Chinese Journal of Tissue Engineering Research ›› 2021, Vol. 25 ›› Issue (9): 1446-1451.doi: 10.3969/j.issn.2095-4344.3753
Previous Articles Next Articles
Related problems in anatomy mechanics, injury characteristics, fixed repair and three-dimensional technology application for olecranon fracture-dislocations
Wang Debin, Bi Zhenggang
- Department of Orthopedics, First Affiliated Hospital of Harbin Medical University, Harbin 150001, Heilongjiang Province, China
-
Received:2020-05-19Revised:2020-05-20Accepted:2020-06-21Online:2021-03-28Published:2020-12-16 -
Contact:Bi Zhenggang, Professor, Doctoral supervisor, Department of Orthopedics, First Affiliated Hospital of Harbin Medical University, Harbin 150001, Heilongjiang Province, China -
About author:Wang Debin, Master candidate, Physician, Department of Orthopedics, First Affiliated Hospital of Harbin Medical University, Harbin 150001, Heilongjiang Province, China
CLC Number:
Cite this article
Wang Debin, Bi Zhenggang. Related problems in anatomy mechanics, injury characteristics, fixed repair and three-dimensional technology application for olecranon fracture-dislocations[J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1446-1451.
share this article
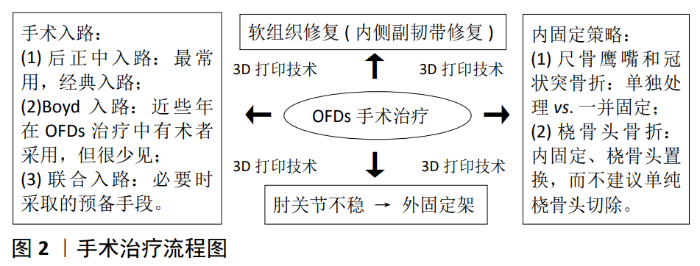
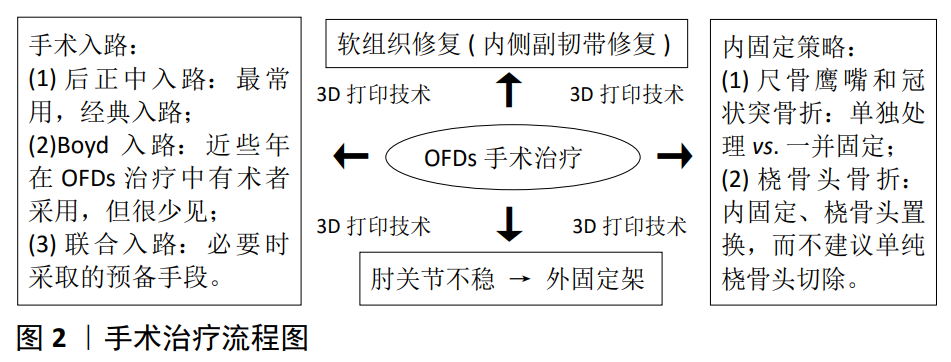
2.1 解剖力学 肘关节是由3种关节整合成的铰链关节,具有高度的协调性和稳定性。肘关节的稳定性首要来自肱尺关节和副韧带复合体的静态限制,其次则是桡骨头、关节囊的静态限制和相关肌肉的动静结合控制。在肱尺关节的静态限制中,鹰嘴阻止肘前移,冠状突则是防止肘后移,且维持肘内翻、前臂旋转的稳定。在滑车切迹中,鹰嘴和冠状突之间被3-5 mm的无软骨“裸区”隔开[8-12],因此,OFDs中鹰嘴和冠状突的复位固定,应注意防止“裸区”变形。 尺骨近端解剖特点主要体现在尺骨桡侧切迹、与鹰嘴相关3种成角和骨质密度分布方面,并对临床诊疗效果具有一定的影响。WEGMANN等[13]通过计算机断层扫描分析发现,尺骨桡侧切迹解剖特点凸显其可变性,其深度由近端向远端递减,且随著曲率半径的增加和冠状面的旋转而改变,影响着尺桡骨近端的匹配。与鹰嘴相关的3种成角则是尺骨近端整体结构特点的体现,也是临床常用的解剖角。BESER等[14]对50个尺骨近端结构进行了详细的测量,其结果显示,鹰嘴后皮层与尺骨干背侧切线构成的尺骨近端背侧角平均(8± 2.3)°( 4°–12°);尺骨干中轴线与鹰嘴轴线构成的尺骨近端内翻角平均(9.3±2.2)°(4°–15°);尺骨中轴线与滑车切迹两末端连线构成的鹰嘴-骨干角平均为(19.3±2.8)° (13°–25°)。在骨质密度方面,GIL等[15]采取定量计算机断层扫描骨密度三维分布,在滑车切迹的近端(包括鹰嘴的尖端)表现高骨密度,且鹰嘴的尖端远比冠状突的尖端骨密度高,并建议骨折固定的方向应朝向高密度处进行。上述3种特点不但影响着临床术前规划和术中操作,而且对OFDs治疗的预后评估也有一定意义。 除了上述尺骨近端特点需要重视外,桡骨头、韧带、关节囊以及相关肌肉在肘关节中起到的作用同样不容忽视。首先,桡骨头虽然是外翻和外旋中重要的二次稳定器,但是桡骨头骨折固定可使在内侧副韧带断裂时肘外翻的稳定性得到很大的提升。其次,内侧副韧带、外侧副韧带分别是外翻、外翻应力的主要限制因素,分别始于内、外上髁,止于冠状突、环状韧带和桡骨外侧;关节囊在肘内、外翻应力中,其前部起到主要抵抗作用[11-16];同时,肱肌、肱二头肌、肱三头肌分别在冠状突、桡骨转子、尺骨鹰嘴处存在止点,且三者的损坏或丢失可导致所有屈曲位置的内翻外翻松弛度增加[9,17-19]。 2.2 损伤特点 OFDs中尺骨鹰嘴骨折仅仅是其损伤之一,冠状突、桡骨头、韧带等也可能受牵连。OFDs以肘关节为核心,鹰嘴为肘关节发生脱位的通道[20]。 首先,OFDs可进一步划分为前方OFDs和后方OFDs。前方OFDs,是在半屈肘时高能量外力冲击前臂背侧面,在肱骨滑车嵌压滑车切迹下摧毁鹰嘴,导致尺桡骨前移,也被视为经鹰嘴骨折-脱位。前脱位发生率仅1%-2%,开放伤多见,常伴冠状突骨折(Regan-Morrey Ⅲ型多见);肱尺关节因部分不吻合而形成半脱位,较少累及韧带[11,21-22]。虽然前Monteggia损伤也发生类似问题,但近端桡尺关系稳定,尤其是环状韧带约束完好是前Monteggia损伤所不具备的特点[23-24]。后方OFDs,尚无关于该损伤机制的文献明确性报道,部分学者推测为屈肘90°时轴向力所致;但是后方OFDs发生率较高,多为闭合伤,常牵涉到冠状突、桡骨头和外侧副韧带。