-222.
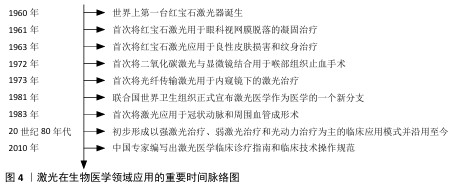
[19] 吕磊,张正厚,隋丽云,等.激光在医学基础和临床研究中的应用[J].中国临床康复,2006,10(17):152-154.
[20] GOLDMAN L, BLANEY DJ, KINDEL DJ, et al. Pathology of the effect of the laser beam on the skin. Nature. 1963:197:912-914.
[21] JAKO GJ. Laser surgery of the vocal cords an experimental study with carbon dioxide lasers on dogs. Laryngoscope. 1972;82(12): 2204-2216.
[22] NATH G, GORISCH W, KIEFHABER PJE. First laser endoscopy via a fiberoptic transmission system. Endoscopy. 1973;5(4):208-213.
[23] 邱海霞,顾瑛.激光医学研究生培养方法初探[J].中国激光医学杂志,2017,26(4): 221-224.
[24] 盖晓波,周形海.激光血管成形术研究近况[J].解放军医学杂志,1987(6):463-465.
[25] 顾瑛.激光医学[J].物理,2010,39(8): 515-521.
[26] KHALKHAL E, REZAEI-TAVIRANI M, ZALI MR, et al. The Evaluation of Laser Application in Surgery: A Review Article. J Lasers Med Sci. 2019;10(Suppl 1):S104-S111.
[27] STEINER R. Laser-Tissue Interactions//RAULIN C, KARSAI S. Laser and IPL Technology in Dermatology and Aesthetic Medicine. Berlin, Heidelberg; Springer Berlin Heidelberg. 2011:23-36.
[28] LECARPENTIER GL, MOTAMEDI M, MCMATH LP, et al. Continuous wave laser ablation of tissue: analysis of thermal and mechanical events. IEEE Trans Biomed Eng. 1993;40(2):188-200.
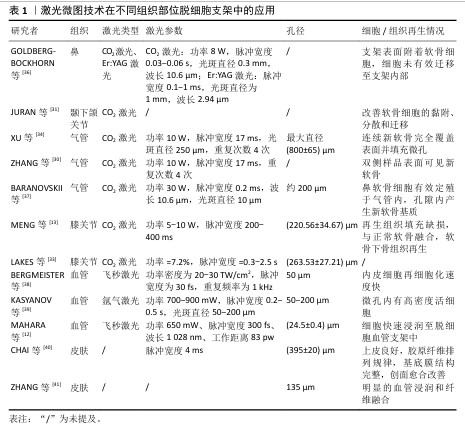
[29] LI Y, XU Y, LIU Y, et al. Decellularized cartilage matrix scaffolds with laser-machined micropores for cartilage regeneration and articular cartilage repair. Mater Sci Eng C Mater Biol Appl. 2019;105:110139.
[30] ZHANG Y, XU Y, LIU Y, et al. Porous decellularized trachea scaffold prepared by a laser micropore technique. J Mech Behav Biomed Mater. 2019;90:96-103.
[31] JURAN CM, DOLWICK MF, MCFETRIDGE PS. Engineered Microporosity: Enhancing the Early Regenerative Potential of Decellularized Temporomandibular Joint Discs. Tissue Eng Part A. 2015;21(3-4): 829-839.
[32] MURPHY CM, HAUGHG, O’BRIEN FJ. The effect of mean pore size on cell attachment, proliferation and migration in collagen–glycosaminoglycan scaffolds for bone tissue engineering. Biomaterials. 2010;31(3): 461-466.
[33] LAKES EH, MATUSKA AM, MCFETRIDGE PS, et al. Mechanical Integrity of a Decellularized and Laser Drilled Medial Meniscus. J Biomech Eng. 2016;138(3): 4032381.
[34] XU Y, LI D, YIN Z, et al. Tissue-engineered trachea regeneration using decellularized trachea matrix treated with laser micropore technique. Acta Biomater. 2017;58:113-121.
[35] MATUSKA AM, MCFETRIDGE PS. Laser micro-ablation of fibrocartilage tissue: Effects of tissue processing on porosity modification and mechanics. J Biomed Mater Res B Appl Biomater. 2018;106(5): 1858-1868.
[36] GOLDBERG-BOCKHORN E, SCHWARZ S, SUBEDI R, et al. Laser surface modification of decellularized extracellular cartilage matrix for cartilage tissue engineering. Lasers Med Sci. 2018;33(2):375-384.
[37] BARANOVSKII D, DEMNER J, NÜRNBERGER S, et al. Engineering of Tracheal Grafts Based on Recellularization of Laser-Engraved Human Airway Cartilage Substrates. Cartilage. 2022;13(1):19476035221075951.
[38] BERGMEISTER H, BOECK P, KASIMIR MT, et al. Effect of laser perforation on the remodeling of acellular matrix grafts . J Biomed Mater Res B Appl Biomater. 2005; 74B(1):495-503.
[39] KASYANOV VA, HODDE J, HILES MC, et al.
Rapid biofabrication of tubular tissue constructs by centrifugal casting in a decellularized natural scaffold with laser-machined micropores. J Mater Sci Mater Med. 2009;20(1):329-337.
[40] CHAI JK, LIANG LM, YANG HM, et al. Preparation of laser micropore porcine acellular dermal matrix for skin graft: An experimental study. Burns. 2007;33(6): 719-725.
