[1] CARON T, BRANSFORD R, NGUYEN Q, et al. Spine fractures in patients with ankylosing spinal disorders. Spine (Phila Pa 1976). 2010;35(11):458-464.
[2] TAN S, YAO JH, FLYNN JA, et al. Zygapophyseal Joint Fusion in Ankylosing Spondylitis Assessed by Computed Tomography: Associations with Syndesmophytes and Spinal Motion. J Rheumatol. 2017;44(7):1004-1010.
[3] MARTINDALE J, SHUKLA R, GOODACRE J. The impact of ankylosing spondylitis/axial spondyloarthritis on work productivity. Best Pract Res Clin Rheumatol. 2015;29(3): 512-523.
[4] PRAY C, FEROZ NI, HAROON NN. Bone Mineral Density and Fracture Risk in Ankylosing Spondylitis: A Meta-Analysis. Calcif Tissue Int. 2017;101(2):182-192.
[5] MIN Y, HUI-YUN G, HOU-CHENG Z, et al. The surgical treatment strategies for thoracolumbar spine fractures with ankylosing spondylitis: a case report. BMC Surg. 2019;19(1):99.
[6] REINHOLD M, KNOP C, KNEITZ C, et al. Spine Fractures in Ankylosing Diseases: Recommendations of the Spine Section of the German Society for Orthopaedics and Trauma (DGOU). Global Spine J. 2018;8(2 Suppl):56-68.
[7] SHEN FH, SAMARTZIS D. Surgical management of lower cervical spine fracture in ankylosing spondylitis. J Trauma. 2006;61(4):1005-1009.
[8] LINDTNER RA, KAMMERLANDER C, GOETZEN M, et al. Fracture reduction by postoperative mobilisation for the treatment of hyperextension injuries of the thoracolumbar spine in patients with ankylosing spinal disorders. Arch Orthop Trauma Surg. 2017;137(4):531-541.
[9] RUSTAGI T, DRAZIN D, ONER C, et al. Fractures in Spinal Ankylosing Disorders: A Narrative Review of Disease and Injury Types, Treatment Techniques, and Outcomes. J Orthop Trauma. 2017;31(Suppl 4):57-74.
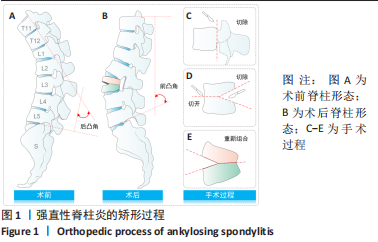
[10] DEBARGE R, DEMEY G, ROUSSOULY P. Radiological analysis of ankylosing spondylitis patients with severe kyphosis before and after pedicle subtraction osteotomy. Eur Spine J. 2010;19(1):65-70.
[11] QIAN BP, WANG XH, QIU Y, et al. The influence of closing-opening wedge osteotomy on sagittal balance in thoracolumbar kyphosis secondary to ankylosing spondylitis: a comparison with closing wedge osteotomy. Spine (Phila Pa 1976). 2012;37(16): 1415-1423.
[12] DEBARGE R, DEMEY G. ROUSSOULY P. Sagittal balance analysis after pedicle subtraction osteotomy in ankylosing spondylitis. Eur Spine J. 2011;20(Suppl 5):619-625.
[13] BESS S, HARRIS JE, TURNER AW, et al. The effect of posterior polyester tethers on the biomechanics of proximal junctional kyphosis: a finite element analysis. J Neurosurg Spine. 2017;26(1):125-133.
[14] CAHILL PJ, WANG W, ASGHAR J, et al. The Use of a Transition Rod May Prevent Proximal Junctional Kyphosis in the Thoracic Spine Following Scoliosis Surgery: A Finite Element Analysis. Spine (Phila Pa 1976). 2012;37(12):687-695.
[15] PEI B, LU D, WU X, et al. Effects of Growing Rod Technique with Different Surgical Modes and Growth Phases on the Treatment Outcome of Early Onset Scoliosis: A 3-D Finite Element Analysis. Int J Environ Res Public Health. 2022;19(4):2057.
[16] PEI B, LU D, WU X, et al. Kinematic and biomechanical responses of the spine to distraction surgery in children with early onset scoliosis: A 3-D finite element analysis. Front Bioeng Biotechnol. 2017;10:933341.
[17] LIU Y, WANG Z, LIU M, et al. Biomechanical influence of the surgical approaches, implant length and density in stabilizing ankylosing spondylitis cervical spine fracture. Sci Rep. 2021;11(1):6023.
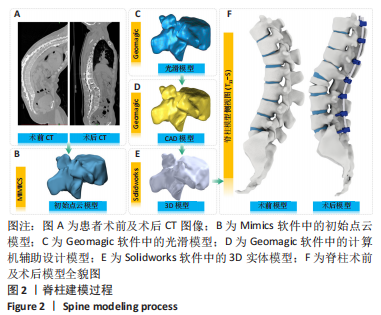
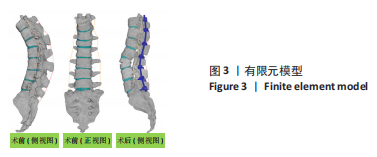
[18] MUHEREMU A, LI H, MA JY, et al. Establishment of a three-dimensional finite element model of severe kyphotic deformity secondary to ankylosing spondylitis. J Int Med Res. 2017;45(2):639-646.
[19] ZHANG TY, WANG YH, ZHANG PX, et al. Different fixation pattern for thoracolumbar fracture of ankylosing spondylitis: A finite element analysis. PloS One. 2021;16(4): e0250009.