桡骨头骨折常为Mason Ⅱ、Ⅲ型;冠状突骨折块大,也多为Regan-Morrey Ⅲ型。由于肱尺关节相对稳定,近端尺桡关节不稳,后方OFDs接近于极近端的后Monteggia损伤[2,6,16,22-23]。但是,在损伤的侧重点问题上,Monteggia损伤绝大多数涉及尺骨干问题,而OFDs主要影响的是尺骨滑车切迹。 其次,生物力学角度也可发现了OFDs的损伤特点,在垂直荷载力的作用下,不同关节角度承受的载荷超过极限时,则发生骨折脱位。当屈肘0°-15°时,可出现 Regan-Morrey Ⅱ型骨折;当屈肘15°-30°时,可发生冠状突骨折后脱位;当屈肘30°-45°时,可发生Regan-Morrey Ⅲ型骨折。随着屈肘角度的增大,应力逐渐集中到鹰嘴后部,当屈肘60°或90°时,可发生鹰嘴骨折前脱位[25-26]。 由此可见,鹰嘴、冠状突骨折不稳在OFDs的损伤特点中占据着主导的地位,影响着OFDs损伤机制的研究,而且后方OFDs损伤机制也有可能从生物力学角度被突破发现。 2.3 诊断分型 OFDs临床表现常为关节肿痛、畸形、活动障碍,且需评估所有的血管、神经损伤情况。YOON等[4]指出除神经血管损害、开放伤等需紧急处理外,伤后急性期查体往往收效甚微。必要时,可在麻醉镇静下进行双侧肘关节查体和伤情评估。此外,影像学检查不但是临床诊断的重要手段,而且对术前规划起着重要作用。患侧肘部X射线片可初步筛查骨折脱位情况,且与健侧肘部X射线片对比,可提升诊疗精准度。对于非粉碎性移位的鹰嘴骨折,只需X射线片即可辨别;当出现因肿痛而伸肘障碍和复杂骨折时,X射线片可发生显影重叠,骨折情况辨别困难。CT和定量三维CT检查则可更全面地观察骨折移位、粉碎程度,排除隐匿性骨折和其他损伤,以及进行冠状突O’Driscoll分型[4,11,27-29]。而MRI并不是完全肯定的必要检查,且不适用肘部创伤急性期[7,11]。此外,鹰嘴骨折的常见几种分型分别为Colton分型、AO分型、Schatzker 分型以及Mayo分型[30],但是目前尚缺少专门针对OFDs独立分型的报道,临床上对该类损伤仍以鹰嘴、冠状突、桡骨头各自骨折分型为主。 2.4 手术治疗 OFDs是一种复杂肘关节损伤,涉及多处组织结构的关节内骨折,造成关节移位不稳,常需采取手术治疗,同心解剖复位固定、可靠地保持稳定、允许早期运动锻炼是OFDs的治疗目标[20,31-32]。首要问题是重建鹰嘴、冠突并恢复滑车切迹形态,同时对伴有的桡骨头骨折问题进行修复/置换;其次则是韧带、关节囊等修复问题,必要时需联合外固定架[7,33-34]。手术治疗流程图见图2。 2.4.1 手术入路 根据损伤具体形态和结构位置不同,选择恰当的手术入路将成为关键问题[16,35]。其中后正中入路可同时处理尺骨和桡骨头骨折以及韧带等软组织,显露结构较广,是很多术者手术治疗OFDs的常用入路[16,31]。李红军等[20]采取后正中入路将鹰嘴骨折块连同肌腱一并翻起的方式治疗OFDs,术后Mayo 肘关节功能评分平均 86.5 分,优良率为87.5%。但是单纯后路有时并不理想,即使挪移鹰嘴骨折块也可能显露不佳,必要时需剥离旋前屈肌群或者肱骨内上髁截骨,致使增加损伤[36]。苏朝阳等[37]则仅通过Boyd入路治疗前方OFDs,虽然对伸肌装置干扰不大,但需要在切断旋后肌基础上进行术野的显露。除了后正中入路和Boyd入路两种单一手术入路外,在这种复杂的肘关节损伤中,为了更有效地固定修复不同部位的损伤,以后正中入路为基础联合其他入路治疗OFDs的策略也受到许多学者的认可。AVASTHI 等[16]指出在桡骨头或冠状突骨折处理困难时,联合内侧或外侧入路也是有必要的。胡晓川等[38]在OFDs病例中通过联合外侧入路处理骨折的桡骨头,术后肘关节 Broberg-Morrey评分平均89.1分,优良率达80%。然而,FENG等[29]则认为肘前入路可使冠状突Regan-Morrey Ⅱ、Ⅲ型骨折达到精准复位和坚强固定。程宇等[36]采取前后联合入路治疗OFDs,术后半年内均达骨愈合标准,末次随访时无疼痛、关节脱位、内植物松动、断裂以及异位骨化问题。郭永权[39]进一步采取前后联合入路与后正中入路分别治疗OFDs,前后联合入路组术中出血量和骨折愈合时间明显少于后正中入路组,术后 Broberg-Morrey 评分明显大于后正中入路组,前后联合入路组和后正中入路组并发症率分别为25.7%及71.4%,且以上对比差异均有显著性意义(P < 0.05)。考虑到总体样本数量为70例,前后联合入路和后正中入路的比较仍需进一步通过大样本的病例统计分析研究。由此可见,后正中入路作为OFDs处理途径的争议性看法较少,且较Boyd入路更常用;而联合入路应在术前或术中发现某处损伤处理困难、无法有效固定修复时,作为一种预备的手术策略。 2.4.2 内固定策略 尺骨鹰嘴骨折主要常用的两种技术包括克氏针张力带技术和钢板技术[30]。克氏针张力带技术可将拉伸力转为压缩力,常用于简单横形骨折,但存在骨间神经损伤、前臂旋转障碍、退针以及针尾刺激症状等相关风险[16,19]。NOWOTNY等[40]认为张力带松动和克氏针滑移可引发骨折处的二次脱位,并提出克氏针的三皮质固定具有更好的拉力强度和固定牢固性,而钢板则常用于斜形、复杂和较差骨质的骨折[16]。在克氏针张力带和钢板的对比中,MIDTGAARD等[41]认为虽然克氏针张力带和锁定钢板在骨折位移或载荷失效方面差异无显著性意义,但锁定钢板对鹰嘴横形骨折固定更可靠。而且,GATHEN等[42]指出钢板可能出现预后不佳的问题,是因为钢板固定常用于骨质量差且更复杂的骨折。针对因钢板刺激周围组织而取出的问题,ELLWEIN等[43]将低矮型双钢板与2.7 mm/3.5 mm锁定加压钢板固定鹰嘴进行对比,内固定取出率分别为27%及38%,差异无显著性意义。同时,解剖锁定钢板可用于缺乏支撑的、粉碎性鹰嘴骨折,当骨量丢失严重时,需植骨重建滑车切迹[19-20]。在冠状突重建中,较小骨折块可行缝合套索固定;冠状突Regan-Morrey Ⅱ、Ⅲ型骨折,常需采用钢板、螺钉固定,而大骨块可用拉力螺钉固定[20,29]。SHEN等[44]用微型钢板固定Regan-Morrey Ⅱ型粉碎骨折,达到了满意的临床疗效。