中国组织工程研究 ›› 2024, Vol. 28 ›› Issue (30): 4757-4762.doi: 10.12307/2024.635
• 骨与关节生物力学 bone and joint biomechanics • 下一篇
腓骨近端骨折对伸直状态下膝关节应力影响的有限元分析
汪嘉琪1,唐江安2,黄国华2,孔德策2,赵一丁2,龚璐璐3,潘红元1,孔德伟1,刘 粤2,杨铁毅2
- 1宁夏医科大学上海市浦东新区公利医院研究生培养基地,上海市 200135;2上海市浦东新区公利医院骨科,上海市 200135;3同济大学生命科学与技术学院,上海市 200092
Finite element analysis of effect of proximal fibular fracture on knee joint stress in an extended state
Wang Jiaqi1, Tang Jiangan2, Huang Guohua2, Kong Dece2, Zhao Yiding2, Gong Lulu3, Pan Hongyuan1, Kong Dewei1, Liu Yue2, Yang Tieyi2
- 1Shanghai Pudong New Area Gongli Hospital Postgraduate Training Base, Ningxia Medical University, Shanghai 200135, China; 2Department of Orthopedics, Shanghai Pudong New Area Gongli Hospital, Shanghai 200135, China; 3College of Life Science and Technology, Tongji University, Shanghai 200092, China
摘要:
文题释义:
腓骨骨折:大多数腓骨近端骨折常与胫骨上端或胫骨干骨折合并发生,此类损伤通常为高能量损伤,常合并韧带、半月板等软组织损伤,术后合并症较多,诸如胫骨平台关节面塌陷、膝关节不稳、膝关节内外翻等等情况,导致复杂胫骨平台骨折的治疗效果不佳。此类骨折因为靠近膝关节,固定有争议且较为困难,易并发关节强直、关节不稳等并发症。有限元分析:最初广泛运用于工程力学研究。20世纪70年代初,随着科学技术的发展,它第一次被用来研究骨科生物力学,近年来,有限元分析发展成为分析骨科力学变化极为有用的工具,推动了骨科仿真生物力学试验的发展。
背景:传统观点认为绝大多数的腓骨近端骨折是不需要固定的,他人和此次研究提示,近端腓骨结构对于膝关节后外侧结构的稳定性具有重要影响,其作用机制值得研究。
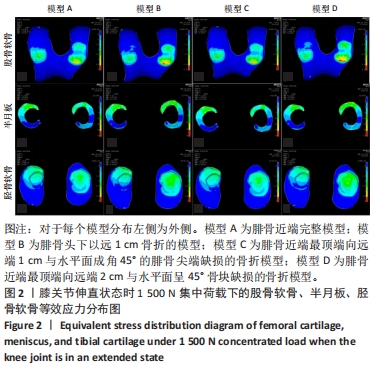
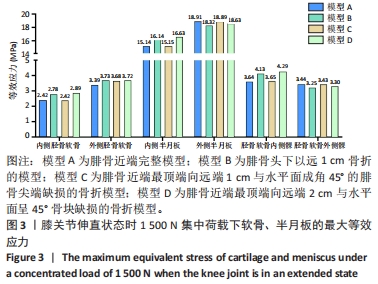
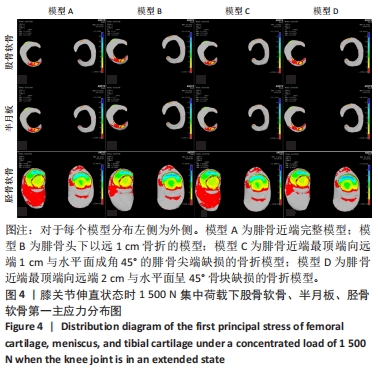