[20] ROBINSON Y, LISON ALMKVIST V, OLERUD C, et al. Finite Element Analysis of Long Posterior Transpedicular Instrumentation for Cervicothoracic Fractures Related to Ankylosing Spondylitis. Global Spine J. 2018;8(6):570-578.
[21] 马涌, 斯刊达尔斯依提, 欧勇, 等. 不同截骨方式修复强直性脊柱炎后凸畸形的有限元分析[J]. 中国组织工程研究,2017,21(19):3038-3043.
[22] 李辉, 张鹏, 尚俊, 等. 去松质骨截骨术与全脊柱截骨术治疗强直性脊柱炎后凸畸形有限元分析[J]. 山西医科大学学报,2019,50(3):368-372.
[23] TONG Z, XIAO B, YAN K, et al. Biomechanical Evaluation of the Transcortical and Transpedicular Trajectories for Pedicle Screw Insertion in Thoracolumbar Fracture Fixation for Ankylosing Spondylitis. Front Surg. 2021;8:706597.
[24] NIGIL HAROON N, SZABO E, RABOUD JM, et al. Alterations of bone mineral density, bone microarchitecture and strength in patients with ankylosing spondylitis: a cross-sectional study using high-resolution peripheral quantitative computerized tomography and finite element analysis. Arthritis Res Ther. 2015;17:37.
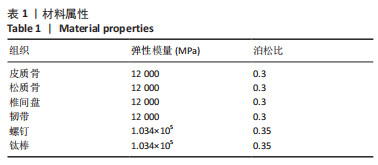
[25] FINLEY SM, BRODKE DS, SPINA NT, et al. FEBio finite element models of the human lumbar spine. Comput. Methods Biomech Biomed Eng. 2018;21(6):444-452.
[26] WANG JL, PARNIANPOUR M, SHIRAZI-ADL A, et al. Viscoelastic finite-element analysis of a lumbar motion segment in combined compression and sagittal flexion. Spine (Phila Pa 1976). 2000;25(3):310-318.
[27] BURSTEIN AH, REILLY DT, MARTENS M. Aging of bone tissue: mechanical properties. J Bone Joint Surg Am. 1976;58(1):82-86.
[28] SHIRAZI-ADL SA, SHRIVASTAVA SC, AHMED AM. Stress Analysis of the Lumbar Disc-Body Unit in Compression A Three-Dimensional Nonlinear Finite Element Study. Spine (Phila Pa 1976). 1984;9(2):120-134.
[29] KURUTZ M, OROSZVÁRY L. Finite element analysis of weightbath hydrotraction treatment of degenerated lumbar spine segments in elastic phase J. Biomech. 2010;43(3):433-441.
[30] CAI XY, SANG DC, YUCHI CX, et al. Using finite element analysis to determine effects of the motion loading method on facet joint forces after cervical disc degeneration. Comput Biol Med. 2020;116:103519.
[31] AGAWAL A, ZAKERI A, AGARWAL AK, et al. Distraction magnitude and frequency affects the outcome in juvenile idiopathic patients with growing rods: Finite element study using a representative scoliotic spine model. Spine J. 2015;15(8):1848-1855.
[32] WHITE AAI, PANJABI MM. Clinical Biomechanics of the Spine. Lippincott-Raven,1992.
[33] MATSUKAWA K, YATO Y, IMABAYASHI H, et al. Biomechanical evaluation of the fixation strength of lumbar pedicle screws using cortical bone trajectory: a finite element study. J Neurosurg Spine. 2015;23(4):471-478.
[34] WERNER BC, SAMARTZIS D, SHEN FH. Spinal fractures in patients with ankylosing spondylitis: etiology, diagnosis, and management. J Am Acad Orthop Surg. 2016; 24(4):241-249.
[35] LEONE A, MARINO M, DELLATTI C, et al. Spinal fractures in patients with ankylosing spondylitis. Rheumatol Int. 2016;36(10):1335-1346.
[36] CHARLES YP, BUY X, GANGI A, et al Fracture in ankylosing spondylitis after minor trauma: radiological pitfalls and treatment by percutaneous instrumentation. A case report. Orthop Traumatol Surg Res. 2013;99(1):115-119.
[37] WESTERVELD LA, VERLAAN JJ, ONER FC. Spinal fractures in patients with ankylosing spinal disorders: a systematic review of the literature on treatment, neurological status and complications. Eur Spine J. 2009;18(2):145-156.
[38] 李民, 周灵, 汪桂珍, 等. 不同腰椎生理曲度下牵引的三维有限元分析[J]. 中国组织工程研究,2020,24(20):3162-3167.
[39] YAMAMOTO I, PANJABI M, CRISCO T, et al. Three-dimensional movements of the whole lumbar spine. Spine. 1989;14(1):1256-1260.
[40] XIAO Z, WANG L, GONG H, et al. Biomechanical evaluation of three surgical scenarios of posterior lumbar interbody fusion by finite element analysis. Biomed Eng Online. 2012;11(1):31.
[41] Agarwal A, Kodigudla M, Kelkar A, et al. Towards a validated patient-specific computational modeling framework to identify failure regions in traditional growing rods in patients with early onset scoliosis. N Am Spine Soc J. 2021;5(5):100043.
[42] 李辉. 强直性脊柱炎后凸矫形生物力学研究和临床疗效分析[D]. 乌鲁木齐: 新疆医科大学.2017. |