Chinese Journal of Tissue Engineering Research ›› 2017, Vol. 21 ›› Issue (15): 2432-2437.doi: 10.3969/j.issn.2095-4344.2017.15.024
Previous Articles Next Articles
Clinical research of posterior femoral condylar offset
Xin Xing1, Qu Tie-bing2
- 1International Hospital, Peking University, Beijing 102206, China; 2China Rehabilitation Research Center-Beijing Bo’ai Hospital, Beijing 100068, China
-
Online:2017-05-28Published:2017-06-07 -
Contact:Qu Tie-bing, Chief physician, China Rehabilitation Research Center-Beijing Bo’ai Hospital, Beijing 100068, China -
About author:Xin Xing, Master, International Hospital, Peking University, Beijing 102206, China -
Supported by:the Special Fund for Public Welfare Industry Research of Ministry of Public Health, No. 201302007
CLC Number:
Cite this article
Xin Xing, Qu Tie-bing. Clinical research of posterior femoral condylar offset[J]. Chinese Journal of Tissue Engineering Research, 2017, 21(15): 2432-2437.
share this article
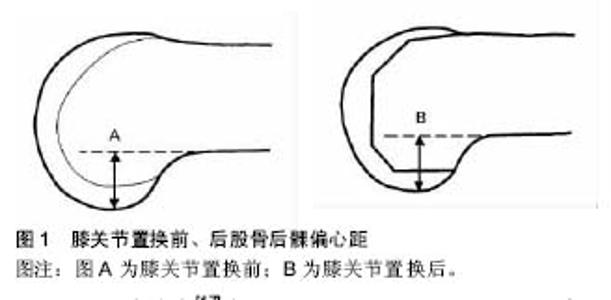
2.1 股骨后髁偏心距的测量 Bellemans等[11]学者在研究膝关节置换后膝关节最大屈曲度的影响因素时首次提出了股骨后髁偏心距的概念:在标准侧位片(股骨内外侧髁重叠位)上,股骨后髁最低点到股骨干远端后皮质切线的距离为股骨后髁偏心距(图1)[11]。其既往膝关节参数的测量方法可分为尸体解剖测量,二维影像学平片测量以及膝关节三维重建后测量几种。尸体测量准确度高,但资源稀缺,目前关于膝关节股骨后髁偏心距的测量暂无尸体数据报道。二维测量方法为:按照Bellemans等[11]学者在研究中要求,膝关节在拍摄平片时拍摄体位时要求股骨内外侧髁相互重叠。此方法存在以下缺点:①膝关节标准侧位片获取难度大;②不同时间段及不同患者摄片时难以统一膝关节的放大倍数。"
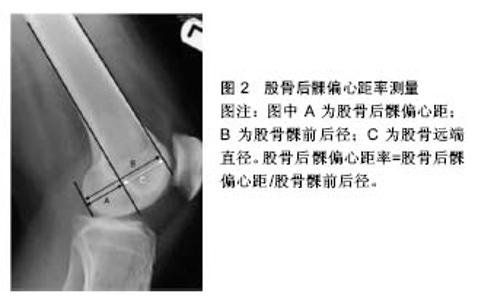
Johal等学者[17]在英国一所研究机构对100例正常志愿者的膝关节平片进行股骨后髁偏心距的测量,其结果为(28.10±2.27) mm,其中男性(29.01±2.04) mm、女性(27.19±2.15) mm。此外,部分学者将膝关节CT数据导入电脑辅助软件,然后在重建后的膝关节三维图像上测量,此方法测量股骨后髁偏心距具有以下优点:①轻松准确获得膝关节标准侧位图像;②避免膝关节普通X射线测量时放大倍数不统一[16-17]。王伟等[16]学者使用膝关节CT数据三维重建方法对100例正常中国人股骨后髁偏心距进行研究,其股骨后髁偏心距的结果平均值为(26.56±2.63) mm,其中男女性股骨后髁偏心距数值分别为(25.8±2.71) mm、(27.32±2.34) mm,男性与女性受试者股骨后髁偏心距存在显著差异。此外韩国全南国立大学医院的对100位受试志愿者股骨远端解剖学参数进行测量[16,19],其研究结果为股骨后髁偏心距男女性分别为(29.01±2.04) mm,(27.19±2.15) mm,男女之间测量数值在统计学上存在显著差异。此外王伟等[16]将研究中中国人股骨后髁偏心距的数据与其他学者的研究数据对比发现不同种族间股骨后髁偏心距存在显著差异。 此外,股骨后髁偏心距的定义为膝关节侧位平片上股骨内外侧髁重叠,这就默许了膝关节股骨后髁偏心距内外侧相同,然而Clarke等[20]学者研究发现正常膝关节股骨后髁软骨并非均匀分布,其研究发现膝关节股骨后内侧髁软骨厚度平均值为2.0 mm,后外侧髁软骨厚度平均值为 1.7 mm。