在OFDs治疗中,许多临床医生根据鹰嘴和冠状突单独骨折特点分别固定[20,36]。冯伟楼等[45]更进一步指出先复位固定鹰嘴有利于确保肱骨远端与鹰嘴部分的滑车切迹对合,随后再处理冠状突,并且两处骨折均予以钢板螺钉固定,可使骨折有效复位和牢靠固定,患者术后21周内骨质断端完全愈合。尺骨鹰嘴和冠状突骨折在OFDs中不论其各自损伤类型发生概率高低,均应详细分析各种骨折类型的具体处理,以及植入物的选择和固定技术灵活运用问题。而且,鹰嘴和冠状突骨折的分别单独处理可使骨折准确复位、牢靠固定,但术中术者应注意避免内固定物之间的碰撞问题,同时应尽可能降低这种分别处理办法所带来的软组织损伤风险。 由于OFDs以冠状突Regan-Morrey Ⅲ型大块骨折较为常见,一些学者也采取在尺骨近端后面跨或不跨鹰嘴钢板旋进螺钉的办法,间接固定冠状突[38],但近些年对于这种间接固定的稳定性问题也引发许多争议。MOON 等[46]进一步研究发现,与从前到后方固定相比,从后到前方固定更具有生物力学稳定性。杨如意等[47]认为在鹰嘴后钢板的基础上于尺骨近端内侧辅助微型钢板固定,可使骨折稳定牢靠。但张继斌等[48]强调双钢板固定可使骨膜剥离过多,影响髓外血供,并选择钢丝捆扎辅助后侧单钢板进行固定,患者术后肘关节功能恢复良好。而OZTURKMEN等[49]在OFDs固定修复中通过鹰嘴后面的3.5 mm锁定板以拉力螺钉固定冠状突主要碎片,应用不依赖于鹰嘴板的螺钉固定冠状突小碎片,所有患者术后12周内骨折均愈合,患肘无不稳定症状。 桡骨头骨折处理手段主要取决于骨折的形态特征,对于伴或不伴微小位移的小骨片可暂不手术处理,而较大的骨折块则需切开复位内固定和人工桡骨头置换,并且这种OFDs的桡骨头骨折更不建议单纯切除桡骨头。骨折块≤3块时,可将骨折块进行复位固定;当超过3个骨折块和严重粉碎桡骨头,桡骨头置换成为优先选择的手术方式[50]。近期,REBGETZ等[51]对无头加压螺钉、锁钉钢板固定桡骨头颈骨折进行生物力学分析,虽然两者的研究结果差异无显著性意义,但螺钉可以改善横形骨折。然而,GRUSZKA等[52]在回顾性分析研究中发现用现代锁定钢板固定复杂桡骨头颈骨折,显示出良好的中期结果,并认为现代锁定钢板不仅可以有效固定这种复杂骨折,同时避免了关节置换或桡骨头切除。 2.4.3 软组织修复 软组织结构对肘关节功能稳定具有重要作用,合理恰当地修复可有效改善临床预后。OFDs中外侧副韧带损伤较为常见,且对外侧副韧带的修复得到广泛认可,外侧副韧带可采取不可吸收缝线、缝合锚钉进行修复,必要时需取半腱肌重建[47,53]。程宇等[36]在OFDs的处理中不但注重关节囊的修复,包括前侧入路切开关节囊在手术闭创时予以缝合,而且认为内侧副韧带裂损很少出现在OFDs中;但恰好该研究中1例患者出现内侧副韧带破裂,并予以锚钉修复,患者术后肘关节获得良好固定。但是在软组织修复中内侧副韧带的修复是否必须与处理骨折同时进行,一直以来成为探讨研究的焦点。GIANNICOLA等[54]认为复杂肘关节损伤中内侧副韧带的损伤可通过避免肘内翻而自行瘢痕愈合,并进一步指出如果残余的肘关节不稳,则应修复内侧副韧带和/或使用外固定架。BIZ等[55]对接受保守治疗、手术治疗和保守治疗失败后二期手术治疗3种情况进行临床疗效分析,并指出没有足够的证据证明在保守治疗和手术治疗对内侧副韧带损伤患者功能结局的影响上差异有显著性意义,但一段时间的康复治疗和每例患者的肘关节功能要求标准可辨别哪些患者真正需要外科手术来修复内侧副韧带。 2.4.4 外固定架 外固定架的应用减少了韧带和骨骼重建程序的数量,特别是在粉碎骨折和不稳定脱位的情况下,便于患者术后早期功能康复锻炼,PIZZOLI等[56]采用外固定架治疗32例患者,术后平均肘关节活动范围为屈伸125.9°,内旋77.8°,外旋79.7°,未出现主要并发症和后外侧或内侧关节不稳。但是,TIZIANI等[57]在外固定架应用标准的文献中强调了外固定架所带来的针道感染和桡神经损伤等相关风险。国内朱涛等[58]采用铰链式外固定架处理肘关节损伤不稳,术后1例皮肤软组织发生坏死并治愈,其余均无感染和神经受累问题。因此,术中精准有效地应用外固定架和术后针道精细保护可更好地提升外固定架疗效。 2.4.5 3D打印技术 近年来,3D打印技术凭借术前规划最佳手术入路、种植体置入、外形设计、术中困难预估等优点,越来越多地应用在骨科手术中,为复杂手术程序的术前规划带来了新的机遇[59]。虽然有关3D打印技术在OFDs应用的专门文献资料相对较少,但是OFDs为复杂肘关节骨折脱位中的一类,通过3D打印技术应用于复杂肘关节骨折脱位诊疗的相关文献可明显展现其优势的一面。姬文晨等[60]则将20例肘关节骨折手术治疗患者随机分为3D打印组、常规组进行对比分析,结果显示,出血量分别(153.3±23.9) mL及(246.3±34.7) mL,手术时间分别为(2.1±0.3) h及(2.9±0.4) h,透视次数分别为(8.7±1.6) 次及(11.1±1.2) 次,且上述3方面差异均有显著性意义(P < 0.05) ,且3D打印组术后1年Mayo评分和患肘活动范围均优于常规组,从而进一步证明了3D打印技术的优势所在。此外,戚晓阳等[61]在应用3D打印技术制作的鹰嘴横形骨折模型上对克氏针进针角度进行生物力学研究,并测出角度为 10°时固定安全可靠。在伴有桡骨头骨折的处理方面,3D打印技术同样彰显其独特的优势,国外LUENAM等[62]使用由3D打印技术创建的特定桡骨头假体治疗无法修复的桡骨头骨折, Mayo 肘关节功能评分从术前20分升到85分,上肢功能障碍评分从术前88.33分降到28.33分。由此可见,3D打印技术作为一种临床辅助工具将会被更多地应用于OFDs的临床诊疗,使得OFDs术前准备工作进一步完善,并且通过术前模拟操作可为术中处理棘手问题打下良好的基础,提高手术效率,减少长时间手术给患者带来的影响。 "
| [1] O’DRISCOLL SW, JUPITER JB, COHEN MS, et al. Difficult elbow fractures: pearls and pitfalls. Instr Course Lect. 2003;52(1):113-134. [2] CHEN NC. Elbow Fractures with Instability Evaluation and Treatment Strategies. Hand Clin. 2018;34(1):75-83. [3] GERELI A, NALBANTOGLU U, DIKMEN G, et al. Fracture-dislocations of the proximal ulna. Acta Orthop Traumatol Turc. 2015;49(3):233-240. [4] YOON RS, TYAGI V, CANTLON MB, et al. Complex coronoid and proximal ulna fractures are we getting better at fixing these? Injury. 2016;47(10): 2053-2059. [5] RAO AJ, COHEN MS. The use of static external fixation for chronic instability of the elbow. J Shoulder Elbow Surg. 2019;28(8):e255-e264. [6] CHAN K, KING GJW, FABER KJ. Treatment of complex elbow fracture-dislocations. Curr Rev Musculoskelet Med. 2016;9(2):185-189. [7] SIEBENLIST S, BUCHHOLZ A, BRAUN KF. Fractures of the proximal ulna: current concepts in surgical management. EFORT Open Rev. 2019;4(1): 1-9. [8] GOTTLIEB M, SCHIEBOUT J. Elbow dislocations in the emergency department: a review of reduction techniques. J Emerg Med. 2018; 54(6):849-854. [9] ROBINSON PM, GRIFFITHS E, WATTS AC. Simple elbow dislocation. Shoulder Elbow. 2017;9(3):195-204. [10] HACKL M, LAPPEN S, NEISS WF, et al. The bare area of the proximal ulna: An anatomical study on optimizing olecranon osteotomy. Orthopade. 2016;5(10):887-894. [11] HANLON DP, MAVROPHILIPOS V. The Emergent Evaluation and Treatment of Elbow and Forearm Injuries. Emerg Med Clin North Am. 2020;38(1):81-102. [12] WEGMANN K, KNOWLES NK, LALONE EE, et al. The shape match of the olecranon tip for reconstruction of the coronoid process: influence of side and osteotomy angle. J Shoulder Elbow Surg. 2019;28(4):e117-e124. [13] WEGMANN K, KNOWLES N, LALONE E, et al. Computed Tomography Analysis of the Radial Notch of the Ulna. J Hand Surg Am. 2019; 44(9): 794.e1-794.e8. [14] BESER CG, DEMIRYUREK D, OZSOY H, et al. Redefining the proximal ulna anatomy. Surg Radiol Anat. 2014;36(10):1023-1031. [15] GIL JA, DASILVA K, JOHNSON E, et al. Three-dimensional characterization of trabecular bone mineral density of the proximal ulna using quantitative computed tomography. J Shoulder Elbow Surg. 2020;29(4):755-760. [16] AVASTHI A, PEACH C. Fractures of the proximal radius and ulna. Orthopaedics and Trauma. 2019;33(5):322-329. [17] THAYER MK, SWENSON AK, HACKETT DJ, et al. Classifications in Brief: Regan-Morrey Classification of Coronoid Fractures. Clin Orthop Relat Res. 2018;476(7):1540-1543. [18] SOUBEYRAND M, ASSABAH B, BEGIN M, et al. Pronation and supination of the hand: Anatomy and biomechanics. Hand Surg Rehabil. 2017; 36(1):2-11. [19] DUPARC F, MERLET MC. Prevention and management of early treatment failures in elbow injuries. Orthop Traumatol Surg Res. 2019; 105(1S):S75-S87. [20] 李红军,汪洁,刘永国,等.尺骨鹰嘴骨折-脱位伴桡骨头及冠状突骨折的手术治疗[J].