Chinese Journal of Tissue Engineering Research ›› 2021, Vol. 25 ›› Issue (33): 5388-5394.doi: 10.12307/2021.332
Previous Articles Next Articles
Clinical application and progress of computer assisted navigation system in total knee arthroplasty
Zhang Tao1, Liang Chunyu2, Zhang Dingding1, Bai Xiaosong1, Shen Xiaoyang1
- 1Affiliated Hospital of North China University of Science and Technology, Tangshan 063000, Hebei Province, China; 2North China University of Science and Technology, Tangshan 063000, Hebei Province, China
-
Received:2020-12-17Revised:2020-12-30Accepted:2021-02-22Online:2021-11-28Published:2021-08-06 -
Contact:Liang Chunyu, Master, Chief physician, North China University of Science and Technology, Tangshan 063000, Hebei Province, China -
About author:Zhang Tao, Physician, Affiliated Hospital of North China University of Science and Technology, Tangshan 063000, Hebei Province, China
CLC Number:
Cite this article
Zhang Tao, Liang Chunyu, Zhang Dingding, Bai Xiaosong, Shen Xiaoyang. Clinical application and progress of computer assisted navigation system in total knee arthroplasty[J]. Chinese Journal of Tissue Engineering Research, 2021, 25(33): 5388-5394.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
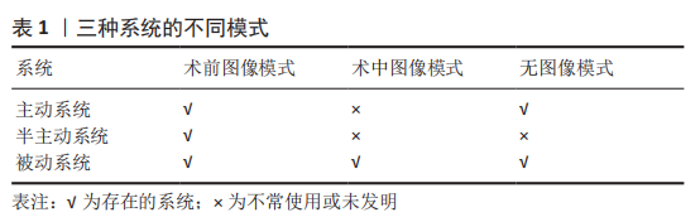
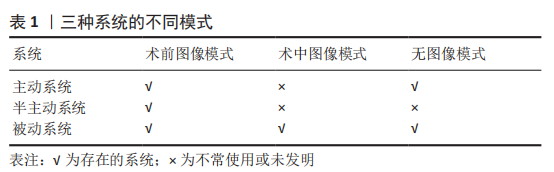
2.1 计算机辅助的分类 计算机辅助手术于20世纪90年代末以被动导航系统的形式被引入[10],1997年进行了第一次计算机辅助TKA术[11]。计算机辅助详细分为3种系统和3种模式[12-13]。3种系统分为:①主动即机器人工具,在没有外科医生直接干预的情况下执行手术任务;②半主动即是受控的机器人工具,系统在预定的框架内限制任务;③被动是形成外科手术的某些部分,但在外科医生的直接指导或控制下进行操作,导航就是这个类别的一部分。3种模式分为:①术前成像方式包括使用图像方式的三维结构,如CT、MRI、US或2D/3D透视技术;②术中成像方式包括使用MRI、CT或更常见的透视,特别是脊柱导航手术;③无图像模式不同于上述两种模式,该技术不需要任何图像模式,无论是术前或术中,依靠手术部位的解剖标志以创建患者特有的模型,这种方式是最常用于膝关节导航。见表1。 CANS被广义分为3类:基于图像的大型操作台、无图像的大型操作台和手持式导航系统[14]。基于图像导航系统依靠术前CT和/或MRI的影像资料提供关节的表面的立体定位配准和整体对齐;无图像的导航系统依靠术中注册关键的解剖标记及关节运动中心,计算机实时显示截骨高度、角度、力线及间隙信息,提供截骨规划及假体选择;而基于手持式加速度计导航系统则去除了大型操作台及显示器,是近些年新研究出的导航系统。B?THIS等[15]研究显示基于图像组(60/65)和无图像组(63/65)的患者,膝内翻/外翻在3°内,股骨和胫骨复合体在内翻/外翻方向无明显差异。基于图像的技术,可以减少TKA住院并发症和输血,而不会显著增加住院费用和住院时间[16]。 2.2 CANS的优势 随着计算机辅助及导航系统的不断发展,在TKA中应用越来越多。从2005到2011年,计算机辅助膝关节置换的比例每年增加23.13%[16]。澳大利亚关节登记数据显示,55岁以下应用导航技术进行TKA的患者从2003年的2.4%增加到2015年的28.6%,并降低了翻修率[17]。 ANTONIOS 等[18]发现美国在2005至2014年期间有6 060 901 例接受TKA的患者,其中273 922例(4.5%)使用计算机导航,24 084例(0.4%)使用机器人辅助,计算机导航的使用从2005年的1.2%增加到2014年的6.3%,同时在研究期间,计算机辅助从2005年的1.2%增至2014年的7.0%。 CANS较传统手术方式能提高下肢机械力线的准确度,使其良好的控制在±3°以内。ZHANG等[19]的研究显示,导航组冠状位股骨角、冠状位胫骨角、胫骨假体后倾角分别为(89.4±1.5)°,(89.3±1.4)°及(6.8±1.6)°,常规组分别为(87.3±3.8)°,(88.1±1.9)°及(10.9±4.6)°,理想角度为90°,90°及7°,发现统计学差异有显著性意义,所以CANS可以通过方便且准确的方法为膝关节骨性关节炎患者恢复下肢力线。TODESCA等[20]同样也表示导航组可以使患者TKA术后有良好的下肢力线和良好的置入定位精度,且差异有显著性意义。同时也有学者表明虽然CANS可以使下肢机械轴良好控制在±3°内,但是与常规手术差异不大,不会使患者满意度得到提升。HARVIE等[21]认为虽然计算机导航的TKA在组件对齐方面提供了更好的结果,但在术后5年内功能结果或患者满意度方面没有统计学上差异。CIP等[22]研究表示,导航组下肢机械轴精确更高,但是术后12年CANS组与常规组在假体存活率、置入准确性、临床结局及评分结果方面无差异。 CANS可以完成准确的截骨,并对伸屈间隙和软组织平衡有极大的帮助,也能完成良好的运动学分析和测量。因为导航通过系统计划精准地在股骨远端和胫骨近端进行切割,截骨后还可以进行验证,而伸屈间隙的水平主要是通过截骨来实现的。伸屈间隙的平衡是TKA术后良好临床结果的关键,传统手术是一个基于主观感觉的直观过程。FICKERT等[23]也表示计算机辅助TKA可以实现精确的间隙平衡,而间隙平衡不依赖于各种术前和术中因素,包括年龄、性别、术前畸形范围和骨关节炎等级,CANS计算并验证胫骨和股骨切割是影响伸屈间隙唯一的可能因素。CHIA等[24]通过测量置入后屈伸间隙,判断间隙差异的增加是否与不良的临床结果有关,得出平衡屈曲-伸展间隙差异≤2 mm在6个月时显示出良好的临床结果;软组织平衡在关节活动中起到重要作用,韧带过紧会造成屈曲畸形、活动范围缩小,韧带过松会使膝关节过伸、加速假体磨损。RITTER等[25]通过研究得出TKA术前屈曲挛缩程度越大术后越有可能发生屈曲挛缩,术后过伸超过10°也会导致疼痛增加、功能差。导航系统可以显示软组织情况,WADA等[26-27]的实验得出,导航组术后极少屈曲挛缩超过5°,没有过伸超过10°。CANS系统具有在术中完美开展运动学分析重现以及在整个运动范围内测量膝关节内翻或外翻对齐的能力。 传统手术股骨、胫骨截骨是通过髓内、外定位来决定的,股骨髓内定位会造成术中出血量增加,可能会出现栓子,术后形成下肢血栓的风险概率增加。与传统手术相比,导航并发症的发生可能更少,例如全身栓塞、失血、心脏事件等。有研究表明,导航辅助TKA的患者中,TKA术后24 h血浆D-二聚体水平明显降低[28]。JIANG等[29]回顾性研究了718例原发性单侧TKA或全髋关节置换的患者,探讨围术期同种异体输血与术后30 d内深静脉血栓的关系,得出输血与关节置换后深静脉血栓有显著相关性,接受输血的患者术后深静脉血栓的风险是未输血患者的4倍。LIODAKIS等[30]研究表明,在TKA中使用CANS可减少围术期输血。丹麦的一项全国性研究表明,TKA术后急性心肌梗死发病率增加,前2周风险增加了30.9倍[31]。KUO等[32]研究显示,导航组在TKA后24 h 收集的引流液中白细胞10水平明显低于常规TKA组(P < 0.01)。CANS TKA的优点是减少炎症标志物的产生,炎症标志物具有预测TKA术后主要并发症和功能恢复的潜力[33];另外导航TKA也可以减少内皮损伤标志物生成[34]。上述研究说明CANS能减少术中及术后并发症的产生,有利于患者预后及术后功能锻炼。 2.3 CANS术后随访 很多骨科医生因为使用CANS术后临床结果不太明显,甚至与传统手术方式无差异而不建议使用。LüTZNER等[35]在短期随访中发现(随访时间<20个月),膝关节协会评分、功能情况及健康状况导航组较常规组有所改善,但差异无显著性意义。DENTI等[36]表示两种技术之间没有明显的差异,导航组和传统组在机械排列和胫骨角度方面差异无显著性意义,两组术后1年以上的日常活动没有明显的差异,都比较满意。AYEKOLOYE等[37]利用Meta分析比较无图像计算机导航辅助TKA与传统手术方式,得出使用无图像计算机导航辅助进行中期随访的功能结果略有改善,总评分点估计为3.36,信任区间(-0.583,7.298);客观评分点估计为1.45,信任区间(0.11,2.799),功能评分点估计为2.4,信任区间(-1.174,5.977)。SONG等[38] 在TKA术后9年共对80例患者进行身体和放射学检查,使用美国特种外科医院评分、西安大略和麦克马斯特大学骨关节炎指数、膝关节协会评分中的功能和疼痛评分对临床结果进行评估,还评估了9年随访期间组件松动及其存活的放射性结果,显示导航辅助TKA比传统TKA方式产生了更好的对齐结果和更好的存活率,但差异无显著性意义;在长期随访中,临床结果在统计学上也是相似的。也有学者提出不同意见,PETURSSON等[39]采集172例患者在术后2年的临床评估结果,显示在膝关节损伤和骨关节炎结果评分中术后症状和日常活动、娱乐得到改善,在西安大略和麦克马斯特大学骨关节炎指数表中术后僵直有所改善,得出在TKA术后2年使用计算机导航患者的疼痛缓解和功能恢复情况优于用常规TKA手术组。MARTíN-HERNáNDEZ等[40]对119例使用导航治疗的患者和80例使用常规器械治疗的患者进行术后3年多中心前瞻性研究,所有患者均分析西安大略和麦克马斯特大学骨关节炎指数、膝关节协会评分以及放射学指标,得出随访期间所有患者临床评分均有改善,但导航组改善更明显。 BAUMBACH等[41]的10年随访结果显示,与传统TKA手术方式相比,导航组提供了显著降低的翻修率和最佳定位;而且使用导航进行TKA患者的疼痛比接受传统手术的患者轻,这表明导航与传统手术方式相比在患者满意度上有显著优势。不管是短期还是中、长期的随访,导航辅助TKA及传统TKA方式在临床及术后效果方面还是存在很大争议。由于一些文章样本量相对较少,得出的结论还有待商榷,在以后的研究中建议将样本量增大,患者病情及身体状况分类更加详尽包括关节畸形程度、既往病史、患病时间及患者体质量、年龄、生活质量、工作类型等,这样得出的结论更加有说服力。虽然在临床结果上尚不能统一,但都提示导航比常规手术更加精准,这对于一些手术经验不足的医院和/或医生来说也是引进使用的重要参考点。 2.4 CANS适用人群 在过去的几十年里,TKA松动仍然是一个值得深入研究的问题。瑞典膝关节置换术登记册中显示65岁以下患者的翻修率为8.5%,而65岁以上患者的翻修率为2%[42]。作者认为65岁以下人群对生活质量要求高,平时日常活动更加频繁,要满足此类人群就要追求更加精准的下肢力线、更好的软组织平衡及相关数据。因此,计算机导航在TKA术中的成本效益将更有利于应用于预期寿命较长、生活质量要求较高的患者群体。LUAN等[43]研究296例患者利用CANS进行单侧TKA,根据性别、年龄、体质量指数、术前髋膝关节角度、运动范围和膝关节协会评分进行分层分析,发现术前内翻畸形超过10°的患者更适合运动学对齐,而体质量指数> 30 kg/m2的患者将更多地受益于机械对齐,严重畸形的患者经常有严重的膝关节挛缩,这些患者需要更多的软组织释放。CANS在软组织的释放中可以发挥重要作用,同时计算机导航可以出色地实现肢体和组件的对齐,而与患者的体质量指数无关,尽管肥胖本身并不是在TKA期间使用CANS的指征,但它将有助于在肥胖患者中始终如一准确地对准肢体和组件[44]。 当膝关节骨性关节炎导致关节外畸形或关节外畸形导致膝关节骨关节炎,在这种情况下进行TKA可能会使患者面临持续疼痛和早期置入失败的风险,因为股骨和/或胫骨关节外畸形造成了异常的解剖轴与不佳的骨标记物,使得正确位置和机械轴的识别困难,这时靠传统的髓内、外引导截骨是不可靠的。TANI等[45]研究表明关节外畸形的患者应用导航,TKA术后膝关节功能评分明显高于传统手术方式,影像学结果的异常值比例也较低,表示CANS对关节外畸形的患者很有用。MATASSI等[46]表示基于加速度计的导航可以使关节外畸形的患者在TKA术后准确实现下肢机械对准并准确置入。CATANI等[47]报告了20例继发于远端股骨或胫骨骨折的关节外畸形患者使用无图像导航系统进行TKA,结果显示,从平均术前对齐(10.4±8.3)°内翻改善到平均术后对齐(0.8±1.2)°内翻,膝关节协会评分从48.4分改善到91.4分,而且未发生一系列并发症。也有学者表明即使使用CANS,在股骨外侧弓角度大的患者中术后冠状位异常值发生率也较高,并且股骨外侧弓的严重程度与术后机械髋膝关节角度异常值的发生率呈正相关[48]。 BOYLAN等[49]在纽约全州规划和研究合作系统中分析在TKA和全髋关节置换术中利用机器人和计算机导航技术的趋势,并确定更有可能使用该技术的患者情况。得出该技术辅助TKA比髋关节置换更常见,而且应用该技术辅助比例每年都在增长,从2008年的2.8%增加到2015年的8.6%;具有私人保险患者的导航技术辅助使用率显著高于医疗保险或医疗补助的患者,同时大型或极大型的医院导航技术辅助利用率也高于小型医院。这些数据表明生活水平高的患者使用CANS的比例高,这可能与患者的自身要求有关,大型医院导航技术的利用率较高可能与需要获得相关数据进行研究有关。 2.5 CANS在其他TKA的应用进展 单髁膝关节置换术是治疗单室膝关节骨性关节炎的有效方法,近些年广泛地在临床上应用。相对TKA,单髁置换术有更快的恢复时间,可保存较多骨量,但是其翻修率较高,通常单髁置换术的翻修是进行TKA。SUN等[50]对翻修单髁置换和原发性TKA的术后结果进行Meta分析,得出将单髁置换术转化为TKA比原发性TKA具有更差的临床结果,此外,单髁置换术转换为TKA比初次TKA更复杂,翻修通常需要更长的胫骨假体柄、更厚的聚乙烯成分和骨移植。LEE等[51]通过CANS将翻修的单髁置换术改为TKA,得出导航辅助翻修可以产生与初级导航辅助TKA相似的临床和放射学结果,并减少骨移植和聚乙烯厚度。因为导航系统可以提供有关骨切除和厚度的信息,尽量减少骨丢失并实现最佳对齐,这样可以使外科医生在实际切除之前设计一个最佳计划。 微创TKA手术因为手术视野有限可能会使组织过度收缩,导致术中并发症增加和股骨胫骨组件错位[52]。