[41] ZHANG Y, ZENG Y, XIN G, et al. Biological function evaluation and effects of laser micro-pore burn-denatured acellular dermal matrix. Burns. 2018;44(2):350-358.
[42] LAVERNIA L, BROWN WE, WONG BJF, et al.
Toward tissue-engineering of nasal cartilages. Acta Biomater. 2019;88:42-56.
[43] BROWN WE, LAVERNIA L, BIELAJEW BJ, et al. Human nasal cartilage: Functional properties and structure-function relationships for the development of tissue engineering design criteria. Acta Biomater. 2023;168:113-124.
[44] FARAHANI PK. Application of Tissue Engineering and Biomaterials in Nose Surgery. JPRAS Open. 2024;40:262-272.
[45] GEMINI L, AL-BOURGOL S, MACHINET G,
et al. Ablation of Bone Tissue by Femtosecond Laser: A Path to High-Resolution Bone Surgery. Materials. 2021;14(9):2429.
[46] MOSHIRFAR M, MEGERDICHIAN A, WEST WB, et al. Comparison of Visual Outcome After Hyperopic LASIK Using a Wavefront-Optimized Platform Versus Other Excimer Lasers in the Past Two Decades. Ophthalmol Ther. 2021;10(3):547-563.
[47] JABBOUR S, BOWER KS. Refractive Surgery in the US in 2021. JAMA. 2021;326(1):77-78.
[48] TIAN K, XIANG M, WEN X, et al. Tissue Ablation with Multi-Millimeter Depth and Cellular-Scale Collateral Damage by a Femtosecond Mid-Infrared Laser Tuned to the Amide-I Vibration. Laser Photonics Rev. 2024;18(2):2300421.
[49] LU K, MA F, YI D, et al. Molecular signaling in temporomandibular joint osteoarthritis. J Orthop Translat. 2022;32:21-27.
[50] WHYTE A, BOEDDINGHAUS R, BARTLEY A,
et al. Imaging of the temporomandibular joint. Clin Radiol. 2021;76(1):76.e21-76.e35.
[51] RAVINDRA A, D’ANGELO W, ZHANG L, et al. Human Bronchial Epithelial Cell Growth on Homologous Versus Heterologous Tissue Extracellular Matrix. J Surg Res. 2021;263: 215-223.
[52] HUO Y, XU Y, WU X, et al. Functional Trachea Reconstruction Using 3D-Bioprinted Native-Like Tissue Architecture Based on Designable Tissue-Specific Bioinks. Adv Sci. 2022;9(29):2202181.
[53] ZHANG B, SUN F, LU Y, et al. A novel decellularized trachea preparation method for the rapid construction of a functional tissue engineered trachea to repair tracheal defects. J Mater Chem B. 2022;10(25): 4810-4822.
[54] XU Y, LI Y, LIU Y, et al. Surface modification of decellularized trachea matrix with collagen and laser micropore technique to promote cartilage regeneration. Am J Transl Res. 2019; 11(9):5390-5403.
[55] DHASMANA A, SINGH A, RAWAL S. Biomedical grafts for tracheal tissue repairing and regeneration “Tracheal tissue engineering: an overview”. Tissue Eng Regen Med. 2020;14(5):653-672.
[56] JIANG S, TIAN G, YANG Z, et al. Enhancement of acellular cartilage matrix scaffold by Wharton’s jelly mesenchymal stem cell-derived exosomes to promote osteochondral regeneration. Bioact Mater. 2021;6(9):2711-2728.
[57] ZHANG JY, XIANG XN, YU X, et al. Mechanisms and applications of the regenerative capacity of platelets-based therapy in knee osteoarthritis. Biomed Pharmacother. 2024:178:117226.
[58] JIA L, ZHANG P, CI Z, et al. Acellular cartilage matrix biomimetic scaffold with immediate enrichment of autologous bone marrow mononuclear cells to repair articular cartilage defects. Mater Today Bio. 2022:15:100310.
[59] 刘雪剑,刘士臣,孙百川,等.激光微孔化脱细胞骨软骨支架的制备及表征[J].中国组织工程研究,2018,22(18):2836-2842.
[60] FORD TJ, ONG P, SECHTEM U, et al. Assessment of Vascular Dysfunction in Patients Without Obstructive Coronary Artery Disease. JACC Cardiovasc Interv. 2020;13(16):1847-1864.
[61] ILANLOU S, KHAKBIZ M, AMOABEDINY G, et al. Preclinical studies of acellular extracellular matrices as small-caliber vascular grafts. Tissue Cell. 2019;60:25-32.
[62] WANG X, CHAN V, CORRIDON PR. Decellularized blood vessel development: Current state-of-the-art and future directions. Front Bioeng Biotechnol. 2022; 10:951644.
[63] WANG X, CHAN V, CORRIDON PR. Acellular Tissue-Engineered Vascular Grafts from Polymers: Methods, Achievements, Characterization, and Challenges. Polymers. 2022;14(22):4825.
[64] BOCK N, PHAM LB, NGUYEN TB, et al. Polydopamine coating of uncrosslinked chitosan as an acellular scaffold for full thickness skin grafts. Carbohydr Polym. 2020;245:116524.
[65] YU G, YE L, TAN W, et al. A novel dermal matrix generated from burned skin as a promising substitute for deep‑degree burns therapy. Mol Med Rep. 2016;13(3):2570-2582. |