中国修复重建外科杂志,2019,33(8):1045-1047. [21] IORDENS GI, VAN LIESHOUT EM, SCHEP NW, et al. Early mobilisation versus plaster immobilisation of simple elbow dislocations: results of the FuncSiE multicentre randomised clinical trial. Br J Sports Med. 2017;51(6):531-538. [22] 周智勇,陈旭,蒋协远.经鹰嘴肘关节骨折脱位的诊断与治疗[J].中华创伤骨科杂志,2012,14(4):342-345. [23] DELPONT M, LOUAHEM D, COTTALORDA J. Monteggia injuries. Orthop Traumatol Surg Res. 2018;104(1S):S113-S120. [24] ARAIN AR, HADDAD S, ANDERSON M, et al. Isolated pediatric transolecranon fracture-dislocation of the elbow managed nonoperatively: A case report and review of literature. Clin Case Rep. 2019;7(7):1435-1438. [25] WAKE H, HASHIZUME H, NISHIDA K, et al. Biomechanical analysis of the mechanism of elbow fracture-dislocations by compression force. J Orthop Sci. 2004;9(1):44-50. [26] RAO ZT, YUAN F, LI B, et al. Effect of elbow flexion angles on stress distribution of the proximal ulnar and radius bones under a vertical load: measurement using resistance strain gauges. J Orthop Surg Res. 2014;9:60. [27] KARBACH LE, ELFAR J. Elbow Instability: Anatomy, Biomechanics, Diagnostic Maneuvers, and Testing. J Hand Surg Am. 2017;42(2):118-126. [28] LUBBERTS B, JANSSEN S, MELLEMA J, et al. Quantitative 3-dimensional computed tomography analysis of olecranon fractures. J Shoulder Elbow Surg. 2016;25(5):831-836. [29] FENG D, ZHANG X, JIANG Y, et al. Plate fixation through an anterior approach for coronoid process fractures: A retrospective case series and a literature review. Medicine (Baltimore). 2018;97(36):e12041. [30] GATHEN M, JAENISCH M, PEEZ C, et al. Plate fixation and tension band wiring after isolated olecranon fracture comparison of outcome and complications. J Orthop. 2020;18(1):69-75. [31] PRIMEAU T, BEAUCHAMP-CHALIFOUR P, PELET S. Complex case of open fracture-dislocation of the elbow. Case Rep Orthop. 2019: 3495742. [32] SOCHOL KM, ANDELMAN SM, KOEHLER SM, et al. Treatment of Traumatic Elbow Instability With an Internal Joint Stabilizer. J Hand Surg Am. 2019;44(6):e161-e167. [33] SEO JB, YI HS, KIM KB, et al. Clinical outcomes of arthroscopic lateral ulnar collateral ligament repair with or without intra-articular fracture. J Orthop Surg (Hong Kong). 2020;28(1):2309499020908348. [34] GEBMANN J, KONIGSHAUSEN M, VON GLINSKI A, et al. Das chronisch dezentrierte Ellenbogengelenk. Obere Extremität. 2016;11(4):218-227. [35] KLUG A, BUSCHBECK S, GRAMLICH Y, et al. Good outcome using anatomically pre-formed buttress plates for anteromedial facet fractures of the coronoid-a retrospective study of twenty-four patients. Int Orthop. 2019;43(12):2817-2824. [36] 程宇,张志刚,徐耀增,等.前后联合入路治疗经鹰嘴肘关节骨折脱位[J].中华创伤骨科杂志,2016,18(7):630-633. [37] 苏朝阳,谭海涛,曾跃林,等.