ALCELIK等[53]研究得出在没有导航的微创组中,冠状面胫骨组件和机械轴的异常值数与导航组相比差异有显著性意义,导航组表现更好;在手术时间、并发症、术后功能评分中,各组之间唯一的统计差异是微创导航组手术时间显著延长,平均增加32 min,但与并发症的增加无关。ZHU等[54]表示将计算机导航与TKA的微创手术方法相结合,CANS可以降低微创膝关节置换术中遇到的截骨和假体定位的精度误差,利用两者的优点,在短期内可以使患者更好和更早地进行功能恢复,并取得令人满意的长期临床和功能结果。 2.6 CANS的最新进展 基于加速度计的便携式导航是最新研发出来的导航系统如OrthAlign?和iASSIST?,与传统技术相比股骨和/或胫骨中使用经皮/经骨定位针的系统会引起穿刺部位并发症,包括疼痛、感染以及很少但破坏性严重的骨折;同时基于加速度计的导航系统具有不增加手术时间、学习曲线较短、费用低于传统导航等优势。PATEL等[55]在处理1例多发性骨软骨瘤膝关节严重外翻畸形的患者时使用基于加速度计的CANS,术后外翻角度为25°-4°,活动范围为0°-135°,膝关节无不稳定发生。IORIO等[56]对53例患者使用基于加速度计导航TKA进行手术,所有患者假体胫骨成分相对于机械轴的垂直方向在3°内对齐。NAM等[57]也表示,便携式导航系统在股骨测截骨同样具有准确性,对48例患者进行测量显示术中目标0°与X射线片上测量的实际术后股骨组分对位的平均绝对差值为(0.8±0.6)°,95.8%定位在术中目标2°以内,100%定位在术中目标3°以内。HUANG等[58]为了研究TKA术中机械轴的修复与改善放置假体成功率之间的关系并评估对线精准度和手术时间,对53例患者使用便携式导航,X射线片结果显示股骨对齐是(0.29±2.2)°内翻,胫骨对齐为(0.09±1.4)°外翻,术后机械轴为(0.2±2.1)°内翻;股骨、胫骨和机械轴的错位率分别为13%,3.8%和17%,固定和导航的平均时间为股骨 3.6 min,胫骨2.6 min,平均止血带时间为 62 min,研究结果表明便携式导航系统不但可以重建精确的下肢机械轴还不增加手术时长;而且与传统导航相比,基于加速度计的便携式导航可避免在股骨和胫骨中使用额外的引脚位置参考阵列,减少了表面配准的要求,消除了红外摄像机和参考阵列之间的术中视线问题[59]。 一种新的、基于手持的iPod导航系统被研发出来,该设备的核心是无菌悬垂的iPod插入一个带有3个反射标记球的手持指针支架,iPod通过红外线摄像头支架中的分离式电脑平台远程工作,3个反射标记球被红外摄像机跟踪,利用连接在手持支架上的指针实现股骨与胫骨解剖标志的数字化。与传统的导航系统相比,基于iPod的导航系统在胫骨和股骨远端骨切割厚度、股骨切割平面和肢体对齐方面表现出良好的相关性和可靠性;它具有快速的注册功能,使TKA的导航系统朝着更加紧凑、用户友好、时间和成本效益迈出了重要的一步[60]。ULIVI等[61]通过测量胫骨和股骨截骨的真实厚度,并与导航系统获得的数据进行比较,测得iPod导航器提供的数据与术中利用游标卡尺进行解剖学测量之间的差异是最小的,平均值为0.03-0.34 mm。KOENEN等[62]进一步验证了这一说法,术后X射线片结果显示与最终导航测量相比平均差异为(1.3±0.9)°,使用iPod导航患者100%在内翻/外翻范围3°内,而且导航所需的平均额外时间为5 min。 2.7 CANS的劣势 HSU等[63]结合技术验收模型和计划行动理论评价得出,医院骨科医生对CANS的接受是成功,但是膝关节置换术已是发展成熟术式,大部分临床医师可以通过手术经验、感觉及目测很好地完成手术,应用CANS尤其是不经常使用的医师需要学习曲线,会增加手术时间和感染概率,而且增加手术费用,最后的临床结果和传统手术方式相差不大,甚至不如传统手术。KANLI?等[64]的研究表明每例导航TKA平均增加10-20 min。NOVAK等[65]表明CANS的TKA比传统手术每例增加1 500美元[66]。CONFALONIERI等[67]观察使用导航系统进行TKA所需的学习曲线,结果显示,没有接受计算机辅助训练但TKA经验丰富的医生需要9例病例,没有接受计算机辅助训练及TKA经验不足的医生需要16例病例。 在应用TKA的导航中主要以无图像CANS和手持式便捷导航系统为主,术中需要髋关节活动来进行解剖标志的注册,对于髋关节僵直的患者不宜使用导航系统。Shah等[68]研究得出导致假体和下肢力线出现异常指标,有一半原因以上是源于不能准确地获取髋部中心的数据,还表示计算机、跟踪系统或摄像机设备都可能会产生系统性的错误。股骨和胫骨需要打入定位杆,就会造成相关并发症的发生,比如骨折、感染等。KHAKHA等[69]研究1 596例CANS术后相关的并发症,并发症发生率很低约1.9%,并且大多是容易治疗的,最常见的并发症是胫骨定位杆的浅表感染。定位杆造成的骨折一般都是个案报道,无系统统计[70-71]。另外在实际使用过程中,可能会因计算机设备的精度影响、术中示踪器松动、术中配准误差等,导致系统输出不正确的手术信息,误导术者的操作。基于加速度计的便携式导航只协助假体组件的对齐,对假体组件大小、假体组件旋转、韧带平衡的意义微乎其微,它可以被简单地视为提高截骨精确度的工具[72]。 BUDHIPARAMA等[73]研究得出基于加速度计的便携式导航在假体组件对齐上有一定的作用,但对功能结果、并发症、再手术的风险没有好处,建议在没有说服力的证据支持之前不要广泛采用新技术。"
| [1] 杨朝君,孙智文,张爱民,等.人工全膝关节置换术结合加速康复外科理念治疗膝关节骨关节炎的临床效果[J]. 中华损伤与修复杂志(电子版),2019,14(5):330-338. [2] MCCALDEN RW, ROBERT CE, HOWARD JL, et al. Comparison of outcomes and survivorship between patients of different age groups following TKA. J Arthroplasty. 2013;28(8 Suppl):83-86. [3] TJOUMAKARIS FP, TUCKER BC, POST Z, et al. Arthroscopic lysis of adhesions for the stiff total knee: results after failed manipulation. Orthopedics. 2014;37(5):e482-487. [4] FENG B, WENG X, LIN J, et al. Long-term follow-up of cemented fixed-bearing total knee arthroplasty in a Chinese population: a survival analysis of more than 10 years. J Arthroplasty. 2013;28(10):1701-1706. [5] JENNY JY, CLEMENS U, KOHLER S, et al. Consistency of implantation of a total knee arthroplasty with a non-image-based navigation system: a case-control study of 235 cases compared with 235 conventionally implanted prostheses. J Arthroplasty. 2005;20(7):832-839. [6] SCHWARZ ML, POTT PP, BECK A, et al. Test bed for assessment of the kinematical determination of navigation systems for total knee arthroplasty. Does a limited range of motion of the hip joint influence the accuracy of the determination? Comput Aided Surg. 2005;10(1):51-57. [7] 黄润华,尚希福,胡飞,等. 人工全膝关节置换术治疗老年膝关节病变合并膝外翻畸形的疗效分析[J]. 临床骨科杂志,2017,20(3): 310-313+317. [8] THIELE K, PERKA C, MATZIOLIS G, et al. Current failure mechanisms after knee arthroplasty have changed: polyethylene wear is less common in revision surgery. J Bone Joint Surg Am. 2015;97(9):715-720. [9] FU Y, WANG M, LIU Y, et al. Alignment outcomes in navigated total knee arthroplasty: a meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2012;20(6):1075-1082. [10] KOHN D, RUPP S. Knieendoprothetik--Operationstechnische Aspekte [Knee endoprosthesis: aspects of surgical techniques]. Orthopade. 2000;29(8):697-707. [11] DELP SL, STULBERG SD, DAVIES B, et al. Computer assisted knee replacement. Clin Orthop Relat Res. 1998;(354):49-56. [12] PICARD F, DEEP K, JENNY JY. Current state of the art in total knee arthroplasty computer navigation. Knee Surg Sports Traumatol Arthrosc. 2016;24(11):3565-3574. [13] PICARD F, DEAKIN AH, RICHES PE, et al. Computer assisted orthopaedic surgery: Past, present and future. Med Eng Phys. 2019;72:55-65. [14] JONES CW, JERABEK SA. Current Role of Computer Navigation in Total Knee Arthroplasty. J Arthroplasty. 2018;33(7):1989-1993. [15] BÄTHIS H, PERLICK L, TINGART M, et al. Radiological results of image-based and non-image-based computer-assisted total knee arthroplasty. Int Orthop. 2004;28(2):87-90. [16] TABATABAEE RM, RASOULI MR, MALTENFORT MG, et al. Computer-Assisted Total Knee Arthroplasty: Is There a Difference Between Image-Based and Imageless Techniques? J Arthroplasty. 2018;33(4):1076-1081. [17] DEEP K, SHANKAR S, MAHENDRA A. Computer assisted navigation in total knee and hip arthroplasty. SICOT J. 2017;3:50. [18] ANTONIOS JK, KORBER S, SIVASUNDARAM L, et al. Trends in computer navigation and robotic assistance for total knee arthroplasty in the United States: an analysis of patient and hospital factors. Arthroplast Today. 2019;5(1):88-95. [19] ZHANG YZ, LU S, ZHANG HQ, et al. Alignment of the lower extremity mechanical axis by computer-aided design and application in total knee arthroplasty. Int J Comput Assist Radiol Surg. 2016;11(10):1881-1890. [20] TODESCA A, GARRO L, PENNA M, et al. Conventional versus computer-navigated TKA: a prospective randomized study. Knee Surg Sports Traumatol Arthrosc. 2017;25(6):1778-1783. [21] HARVIE P, SLOAN K, BEAVER RJ. Computer navigation vs conventional total knee arthroplasty: five-year functional results of a prospective randomized trial. J Arthroplasty. 2012;27(5):667-672.e1. [22] CIP J, OBWEGESER F, BENESCH T, et al. Twelve-Year Follow-Up of Navigated Computer-Assisted Versus Conventional Total Knee Arthroplasty: A Prospective Randomized Comparative Trial. J Arthroplasty. 2018;33(5):1404-1411. [23] FICKERT S, JAWHAR A, SUNIL P, et al. Precision of Ci-navigated extension and flexion gap balancing in total knee arthroplasty and analysis of potential predictive variables. Arch Orthop Trauma Surg. 2012;132(4):565-574. [24] CHIA ZY, PANG HN, TAN MH, et al. Gap difference in navigated TKA: a measure of the imbalanced flexion-extension gap. SICOT J. 2018;4:30. [25] RITTER MA, LUTGRING JD, DAVIS KE, et al. The role of flexion contracture on outcomes in primary total knee arthroplasty. J Arthroplasty. 