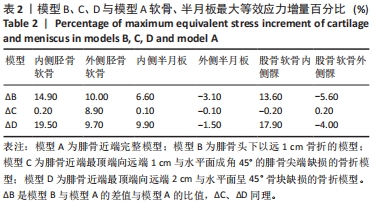
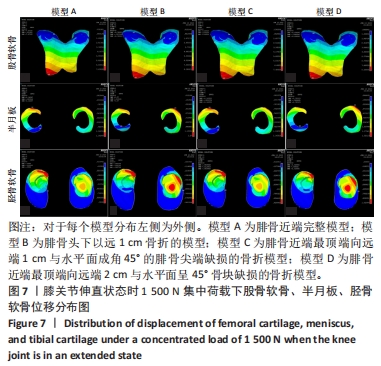
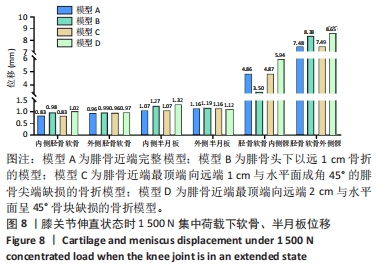
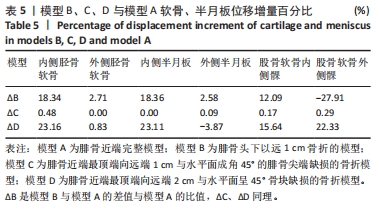
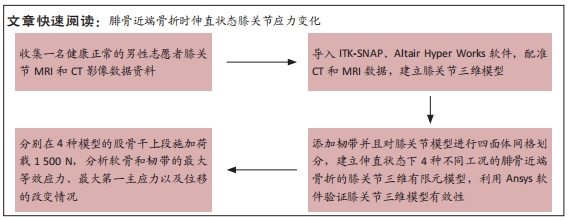
目的:探讨腓骨近端骨折对于伸直状态膝关节各结构生物力学的影响。方法:运用有限元方法进行仿真生物力学试验。选用1名健康青年男性志愿者膝关节MRI和CT影像数据资料建立伸直状态下的膝关节有限元模型,并模拟4种近端腓骨形态:模型A为完整模型,模型B为腓骨头下以远1 cm骨折模型,模型C为腓骨近端最顶端向远端1 cm的尖端缺损骨折模型,模型D为腓骨近端最顶端向远端2 cm的骨缺损模型。在股骨干上施加纵向集中载荷1 500 N,对比分析膝关节伸直状态下,4种工况下膝关节各个结构最大等效应力、最大第一主应力的分布以及改变趋势。
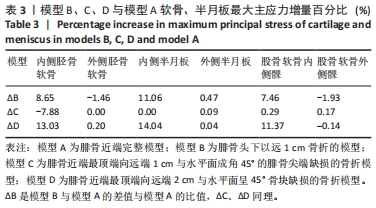
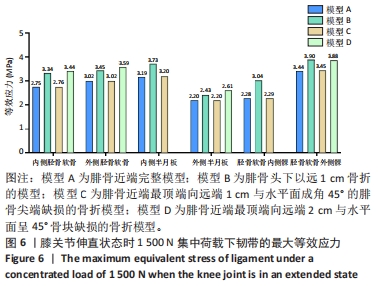
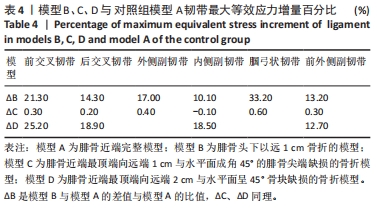
结果与结论:①模型A胫骨软骨、半月板外侧室最大等效应力大于内侧;胫骨平台、半月板内侧室最大第一主应力大于外侧;股骨软骨内侧髁最大等效应力大于外侧髁,股骨软骨内侧髁最大第一主应力大于内侧髁;②相较于模型A,模型C的软骨、半月板的最大等效应力和最大第一主应力大小以及分布情况无明显差异;③相较于模型A,模型B的最大等效应力上升幅度依次为内侧胫骨软骨(14.9%),股骨软骨内侧髁(13.6%),内侧半月板(6.6%);最大第一主应力上升幅度依次为内侧半月板(11.06%),内侧胫骨软骨(8.65%),股骨软骨内侧髁(7.46%);韧带的最大等效应力上升幅度依次为:腘弓状韧带(33.2%) >前交叉韧带(21.3%) >腓侧副韧带(17%) >后交叉韧带(14.3%) >前外侧副韧带(13.2%) >内侧副韧带(10.1%);④相较于模型A,模型D的最大等效应力上升趋势依次为内侧胫骨软骨(19.5%),股骨软骨内侧髁(17.9%),内侧半月板(9.9%);最大第一主应力依次为内侧半月板(14.04%),内侧胫骨软骨(13.03%),股骨软骨内侧髁(11.37%);韧带最大等效应力上升趋势依次为:前交叉韧带(25.2%) >后交叉韧带(18.9%) >内侧副韧带(18.5%) >前外侧副韧带(12.7%);⑤提示在膝关节伸直情况下,腓骨头下1 cm骨折和2 cm腓骨尖端骨缺损对内侧室软骨、前交叉韧带以及后外侧韧带复合体结构的影响较大。
https://orcid.org/0009-0006-5196-8814 (汪嘉琪)
中国组织工程研究杂志出版内容重点:人工关节;骨植入物;脊柱;骨折;内固定;数字化骨科;组织工程
中图分类号: