Chinese Journal of Tissue Engineering Research ›› 2021, Vol. 25 ›› Issue (9): 1465-1470.doi: 10.3969/j.issn.2095-4344.3766
Previous Articles Next Articles
Treatment of displaced intra-articular calcaneal fractures with cannulated screws and plates: a meta-analysis of 15 randomized controlled trials
Hu Kai1, Qiao Xiaohong2, Zhang Yonghong3, Wang Dong3, Qin Sihe4
- 1Shanxi Medical University, Taiyuan 030001, Shanxi Province, China; 2Lüliang People’s Hospital Affiliated to Shanxi Medical University, Lüliang 033000, Shanxi Province, China; 3Department of Orthopedics, Second Hospital of Shanxi Medical University, Taiyuan 030001, Shanxi Province, China; 4Rehabilitation Hospital Affiliated to National Rehabilitation Auxiliary Research Center, Beijing 100176, China
-
Received:2020-04-03Revised:2020-04-11Accepted:2020-05-27Online:2021-03-28Published:2020-12-16 -
Contact:Qiao Xiaohong, MD, Chief physician, Lüliang People’s Hospital Affiliated to Shanxi Medical University, Lüliang 033000, Shanxi Province, China -
About author:Hu Kai, Master candidate, Shanxi Medical University, Taiyuan 030001, Shanxi Province, China
CLC Number:
Cite this article
Hu Kai, Qiao Xiaohong, Zhang Yonghong, Wang Dong, Qin Sihe. Treatment of displaced intra-articular calcaneal fractures with cannulated screws and plates: a meta-analysis of 15 randomized controlled trials[J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1465-1470.
share this article
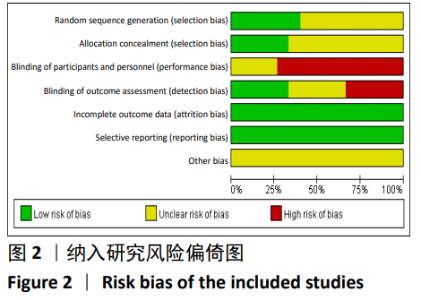
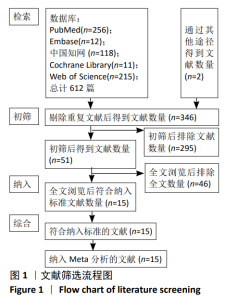
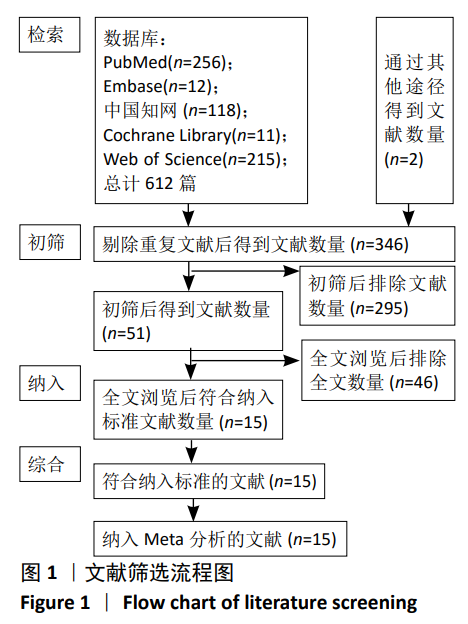
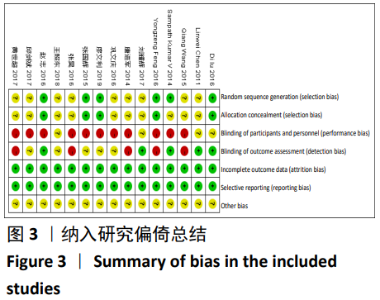
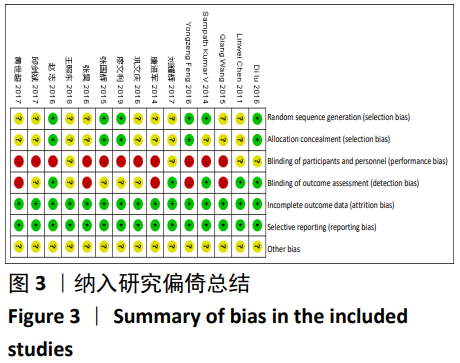
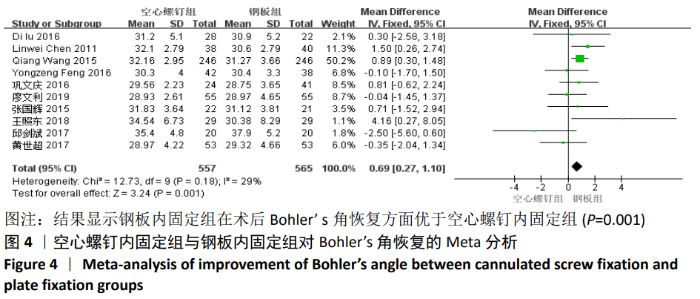
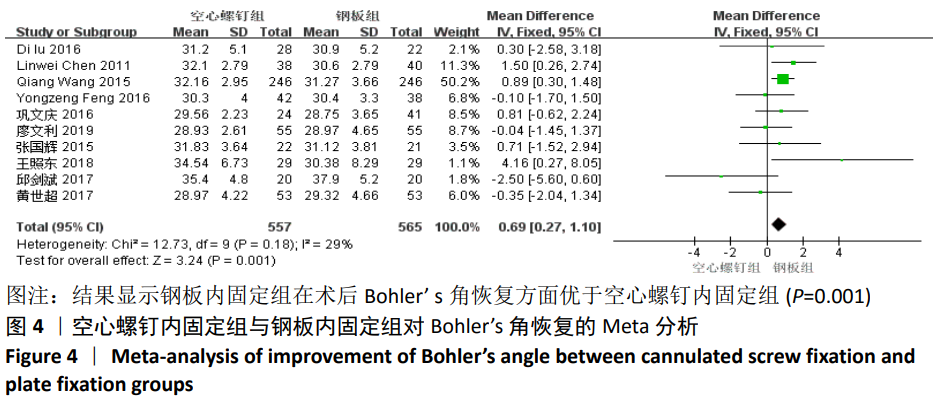
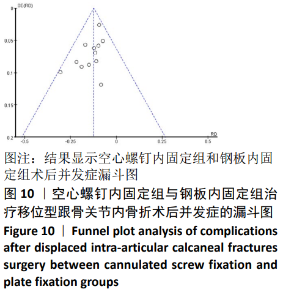
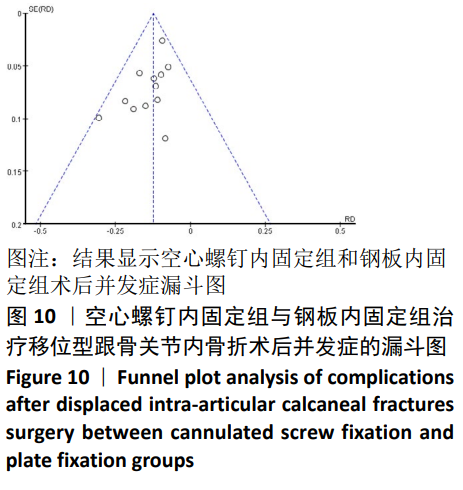
2.2 文献质量评价结果 根据Cochrane风险偏倚评价工具对纳入文献的质量进行评估包括是否随机、是否隐藏分组、受试者和研究者是否采用盲法、结局数据的完整性、对实验结果的选择性报告、其他偏倚风险等7个评价指标。纳入研究风险偏倚图,见图2。总体上看,纳入的文献存在一定的偏倚风险。其中6篇文献随机分组产生的评估为低风险[13,15-17,23,25],同时都进行了隐藏分组,文献质量较高,其他文献2个项目为不清楚。有4篇文献对受试者是否采用盲法不清楚外[11,16,18-19],其他文献都没有对受试者采用盲法,有5篇文献对研究者采用了盲法[11,13,16,19,23],有5篇文献对研究者是否采用了盲法不清楚[17-18,20,22,25],其他文献对研究者未采用盲法。"

| [1] EASTWOOD DM, GREGG PJ, ATKINS RM. Intra-articular fractures of the calcaneum. Part I: Pathological anatomy and classification. J Bone Joint Surg Br. 1993;75(2):183-188. [2] MITCHELL MJ, MCKINLEY JC, ROBINSON CM. The epidemiology of calcaneal fractures. Foot. 2009; 19(4):197-200. [3] POTER MQ, NUNLEY JA. Long-term functional outcomes after operative treatment for intra-articular fractures of the calcaneus. J Bone Joint Surg Am. 2009;91(8):1854-1860. [4] VAN TETERING EAA, BUCKLEY RE. Functional Outcome (SF-36) of Patients with Displaced Calcaneal Fractures Compared to SF-36 