2007; 22(8):1092-1096. [26] WADA K, MIKAMI H, HAMADA D, et al. Measurement of rotational and coronal alignment in total knee arthroplasty using a navigation system is reproducible. Arch Orthop Trauma Surg. 2016;136(2):271-276. [27] SARDANA V, BURZYNSKI JM, KHAN M, et al. Long-term functional outcomes and knee alignment of computer-assisted navigated total knee arthroplasty. Musculoskelet Surg. 2017;101(1):37-43. [28] SIU KK, WU KT, KO JY, et al. Effects of computer-assisted navigation versus the conventional technique for total knee arthroplasty on levels of plasma thrombotic markers: a prospective study. Biomed Eng Online. 2019;18(1):99. [29] JIANG T, SONG K, YAO Y, et al. Perioperative allogenic blood transfusion increases the incidence of postoperative deep vein thrombosis in total knee and hip arthroplasty. J Orthop Surg Res. 2019;14(1):235. [30] LIODAKIS E, ANTONIOU J, ZUKOR DJ, et al. Navigated vs Conventional Total Knee Arthroplasty: Is There a Difference in the Rate of Respiratory Complications and Transfusions? J Arthroplasty. 2016;31(10):2273-2277. [31] LALMOHAMED A, VESTERGAARD P, KLOP C, et al. Timing of acute myocardial infarction in patients undergoing total hip or knee replacement: a nationwide cohort study. Arch Intern Med. 2012; 172(16):1229-1235. [32] KUO SJ, HSU HC, WANG CJ, et al. Effects of computer-assisted navigation versus conventional total knee arthroplasty on the levels of inflammation markers: A prospective study. PLoS One. 2018;13(5): e0197097. [33] LANGKILDE A, JAKOBSEN TL, BANDHOLM TQ, et al. Inflammation and post-operative recovery in patients undergoing total knee arthroplasty-secondary analysis of a randomized controlled trial. Osteoarthritis Cartilage. 2017;25(8):1265-1273. [34] KUO SJ, WANG FS, WANG CJ, et al. Effects of Computer Navigation versus Conventional Total Knee Arthroplasty on Endothelial Damage Marker Levels: A Prospective Comparative Study. PLoS One. 2015;10(5): e0126663. [35] LÜTZNER J, GÜNTHER KP, KIRSCHNER S. Functional outcome after computer-assisted versus conventional total knee arthroplasty: a randomized controlled study. Knee Surg Sports Traumatol Arthrosc. 2010;18(10):1339-1344. [36] DENTI M, SOLDATI F, BARTOLUCCI F, et al. Conventional versus Smart Wireless Navigation in Total Knee Replacement: Similar Outcomes in a Randomized Prospective Study. Joints. 2018;6(2):90-94. [37] AYEKOLOYE C, NWANGWU O, ALONGE T. Computer Navigation-Assisted Knee Replacement Demonstrates Improved Outcome Compared with Conventional Knee Replacement at Mid-Term Follow-up: A Systematic Review and Meta-analysis. Indian J Orthop. 2020;54(6):757-766. [38] SONG EK, AGRAWAL PR, KIM SK, et al. A randomized controlled clinical and radiological trial about outcomes of navigation-assisted TKA compared to conventional TKA: long-term follow-up. Knee Surg Sports Traumatol Arthrosc. 2016;24(11):3381-3386. [39] PETURSSON G, FENSTAD AM, GØTHESEN Ø, et al. Computer-Assisted Compared with Conventional Total Knee Replacement: A Multicenter Parallel-Group Randomized Controlled Trial. J Bone Joint Surg Am. 2018;100(15):1265-1274. [40] MARTÍN-HERNÁNDEZ C, SANZ-SAINZ M, REVENGA-GIERTYCH C, et al. Navigated versus conventional total knee arthroplasty: A prospective study at three years follow-up. Rev Esp Cir Ortop Traumatol. 2018: S1888-4415(18)30007-9. [41] BAUMBACH JA, WILLBURGER R, HAAKER R, et al. 10-Year Survival of Navigated Versus Conventional TKAs: A Retrospective Study. Orthopedics. 