同样地,Voleti等[21]学者通过膝关节MRI数据测量膝关节股骨后髁偏心距时也证实了该观点,研究结果发现股骨后内髁侧平均是后外侧髁厚度的1.12倍。 2.2 股骨后髁偏心距与股骨后髁偏心距率 2.2.1 股骨远端直径(distal femur dimension,DFD) 介绍股骨后髁偏心距率概念前,首先介绍一下股骨干远端直径。股骨干远端直径为标准侧位片上股骨干远端前后皮质切线之间的距离(图2),然而既往研究发现正常股骨存在10°左右前弓角[22],为了保证股骨远端测量数据的统一性,研究者测量股骨远端直径时选择距离股骨远端关节面约15 cm一段股骨作为测量样本,同时选择距离股骨远端关节面10 cm股骨皮质点做股骨前后皮质切线来计算股骨远端直径[11]。王伟等[16]研究结果为股骨远端直径(30.36±2.69) mm,其中男女性受试者测量数据分别为(31.78±2.20) mm、(28.94±2.38) mm,男女性之间具有显著差异。此外Johal等[17]学者研究结果为股骨远端直径均值为35.37 mm,男女性数据分别约为38.07 mm、 32.85 mm,男女之间股骨远端直径存在显著差异。由此可以推断股骨远端直径存在性别及种族间差异。 2.2.2 股骨后髁偏心距率(femoral condylar offset ratio,FCOR) 研究者利用膝关节平片进行股骨后髁偏心距测量时发现平片测量时存在不同程度的放大倍 数[15,23],此外,既往研究证实股骨后髁偏心距存在性别间差异,为了寻找一个较为稳定的参数来比较不同文献中以及膝关节置换手术前后股骨后髁偏心距的变化,Soda等[23]学者提出了股骨后髁偏心距的概念:股骨后髁偏心距/股骨远端前后径(FCO/ACP,图2)。王伟等[16]学者研究发现男女性受试者股骨后髁偏心距与股骨远端前后径都存在显著相关性(R²=0.472 3/0.422 6)。此外王伟学者的研究结果为中国志愿者膝关节股骨后髁偏心距率男性为(0.46±0.03),女性为(0.47±0.04),男女志愿者之间无显著差异。西方学者文献报道的股骨后髁偏心距率数据为男性(0.44±0.02),女性(0.45±0.02),男女之间无统计学差异[19]。Johal等[17]研究结果为男性股骨后髁偏心距率为0.44±0.02,女性为0.45±0.02。王伟、Johal及Seon 等[17,19]学者的研究结果发现性别之间股骨后髁偏心距率无显著差异,但不同种族间股骨后髁偏心距率存在显著统计学差异。鉴于膝关节实际内外侧股骨后髁偏心距存在差异,那么可以推断股骨后髁偏心距率也可能存在内外侧的差异,但目前暂无相关方面基础或临床研究。"

2.3 股骨后髁偏心距与胫骨平台后倾角 Ginotti等[18]在膝关节MRI对上测量股骨后髁偏心距与胫骨平台后倾角时发现胫骨平台后倾角与股骨外侧髁存在相关性(r²=0.127,p=0.001),但是未发现外侧股骨后髁偏心距与胫骨平台后倾角存在相关性(r²=0.01,p=0.829)。这可能和正常膝关节的解剖学特点及膝关节生物力学有关。因为既往研究发现正常膝关节内侧平台凹型的解剖特点和股骨内侧髁良好的形合度、胫骨内侧副韧带较外侧副韧带紧张度高以及膝关节“Medial-Pivot”运动模式都间接的体现出股骨内侧髁与胫骨内侧平台有着更为紧密的关系[24],而膝关节屈曲过程主要是股骨后髁与胫骨平台的接触,这可能是内侧胫骨平台与股骨后髁偏心距存在显著相关性原因。 综上所述,膝关节股骨远端测量参数存在性别或种族间差异,为了保证膝关节置换手术重建膝关节的初始生物力学,假体的设计应当重新考虑性别、种族间及内外侧髁间差异。 2.4 股骨后髁偏心距与膝关节最大屈曲度 既往关于股骨后髁偏心距与膝关节置换术后最大屈曲度相关性的研究结论却未能统一。 2002年Bellemans等[11]学者研究研究发现使用后交叉韧带韧带保留型假体膝关节置换后,股骨后髁偏心距与膝关节术后最大屈曲度存在相关性(R²=0.58,P < 0.001),研究进一步表明:①膝关节置换后股骨后髁偏心距每减少1 mm,膝关节关节活动度较术前平均减少6.1°;②术后股骨后髁偏心距重建减小3 mm以上,膝关节活动度将明显减少。2008年Arabori等[25]学者研究发现后交叉韧带保留型假体膝关节置换后股骨后髁偏心距与膝关节活动度相关。2009年Malviya等[15]学者的研究发现后交叉韧带保留型假体膝关节置换后12个月关节最大屈曲度与股骨后髁偏心距的差异存在相关性(R=0.69,P < 0.000 1),与后髁偏心距率的差异成显著相关(R=0.68,P < 0.000 1)。2015年王建涛等[26]学者发现股骨后髁偏心距在与后交叉韧带替代型假体膝关节置换后膝关节最大主动屈曲度存在相关性。 然而2010年Baeur等[1]学者研究发现股骨后髁偏心距与后交叉韧带替代型假体膝关节置换后膝关节最大屈曲度无相关性,甚至Ishil等[9]学者发现不论使用后交叉韧带替代还是保留型假体膝关节置换,股骨后髁偏心距与术后最大屈曲程度均无明确相关性。其原因可能为膝关节的活动度是众多因素综合作用的结果[15]。然而,尽管股骨后髁偏心距与膝关节置换后最大屈曲度相关性研究结果存在矛盾性,但是股骨后髁偏心距在维持膝关节置换术后高屈曲状态作用显著,以下为股骨后髁偏心距影响膝关节置换后最大屈曲度的机制。 2.4.1 胫骨平台-股骨后皮质撞击机制 Bellemans首次提出胫骨平台后缘与股骨后皮质的撞击是膝关节置换术后最大屈曲度的制约因素。增加股骨后髁偏心距可以延缓股骨-胫骨撞击从而增加膝关节屈曲度(图3)。这种机制被发现在正常膝关节及膝关节置换中。"

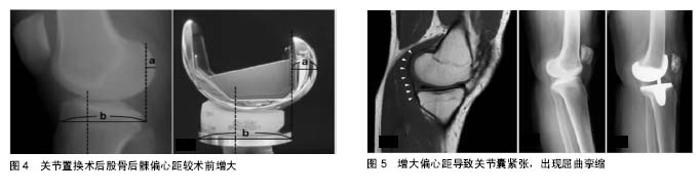
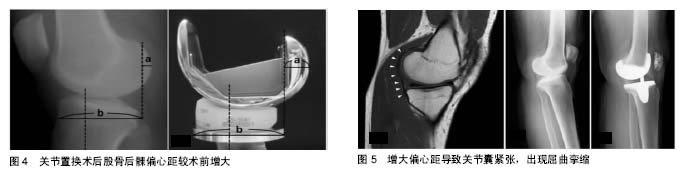
股骨后髁偏心距在保证正常膝关节高屈曲中状态中作用显著,既往许多学者对正常膝关节生物力学进行研究[27-32],其中Johal等[29]学者通过膝关节MRI观测到正常膝关节屈曲范围0°-120°时股骨后髁外旋20°,屈膝超过120°时股骨内外髁在胫骨平台等距后移,这两种机制可以延缓膝关节胫骨平台后缘与股股骨干远端后皮质的撞击,从而保证了正常膝关节高屈曲范围。此外Gungor等[33]的研究发现内外侧股髁骨前后径0.8 mm差异与股骨1°外旋显著相关(R²=0.645,P < 0.0001),因此正常膝关节屈膝时股骨后髁偏心距在股骨旋转中也有重要的作用。 南开大学医学机构的一项研究发现后交叉韧带替代型假体膝关节置换术后股骨后髁偏心距与膝关节最大屈曲度显著相关[26]。究其原因为,后交叉韧带替代型假体置换后膝关节屈曲时,股骨髁存在“rollback”机制[34],该机制可延缓胫骨-股骨撞击,提高膝关节置换术后关节最大屈曲度。此外其他学者的研究也发现使用后交叉韧带保留型假体置换,膝关节屈曲时也存在“Rollback”机制[18]。此外也有部分学者发现后交叉韧带替代型假体在屈膝时股骨髁在胫骨平台上的位置较后交叉韧带保留型假体靠后,导致胫骨-股骨撞击延迟,从而增加膝关节最大屈曲度。此外Fujimoto等[7]学者研究也证实后交叉韧带保留型假体膝关节置换时0°-90°胫骨股骨间隙的主要影响因素为股骨后髁偏心距,其原因为膝关节0°-90°的活动主要是由股骨后髁与胫骨平台的接触完成,较小的股骨后髁在屈膝时更容易发生胫骨后缘与股骨后皮质相撞,从而影响膝关节活动度。然而部分学者却未发现股骨后髁偏心距与膝关节最大屈曲度相关,Goldstein研究可能原因为,尽管后交叉韧带替代型假体存在“Rollback”机制,但是如果股骨后髁后方存在的骨赘阻止其“Rollback”,其假体优势可能就未能显现出来。 2.4.2 股骨后髁偏心距与术中关节间隙 Takayama 等[35]学者研究发现后交叉韧带保留型假体膝关节置换。 术中屈膝90°、120°时关节间隙大小与膝关节术后最大屈曲度相关,而Fujimoto等[27]学者研究证实了后交叉韧带保留型假体膝关节置换时0°-90°胫骨股骨间隙的主要影响因素为股骨后髁偏心距。此外Takayama等[35]研究还发现使用后交叉韧带保留型假体时如果屈曲间隙大于伸直间隙可以获得术后较好的最大屈曲度(R=0.41,p=0.013)。因为既往文献研究发现,屈曲间隙紧张时导致屈膝时胫骨假体上翘,撞击髌骨下极导致屈曲受限。然而Matsumoto等[14]学者研究发现使用后交叉韧带替代型假体膝关节置换时屈曲间隙小于伸直间隙时,术后可能会获得较好的膝关节屈曲度。 这可能提示使用后交叉韧带替代型假体进行膝关节置换时,术中应当恢复股骨原始后髁偏心距,然而使用后交叉韧带保留型假体进行膝关节置换时,术中可以适当的减小股骨后髁偏心距,以保证后交叉韧带功能能良好的发挥。 2.5 股骨后髁偏心距与膝关节屈曲挛缩 膝关节置换术的基本理念之一为等量截骨,然而既往研究发现使用不同类型假体,膝关节置换后股骨后髁偏心距存在不同程度的差异,Kim等[13]研究发现膝关节置换后股骨后髁偏心距平均增加3.3 mm,Johal等[17]学者研究CR普通假体及CR高屈曲假体膝关节置换后股骨后髁偏心距平均增加分别为1 mm,1.3 mm。术后股骨后髁偏心距的增加将导致髌骨填塞,而髌骨填塞将影响膝关节置换后功 能恢复,此外Onodera等[36]学者研究发现股骨后髁偏心距的增大将导致膝关节后方关节囊及软组织紧张,从而出现屈曲挛缩(图4,5),而既往研究已经明确屈曲挛缩将严重膝关节功能的恢复。另外如果术中通过加截股骨远端来纠正后方关节囊紧张导致的伸直间隙紧张将导致关节线上移,关节线的上移将可能导致髌股关节间压力增高、膝前痛,影响膝关节置换术后功能的恢复[37-38]。 "
| [1] Bauer T, Biau D, Colmar M,et al.Influence of posterior condylar offset on knee flexion after cruciate-sacrificing mobile-bearing total knee replacement: a prospective analysis of 410 consecutive cases. Knee. 2010;17(6): 375-380.[2] Ishikawa H, Saura R, Ohno O, et al.Long-term results of posterior release surgery for severe flexion contracture of the knee in patients with rheumatoid arthritis. Clin Orthop Relat Res.1991;(262):242-247.[3] Kettelkamp DB, Johnson RJ, Smidt GL, et al.An electrogoniometric study of knee motion in normal gait. J Bone Joint Surg Am.1970;52(4):775-790.[4] Tew M, Forster IW, Wallace WA. Effect of total knee arthroplasty on maximal flexion. Clin Orthop Relat Res. 1989;(247): 168-174.[5] Miner AL, Lingard EA, Wright EA, et al.Knee range of motion after total knee arthroplasty: how important is this as an outcome measure? J Arthroplasty.2003;18(3): 286-294.[6] Bellemans J, Robijns F, Duerinckx J, et al.The influence of tibial slope on maximal flexion after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc.2005;13(3): 193-196.[7] Fujimoto E, Sasashige Y, Masuda Y, et al.Significant effect of the posterior tibial slope and medial/lateral ligament balance on knee flexion in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc.2013;21(12):2704-2712.[8] Kim JH.Effect of posterior femoral condylar offset and posterior tibial slope on maximal flexion angle of the knee in posterior cruciate ligament sacrificing total knee arthroplasty. Knee Surg Relat Res.2013;25(2):54-59.[9] Ishii Y, Noguchi H, Takeda M, et al.Posterior condylar offset does not correlate with knee flexion after TKA. Clin Orthop Relat Res.2013;471(9): 2995-3001.[10] Geijsen GJ, Heesterbeek PJ, van Stralen G,et al.Do tibiofemoral contact point and posterior condylar offset influence outcome and range of motion in a mobile-bearing total knee arthroplasty? Knee Surg Sports Traumatol Arthrosc. 2014;22(3):550-555.[11] Bellemans J, Banks S, Victor J, et al. Fluoroscopic analysis of the kinematics of deep flexion in total knee arthroplasty. Influence of posterior condylar offset. J Bone Joint Surg Br. 2002;84(1):50-53.[12] Dennis DA, Komistek RD, Stiehl JB,et al.Range of motion after total knee arthroplasty: the effect of implant design and weight-bearing conditions.J Arthroplasty.1998; 13(7): 748-752.[13] Kim YH,Sohn KS,Kim JS.Range of motion of standard and high-flexion posterior stabilized total knee prostheses. A prospective, randomized study.J Bone Joint Surg Am.2005; 87(7): 1470-1475.[14] Matsumoto T, Mizuno K, Muratsu H, et al.Influence of intra-operative joint gap on post-operative flexion angle in osteoarthritis patients undergoing posterior-stabilized total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2007;15(8):1013-1018.[15] Malviya A, Lingard EA, Weir DJ, et al.Predicting range of movement after knee replacement: the importance of posterior condylar offset and tibial slope.Knee Surg Sports Traumatol Arthrosc.2009;17(5):491-498.[16] Wang W, Tsai TY, Yue B, et al.Posterior femoral condylar offsets of a Chinese population. Knee.2014;21(2): 553-556.[17] Johal P, Hassaballa MA, Eldridge JD, et al.The Posterior Condylar Offset Ratio. Knee.2012; 19(6):843-845.[18] Cinotti G, Sessa P, Ripani FR,et al.Correlation between posterior offset of femoral condyles and sagittal slope of the tibial plateau.J Anat.2012;221(5): 452-458.[19] Seon JK, Park JK, Shin YJ,et al.Comparisons of kinematics and range of motion in high-flexion total knee arthroplasty: cruciate retaining vs. substituting designs. Knee Surg Sports Traumatol Arthrosc.2011;19(12):2016-2022.[20] Clarke HD.Changes in posterior condylar offset after total knee arthroplasty cannot be determined by radiographic measurements alone. J Arthroplasty.2012; 27(6):1155- 1158.[21] Voleti PB, Stephenson JW, Lotke PA, et al.Plain radiographs underestimate the asymmetry of the posterior condylar offset of the knee compared with MRI. Clin Orthop Relat Res. 2014; 472(1):155-161.