Normative Data. Foot Ankle Int. 2004;25(10):733-738. [5] GOTHA HE, ZIDE JR. Current controversies in management of calcaneus fractures. Orthop Clin North Am. 2017;48(1):91-103. [6] BUCKLEY R. OperatⅣe care did not benefit closed, displaced,intra-articular calcaneal fractures. J Bone Joint Surg Am. 2015;97(4):341. [7] SHARR PJ, MANGUPPLI MM, WINSON IG, et al. Current management options for displaced intra-articular calcaneal fractures: nonoperative, ORIF, minimally invasⅣe reduction and fixation or primary ORIF and subtalar arthrodesis. A contemporary review. Foot Ankle Surg. 2016; 22(1):1-8. [8] ABDELGAWAD AA, KANLIC E. Minimally invasive (sinus tarsi) approach for open reduction and internal fixation of intraarticular calcaneus fractures in children: surgical technique and case report of two patients. J Foot Ankle Surg. 2015; 54(1):135-139. [9] ARASTU M, SHEEHAN B, BUCKLEY R. Minimally invasive reduction and fixation of displaced calcaneal fractures: surgical technique and radiographic analysis. Int Orthop. 2014;38(3):539-545. [10] NOSEWICZ T, KNUPP M, BARG A, MASS M, et al. Mini-open sinus tarsi approach with percutaneous screw fixation of displaced calcaneal fractures. Foot Ankle Int. 2012;33(11):925-933. [11] CHEN L, ZHANG G, HONG J, et al. Comparison of percutaneous screw fixation and calcium sulfate cement grafting versus open treatment of displaced intra-articular calcaneal fractures. Foot Ankle Int. 2011;32(10):979-985. [12] WANG Q, LI X, SUN Y, et al. Comparison of the outcomes of two operational methods used for the fixation of calcaneal fracture. Cell Biochem Biophys. 2015;72(1):191-196. [13] SAMPATH KV, MARIMUTHU K, SUBRAMANI S, et al. Prospective randomized trial comparing open reduction and internal fixation with minimally invasive reduction and percutaneous fixation in managing displaced intra-articular calcaneal fractures. Int Orthop. 2014;38(12):2505-2512. [14] 唐进军.微创空心螺钉内固定与钢板内固定治疗跟骨骨折的临床思路构建[J].大家健康(学术版),2014,8(13):153-154. [15] FENG Y, SHUI X, WANG J, et al. Comparison of percutaneous cannulated screw fixation and calcium sulfate cement grafting versus minimally invasive sinus tarsi approach and plate fixation for displaced intra-articular calcaneal fractures: a prospective randomized controlled trial. BMC Musculoskeletal Disorders. BMC Musculoskelet Disord. 2016;17(1):288. [16] LU D, ZHU SY, YANG J, et al. A comparison of two minimally invasive procedures for intra-articular displaced calcaneal fractures in older children. Acta Orthop Belg. 2016;82(4):779-786. [17] 廖文利,何久盛,曹立峰.经皮撬拨复位空心螺钉与切开复位钢板内固定治疗Sanders Ⅱ、Ⅲ型跟骨骨折的比较[J].临床骨科杂志,2019, 22(4):492-495. [18] 王照东,官建中,吴敏,等.经皮撬拨复位空心螺钉内固定和切开复位钢板内固定治疗跟骨骨折疗效比较[J].淮海医药,2018,36(3):286-289. [19] 刘耀辉,李雪林,陈小微,等.