单一 Boyd 入路手术治疗经尺骨鹰嘴肘关节骨折脱位[J].中国骨与关节损伤杂志, 2019,34(7):758-760. [38] 胡晓川,向明,陈杭,等.前向鹰嘴骨折脱位的手术治疗[J].中国修复重建外科杂志,2012,26(12):1462-1465. [39] 郭永权.前后联合入路和肘关节后侧正中入路治疗经鹰嘴肘关节骨折脱位的效果比较[J].中国民康医学,2019,31(1):38-40. [40] NOWOTNY J, BISCHOFF F, AHLFELD T, et al. Biomechanical comparison of bi- and tricortical k-wire fixation in tension band wiring osteosynthesis. Eur J Med Res. 2019;24(1):33. [41] MIDTGAARD KS, SOREIDE E, BRATTGJERD JE, et al. Biomechanical comparison of tension band wiring and plate fixation with locking screws in transverse olecranon fractures. J Shoulder Elbow Surg. 2020. doi:10.1016/j.jse.2020.01.079.[Epub ahead of print] [42] GATHEN M, PLOEGER MM, PEEZ C, et al. Comparison of the Subjective Elbow Value with the DASH, MEPS und Morrey Score after Olecranon Fractures. Z Orthop Unfall. 2020;158(2):208-213. [43] ELLWEIN A, LILL H, WARNHOFF M, et al. Can low-profile double-plate osteosynthesis for olecranon fractures reduce implant removal? A retrospective multicenter study. J Shoulder Elbow Surg. 2020.29(6): 1275-1281. [44] SHEN JJ, QIU QM, GAO YB, et al. Direct anterior approach for mini plate fixation of Regan-Morrey type II comminuted ulnar coronoid process fracture. J Orthop Surg (Hong Kong). 2019;27(1):2309499018825223. [45] 冯伟楼,李树灏,张堃,等.前路钢板固定尺骨冠状突治疗复杂肘关节损伤[J]. 中国组织工程研究,2020,24(6):850-855. [46] MOON JG, ZOBITZ ME, AN KN, et al. Optimal screw orientation for fixation of coronoid fractures. J Orthop Trauma. 2009;23(4):277-280. [47] 杨如意,周雨,刘立峰,等.后内侧双钢板治疗复杂尺骨鹰嘴骨折的后内侧双钢板治疗复杂尺骨鹰嘴骨折的疗效观疗效观察[J]. 中国修复重建外科杂志, 2016,30(12):1462-1466. [48] 张继斌,张明义,刘恒.尺骨解剖板及钢丝治疗鹰嘴合并冠突骨折一例报告[J].中国骨与关节杂志,2017,6(4):318-320. [49] OZTURKMEN Y, SUKUR E, AKMAN YE, et al. Clinical and radiological evaluation of surgical management in olecranon fracture-dislocations. Musculoskelet Surg. 2019. doi:10.1007/s12306-019-00623-0. [Epub ahead of print] [50] EYBERG BA, MCKEE MD. Indications and Clinical Results of Radial Head Replacement: Has Anything Changed? J Orthop Trauma. 2019;33 Suppl 8:S1-S6. [51] REBGETZ PR, DANIELE L, UNDERHILL ID, et al. A biomechanical study of headless compression screws versus a locking plate in radial head fracture fixation. J Shoulder Elbow Surg. 2019;28(4):e111-e116. [52] GRUSZKA D, NOWAK TE, TKACZ T, et al. Complex radial head and neck fractures treated with modern locking plate fixation. J Shoulder Elbow Surg. 2019;28(6):1130-1138. [53] GIANNICOLA G, SESSA P, CALELLA P. Chronic complex persistent elbow instability: a consecutive and prospective case series and review of recent literature. J Shoulder Elbow Surg. 2020;29(4):e103-e117. [54] GIANNICOLA G, SACCHETTI FM, GRECO A, et al. Management of complex elbow instability. Musculoskeletal