2016;39(3 Suppl):S72-76. [42] HARRYSSON OL, ROBERTSSON O, NAYFEH JF. Higher cumulative revision rate of knee arthroplasties in younger patients with osteoarthritis. Clin Orthop Relat Res. 2004;(421):162-168. [43] LUAN C, XU DT, CHEN NJ, et al. How to choose kinematic or mechanical alignment individually according to preoperative characteristics of patients? BMC Musculoskelet Disord. 2020;21(1):443. [44] SHETTY GM, MULLAJI AB, BHAYDE S, et al. No effect of obesity on limb and component alignment after computer-assisted total knee arthroplasty. Knee. 2014;21(4):862-865. [45] TANI I, NAKANO N, TAKAYAMA K, et al. Navigated total knee arthroplasty for osteoarthritis with extra-articular deformity. Acta Ortop Bras. 2018;26(3):170-174. [46] MATASSI F, COZZI LEPRI A, INNOCENTI M, et al. Total Knee Arthroplasty in Patients With Extra-Articular Deformity: Restoration of Mechanical Alignment Using Accelerometer-Based Navigation System. J Arthroplasty. 2019;34(4):676-681. [47] CATANI F, DIGENNARO V, ENSINI A, et al. Navigation-assisted total knee arthroplasty in knees with osteoarthritis due to extra-articular deformity. Knee Surg Sports Traumatol Arthrosc 2012;20:546-551. [48] NAM JH, SONG SK, CHO MR, et al. The advantage of navigation for knee with lateral femoral bowing in total knee arthroplasty. J Orthop Surg (Hong Kong). 2020;28(3):2309499020965679. [49] BOYLAN M, SUCHMAN K, VIGDORCHIK J, et al. Technology-Assisted Hip and Knee Arthroplasties: An Analysis of Utilization Trends. J Arthroplasty. 2018;33(4):1019-1023. [50] SUN X, SU Z. A meta-analysis of unicompartmental knee arthroplasty revised to total knee arthroplasty versus primary total knee arthroplasty. J Orthop Surg Res. 2018;13(1):158. [51] LEE HJ, PARK YB, SONG MK, et al. Comparison of the outcomes of navigation-assisted revision of unicompartmental knee arthroplasty to total knee arthroplasty versus navigation-assisted primary TKA. Int Orthop. 2019;43(2):315-322. [52] ALCELIK I, SUKEIK M, POLLOCK R, et al. Comparison of the minimally invasive and standard medial parapatellar approaches for primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2012; 20(12):2502-2512. [53] ALCELIK IA, BLOMFIFIELD MI, DIANA G, et al. A Comparison of Short Term Outcomes of Minimally Invasive Computer Assisted versus Minimally Invasive Conventional Instrumentation for Primary Total Knee Arthroplasty A Systematic Review and Meta-analysis. J Arthroplasty. 201 6;31(2):410-418. [54] ZHU M, ANG CL, YEO SJ, et al. Minimally Invasive Computer-Assisted Total Knee Arthroplasty Compared With Conventional Total Knee Arthroplasty: A Prospective 9-Year Follow-Up. J Arthroplasty. 2016;31(5):1000-1004. [55] PATEL BH, ZEEGEN E, SASSOON A. Accelerometer-Based, Computer-Navigated Total Knee Arthroplasty to Correct a Complex Deformity in a Patient With Multiple Hereditary Exostoses. Arthroplast Today. 2020;6(4):796-802. [56] IORIO R, MAZZA D, DROGO P, et al. Clinical and radiographic outcomes of an accelerometer-based system for the tibial resection in total knee arthroplasty. Int Orthop. 2015;39(3):461-466. [57] NAM D, NAWABI DH, CROSS MB, et al. Accelerometer-based computer navigation for performing the distal femoral resection in total knee arthroplasty. J Arthroplasty. 2012;27(9):1717-1722. [58] HUANG EH, COPP SN, BUGBEE WD. Accuracy of A Handheld Accelerometer-Based Navigation System for Femoral and Tibial Resection in Total Knee Arthroplasty. J Arthroplasty. 