跗骨窦小切口结合空心螺钉与L型切口结合钢板内固定治疗SandersⅢ型跟骨骨折疗效比较[J].世界复合医学,2017,3(4):9-12,16. [20] 邱剑斌.微创空心螺钉内固定及钢板内固定手术治疗40例跟骨骨折患者的临床效果评价[J].中外医学研究,2017,15(31):169-170. [21] 黄世超,倪锋,魏广奇,等.经皮撬拨复位空心螺钉与切开复位钢板内固定治疗SandersⅡ、Ⅲ型跟骨骨折疗效比较[J].中国临床研究, 2017,30(6):813-815. [22] 巩文庆,曹溢.微创撬拨复位空心拉力螺钉固定与钢板内固定治疗SandersⅡ型、Ⅲ型跟骨骨折的疗效分析[J].中国实用医药,2016, 11(33):4-6. [23] 赵志,吴敏,肖玉周,等.经皮撬拔空心钉固定与“L”型切口治疗跟骨骨折的临床疗效[J].中国矫形外科杂志,2016,24(6):495-499. [24] 张昊,张金金,张普,等.不同固定方法对跟骨骨折的临床治疗效果研究[J].黑龙江医药,2016, 29(1):112-113. [25] 张国辉.闭合复位空心螺钉固定与切开复位钢板固定治疗跟骨骨折临床疗效比较[J].海军医学杂志,2015,36(3):227-229. [26] COTTOM JM, BAKER JS. Restoring the anatomy of calcaneal fractures: a simple technique with radiographic review. Foot Ankle Spec. 2017;10(3): 235-239. [27] DIRANZO-GARCíA J, BERTó-MARTí X, CASTILLO-RUIPEREZ L, et al. Treatment of intraarticular calcaneal fractures by reconstruction plate. Results and complications of 86 fractures. Rev Esp Cir Ortop Traumatol. 2018. Doi: 10.1016/j.recot.2018.01.010. [28] HARVEY EJ, GRUJIC L, EARLY JS, et al. Morbidity associated with ORIF of intra-articular calcaneus fractures using a lateral approach. Foot Ankle Int. 2001;22:868-873. [29] PASTIDES PS, MILNES L, ROSENFELD PF. Percutaneous arthroscopic calcaneal osteosynthesis: a minimally invasive technique for displaced intra-articular calcaneal fractures. J Foot Ankle Surg. 2015;54(5):798-804. [30] 张青山,张蜀华.两种手术治疗Sanders Ⅱ型、Ⅲ型跟骨骨折的比较[J].实用骨科杂志, 2014, 20(6):515-519. [31] 李景光,陈先进,吕维宝,等.经皮撬拨复位空心螺钉与切开复位钢板内固定治疗 Sanders Ⅱ、Ⅲ型跟骨骨折的比较[J].中国矫形外科杂志,2016,24(16):1449-1455. [32] 王金辉.微创空心螺钉内固定和钢板内固定治疗跟骨骨折的临床观察[J].中国继续医学教育, 2016,8(11):165-166. [33] SMEREK JP, KADAKIA A, BELKOFF SM, et al. Percutaneous screw configuration versus perimeter plating of calcaneus fractures: a cadaver study. Foot Ankle Int. 2008;29(9):931-935. [34] ZHAO W, ZHANG Y. Comparison and predictive factors analysis for efficacy and safety of Kirschner wire, anatomical plate fixation and cannulated screw in treating patients with open calcaneal fractures. Medicine (Baltimore). 2019;98(43):e17498. [35] PENG Y, LIU J, ZHANG G, et al. Reduction and functional outcome of open reduction plate fixation versus minimally invasive reduction with percutaneous screw fixation for displaced calcaneus fracture: a retrospective study. J Orthop Surg Res. 2019;14(1):124. [36] NI M, WONG DWC, MEI J, et al. Biomechanical comparison of locking plate and crossing metallic and absorbable screws fixations for intraarticular calcaneal fractures. Sci China Life Sci. 2016;59(9):958-964. [37] ZHANG G, DING S, RUAN Z. Minimally invasive treatment of calcaneal fracture. J Int Med Res. 2019;47(8):3946-3954. . [38] VICENTI G, CARROZZO M, SOLARINO G, et al. Comparison of plate, calcanealplasty and external fixation in the management of calcaneal fractures. Injury. 