Surg. 2010;94(S1):25-36. [55] BIZ C, CRIMI A, BELLUZZI E, et al. Conservative Versus Surgical Management of Elbow Medial Ulnar Collateral Ligament Injury: A Systematic Review. Orthop Surg. 2019;11(6):974-984. [56] PIZZOLI A, BONDI M, SCHIRRU L, et al. The use of articulated external fixation for complex elbow trauma treatment. Musculoskelet Surg. 2019. doi:10.1007/s12306-019-00632-z. [Epub ahead of print] [57] TIZIANI S, DIENSTKNECHT T, OSTERHOFF G, et al. Standards for external fixation application: national survey under the auspices of the German Trauma Society. Int Orthop. 2019;43(8):1779-1785. [58] 朱涛,郑建平,杨勇. 铰链式外固定架在不稳定性肘关节损伤中的应用[J]. 宁夏医科大学学报, 2019,41(7):710-712. [59] HORAS K, HOFFMANN R, FAULENBACH M, et al. Advances in the Preoperative Planning of Revision Trauma Surgery Using 3D Printing Technology. J Orthop Trauma. 2020;34(5):e181-e186. [60] 姬文晨,蒋婉婷, 李嘉,等. 3D 打印联合Minmics 软件在肘关节骨折中的应用[J]. 山西医科大学学报,2019,50(5):680-684. [61] 戚晓阳,邱旭升,施鸿飞,等. 克氏针进针角度对尺骨鹰嘴横形骨折张力带固定稳定性的影响[J]. 中国骨与关节损伤杂志,2018, 33(11):1215-1217. [62] LUENAM S, KOSIYATRAKUL A, HANSUDEWECHAKUL C, et al. The Patient-Specific Implant Created with 3D Printing Technology in Treatment of the Irreparable Radial Head in Chronic Persistent Elbow Instability. Case Reports Orthop. 2018;2018:9272075. |
| [1] | Pu Rui, Chen Ziyang, Yuan Lingyan. Characteristics and effects of exosomes from different cell sources in cardioprotection [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(在线): 1-. |
| [2] | Hu Kai, Qiao Xiaohong, Zhang Yonghong, Wang Dong, Qin Sihe. Treatment of displaced intra-articular calcaneal fractures with cannulated screws and plates: a meta-analysis of 15 randomized controlled trials [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1465-1470. |
| [3] | Huang Dengcheng, Wang Zhike, Cao Xuewei. Comparison of the short-term efficacy of extracorporeal shock wave therapy for middle-aged and elderly knee osteoarthritis: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1471-1476. |
| [4] | Xu Feng, Kang Hui, Wei Tanjun, Xi Jintao. Biomechanical analysis of different fixation methods of pedicle screws for thoracolumbar fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1313-1317. |
| [5] | Jiang Yong, Luo Yi, Ding Yongli, Zhou Yong, Min Li, Tang Fan, Zhang Wenli, Duan Hong, Tu Chongqi. Von Mises stress on the influence of pelvic stability by precise sacral resection and clinical validation [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1318-1323. |
| [6] | Zhang Tongtong, Wang Zhonghua, Wen Jie, Song Yuxin, Liu Lin. Application of three-dimensional printing model in surgical resection and reconstruction of cervical tumor [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1335-1339. |