2015;30(11):1906-1910. [59] GOH GS, LIOW MHL, TAY DK, et al. Accelerometer-Based and Computer-Assisted Navigation in Total Knee Arthroplasty: A Reduction in Mechanical Axis Outliers Does Not Lead to Improvement in Functional Outcomes or Quality of Life When Compared to Conventional Total Knee Arthroplasty. J Arthroplasty. 2018;33(2):379-385. [60] MULLAJI AB, SHETTY GM. Efficacy of a novel iPod-based navigation system compared to traditional navigation system in total knee arthroplasty. Comput Assist Surg (Abingdon). 2017;22(1):10-13. [61] ULIVI M, ORLANDINI LC, MERONI V, et al. Intraoperative validation of bone cut accuracy of a pinless smart touch-screen navigation system device in total knee arthroplasty. Int J Med Robot. 2019;15(5):e2030. [62] KOENEN P, SCHNEIDER MM, FRÖHLICH M, et al. Reliable Alignment in Total Knee Arthroplasty by the Use of an iPod-Based Navigation System. Adv Orthop. 2016;2016:2606453. [63] HSU HM, CHANG IC, LAI TW. Physicians’ perspectives of adopting computer-assisted navigation in orthopedic surgery. Int J Med Inform. 2016;94:207-214. [64] KANLIĆ EM, DELAROSA F, PIRELA-CRUZ M. Computer assisted orthopaedic surgery -- CAOS. Bosn J Basic Med Sci. 2006;6(1):7-13. [65] NOVAK EJ, SILVERSTEIN MD, BOZIC KJ. The cost-effectiveness of computer-assisted navigation in total knee arthroplasty. J Bone Joint Surg Am. 2007;89(11):2389-2397. [66] GOH GS, LIOW MH, LIM WS, et al. Accelerometer-Based Navigation Is as Accurate as Optical Computer Navigation in Restoring the Joint Line and Mechanical Axis After Total Knee Arthroplasty: A Prospective Matched Study. J Arthroplasty. 2016;31(1):92-97. [67] CONFALONIERI N, CHEMELLO C, CERVERI P, et al. Is computer-assisted total knee replacement for beginners or experts? Prospective study among three groups of patients treated by surgeons with different levels of experience. J Orthop Traumatol. 2012;13(4):203-210. [68] SHAH SM, SCIBERRAS NC, ALLEN DJ, et al. Technical and surgical causes of outliers after computer navigated total knee arthroplasty. J Orthop. 2019;18:171-176. [69] KHAKHA RS, CHOWDHRY M, NORRIS M, et al. Low incidence of complications in computer assisted total knee arthroplasty--A retrospective review of 1596 cases. Knee. 2015;22(5):416-418. [70] BELDAME J, BOISRENOULT P, BEAUFILS P. Pin track induced fractures around computer-assisted TKA. Orthop Traumatol Surg Res. 2010; 96(3):249-255. [71] BLUE M, DOUTHIT C, DENNISON J, et al. Periprosthetic Fracture through a Unicortical Tracking Pin Site after Computer Navigated Total Knee Replacement. Case Rep Orthop. 2018;2018:2381406. [72] BATAILLER C, SWAN J, SAPPEY MARINIER E, et al. New Technologies in Knee Arthroplasty: Current Concepts. J Clin Med. 2020;10(1):47. [73] BUDHIPARAMA NC, LUMBAN-GAOL I, IFRAN NN, et al. Does Accelerometer-based Navigation Have Any Clinical Benefit Compared with Conventional TKA? A Systematic Review. Clin Orthop Relat Res. 2019;477(9):2017-2029. [74] SMITH BR, DEAKIN AH, BAINES J, et al. Computer navigated total knee arthroplasty: the learning curve. Comput Aided Surg. 2010;15(1-3):40-48. [75] PACHECO AP, FILHO OT, DA MOTA E, et al. Navigated versus mechanical knee replacement: comparison between initial navigated and conventional cases performed by the same surgeon. Rev Bras Ortop. 2015;47(3):359-362. (责任编辑:GD,ZN,ZH) |