2019;50 Suppl 4:S39-S46. [39] RAMMELT S, AMLANG M, BARTHEL S, et al. Percutaneous treatment of less severe intraarticular calcaneal fractures. Clin Orthop Relat Res. 2010;468(4):983-990. [40] STAPLETON JJ, ZGONIS T. Surgical Treatment of Intra-articular Calcaneal Fractures. Clin Podiatr Med Surg. 2014;31(4):539-546. [41] TOMASZ N, MARKUS K, ALEXEJ B, et al. Mini-open sinus tarsi approach with percutaneous screw fixation of displaced calcaneal fractures: a prospective computed tomography-based study. Foot Ankle Int. 2012;33(11):925-933. [42] PITTS CC, ALMAGUER A, WILSON JT, et al. Radiographic and postoperative outcomes of plate versus screw constructs in open reduction and internal fixation of calcaneus fractures via the sinus tarsi. Foot Ankle Int. 2019;40(8):929-935. [43] DEWALL M, HENDERSON CE, MCKINLEY TO, et al. Percutaneous reduction and fixation of displaced intra-articular calcaneus fractures. J Orthop Trauma. 2010;24(8):466-472. [44] DAWS SB, NEARY K, LUNDEEN G. Short-term radiographic outcomes of calcaneus fractures treated with 2-incision, minimally invasive approach. Foot Ankle Int. 2019;40(9):1060-1067. [45] TENNENT TD, CALDER PR, SALISBURY RD, et al. The operative management of displaced intra-articular fractures of the calcaneum: a two-centre study using a defined protocol. Injury. 2001;32(6):491-496. [46] JACQUOT F, ATCHABAHIAN A, et al. Balloon reduction and cement fixation in intra-articular calcaneal fractures: a percutaneous approach to intra-articular calcaneal fractures. Int Orthop. 2011;35(7):1007-1014. |
| [1] | Huang Dengcheng, Wang Zhike, Cao Xuewei. Comparison of the short-term efficacy of extracorporeal shock wave therapy for middle-aged and elderly knee osteoarthritis: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1471-1476. |
| [2] | Xu Feng, Kang Hui, Wei Tanjun, Xi Jintao. Biomechanical analysis of different fixation methods of pedicle screws for thoracolumbar fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1313-1317. |
| [3] | Jiang Yong, Luo Yi, Ding Yongli, Zhou Yong, Min Li, Tang Fan, Zhang Wenli, Duan Hong, Tu Chongqi. Von Mises stress on the influence of pelvic stability by precise sacral resection and clinical validation [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1318-1323. |
| [4] | Zhang Tongtong, Wang Zhonghua, Wen Jie, Song Yuxin, Liu Lin. Application of three-dimensional printing model in surgical resection and reconstruction of cervical tumor [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1335-1339. |
| [5] | Zhang Yu, Tian Shaoqi, Zeng Guobo, Hu Chuan. Risk factors for myocardial infarction following primary total joint arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1340-1345. |