| [7] | Zhang Yu, Tian Shaoqi, Zeng Guobo, Hu Chuan. Risk factors for myocardial infarction following primary total joint arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1340-1345. |
| [8] | Wei Wei, Li Jian, Huang Linhai, Lan Mindong, Lu Xianwei, Huang Shaodong. Factors affecting fall fear in the first movement of elderly patients after total knee or hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1351-1355. |
| [9] | Wang Jinjun, Deng Zengfa, Liu Kang, He Zhiyong, Yu Xinping, Liang Jianji, Li Chen, Guo Zhouyang. Hemostatic effect and safety of intravenous drip of tranexamic acid combined with topical application of cocktail containing tranexamic acid in total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1356-1361. |
| [10] | Xiao Guoqing, Liu Xuanze, Yan Yuhao, Zhong Xihong. Influencing factors of knee flexion limitation after total knee arthroplasty with posterior stabilized prostheses [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1362-1367. |
| [11] | Huang Zexiao, Yang Mei, Lin Shiwei, He Heyu. Correlation between the level of serum n-3 polyunsaturated fatty acids and quadriceps weakness in the early stage after total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1375-1380. |
| [12] | Zhang Chong, Liu Zhiang, Yao Shuaihui, Gao Junsheng, Jiang Yan, Zhang Lu. Safety and effectiveness of topical application of tranexamic acid to reduce drainage of elderly femoral neck fractures after total hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1381-1386. |
| [13] | Wang Haiying, Lü Bing, Li Hui, Wang Shunyi. Posterior lumbar interbody fusion for degenerative lumbar spondylolisthesis: prediction of functional prognosis of patients based on spinopelvic parameters [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1393-1397. |
| [14] | Lü Zhen, Bai Jinzhu. A prospective study on the application of staged lumbar motion chain rehabilitation based on McKenzie’s technique after lumbar percutaneous transforaminal endoscopic discectomy [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1398-1403. |
| [15] | Chen Xinmin, Li Wenbiao, Xiong Kaikai, Xiong Xiaoyan, Zheng Liqin, Li Musheng, Zheng Yongze, Lin Ziling. Type A3.3 femoral intertrochanteric fracture with augmented proximal femoral nail anti-rotation in the elderly: finite element analysis of the optimal amount of bone cement [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1404-1409. |
| Viewed | ||||||||||||||||||||||||||||||||||||||||||||||||||
|
Full text 465
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||
|
Abstract 587
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||