| [1] | Pu Rui, Chen Ziyang, Yuan Lingyan. Characteristics and effects of exosomes from different cell sources in cardioprotection [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(在线): 1-. |
| [2] | Wang Jinjun, Deng Zengfa, Liu Kang, He Zhiyong, Yu Xinping, Liang Jianji, Li Chen, Guo Zhouyang. Hemostatic effect and safety of intravenous drip of tranexamic acid combined with topical application of cocktail containing tranexamic acid in total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1356-1361. |
| [3] | Peng Zhihao, Feng Zongquan, Zou Yonggen, Niu Guoqing, Wu Feng. Relationship of lower limb force line and the progression of lateral compartment arthritis after unicompartmental knee arthroplasty with mobile bearing [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1368-1374. |
| [4] | Zhang Chao, Lü Xin. Heterotopic ossification after acetabular fracture fixation: risk factors, prevention and treatment progress [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1434-1439. |
| [5] | Zhou Jihui, Li Xinzhi, Zhou You, Huang Wei, Chen Wenyao. Multiple problems in the selection of implants for patellar fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1440-1445. |
| [6] | Wang Debin, Bi Zhenggang. Related problems in anatomy mechanics, injury characteristics, fixed repair and three-dimensional technology application for olecranon fracture-dislocations [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1446-1451. |
| [7] | Ji Zhixiang, Lan Changgong. Polymorphism of urate transporter in gout and its correlation with gout treatment [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1290-1298. |
| [8] | Yuan Mei, Zhang Xinxin, Guo Yisha, Bi Xia. Diagnostic potential of circulating microRNA in vascular cognitive impairment [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1299-1304. |
| [9] | Wang Xianyao, Guan Yalin, Liu Zhongshan. Strategies for improving the therapeutic efficacy of mesenchymal stem cells in the treatment of nonhealing wounds [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1081-1087. |
| [10] | Wan Ran, Shi Xu, Liu Jingsong, Wang Yansong. Research progress in the treatment of spinal cord injury with mesenchymal stem cell secretome [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1088-1095. |
| [11] | Liao Chengcheng, An Jiaxing, Tan Zhangxue, Wang Qian, Liu Jianguo. Therapeutic target and application prospects of oral squamous cell carcinoma stem cells [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1096-1103. |
| [12] | Zhao Min, Feng Liuxiang, Chen Yao, Gu Xia, Wang Pingyi, Li Yimei, Li Wenhua. Exosomes as a disease marker under hypoxic conditions [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1104-1108. |
| [13] | Xie Wenjia, Xia Tianjiao, Zhou Qingyun, Liu Yujia, Gu Xiaoping. Role of microglia-mediated neuronal injury in neurodegenerative diseases [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1109-1115. |
| [14] | Li Shanshan, Guo Xiaoxiao, You Ran, Yang Xiufen, Zhao Lu, Chen Xi, Wang Yanling. Photoreceptor cell replacement therapy for retinal degeneration diseases [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1116-1121. |
| [15] | Jiao Hui, Zhang Yining, Song Yuqing, Lin Yu, Wang Xiuli. Advances in research and application of breast cancer organoids [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1122-1128. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||