| [6] | Wei Wei, Li Jian, Huang Linhai, Lan Mindong, Lu Xianwei, Huang Shaodong. Factors affecting fall fear in the first movement of elderly patients after total knee or hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1351-1355. |
| [7] | Wang Jinjun, Deng Zengfa, Liu Kang, He Zhiyong, Yu Xinping, Liang Jianji, Li Chen, Guo Zhouyang. Hemostatic effect and safety of intravenous drip of tranexamic acid combined with topical application of cocktail containing tranexamic acid in total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1356-1361. |
| [8] | Xiao Guoqing, Liu Xuanze, Yan Yuhao, Zhong Xihong. Influencing factors of knee flexion limitation after total knee arthroplasty with posterior stabilized prostheses [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1362-1367. |
| [9] | Huang Zexiao, Yang Mei, Lin Shiwei, He Heyu. Correlation between the level of serum n-3 polyunsaturated fatty acids and quadriceps weakness in the early stage after total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1375-1380. |
| [10] | Zhang Chong, Liu Zhiang, Yao Shuaihui, Gao Junsheng, Jiang Yan, Zhang Lu. Safety and effectiveness of topical application of tranexamic acid to reduce drainage of elderly femoral neck fractures after total hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1381-1386. |
| [11] | Wang Haiying, Lü Bing, Li Hui, Wang Shunyi. Posterior lumbar interbody fusion for degenerative lumbar spondylolisthesis: prediction of functional prognosis of patients based on spinopelvic parameters [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1393-1397. |
| [12] | Lü Zhen, Bai Jinzhu. A prospective study on the application of staged lumbar motion chain rehabilitation based on McKenzie’s technique after lumbar percutaneous transforaminal endoscopic discectomy [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1398-1403. |
| [13] | Chen Xinmin, Li Wenbiao, Xiong Kaikai, Xiong Xiaoyan, Zheng Liqin, Li Musheng, Zheng Yongze, Lin Ziling. Type A3.3 femoral intertrochanteric fracture with augmented proximal femoral nail anti-rotation in the elderly: finite element analysis of the optimal amount of bone cement [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1404-1409. |
| [14] | Du Xiupeng, Yang Zhaohui. Effect of degree of initial deformity of impacted femoral neck fractures under 65 years of age on femoral neck shortening [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1410-1416. |
| [15] | Zhang Shangpu, Ju Xiaodong, Song Hengyi, Dong Zhi, Wang Chen, Sun Guodong. Arthroscopic suture bridge technique with suture anchor in the treatment of acromioclavicular dislocation [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1417-1422. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||