[22] Rubin PJ, Leyvraz PF, Aubaniac JM, et al.The morphology of the proximal femur. A three-dimensional radiographic analysis. J Bone Joint Surg Br.1992;74(1): 28-32.[23] Soda Y, Oishi J, Nakasa T, et al.New parameter of flexion after posterior stabilized total knee arthroplasty: posterior condylar offset ratio on X-ray photographs. Arch Orthop Trauma Surg.2007;127(3): 167-170.[24] Blaha J, Wojtys E. Motion and stability of the knee. In: Scott WN, ed. Surgery of the Knee. 4th ed. New York, NY: Churchill Livingstone; 2005:227-239.[25] Arabori M, Matsui N, Kuroda R, et al.Posterior condylar offset and flexion in posterior cruciate-retaining and posterior stabilized TKA. J Orthop Sci.2008;13(1):46-50.[26] Wang JT, Zhang Y, Liu Q, et al.Effect of posterior condylar offset on clinical results after posterior-stabilized total knee arthroplasty. Chin J Traumatol. 2015;18(5):259-266.[27] Hill PF, Vedi V, Williams A, et al.Tibiofemoral movement 2: the loaded and unloaded living knee studied by MRI.J Bone Joint Surg Br.2000;82(8): 1196-1198.[28] Iwaki H, Pinskerova V, Freeman MA. Tibiofemoral movement 1: the shapes and relative movements of the femur and tibia in the unloaded cadaver knee. J Bone Joint Surg Br.2000; 82(8): 1189-1195.[29] Johal P, Williams A, Wragg P,et al.Tibio-femoral movement in the living knee. A study of weight bearing and non-weight bearing knee kinematics using 'interventional' MRI. J Biomech. 2005;38(2):269-276.[30] Nakagawa S, Kadoya Y, Todo S, et al.Tibiofemoral movement 3: full flexion in the living knee studied by MRI.J Bone Joint Surg Br.2000;82(8):1199-1200.[31] Williams A, Logan M.Understanding tibio-femoral motion. Knee. 2004;11(2): 81-88.[32] Karrholm J, Brandsson S, Freeman MA. Tibiofemoral movement 4 changes of axial tibial rotation caused by forced rotation at the weight-bearing knee studied by RSA. J Bone Joint Surg Br. 2000;82(8):1201-1203.[33] Gungor HR, Ok N, Agladioglu K, et al.Significance of asymmetrical posteromedial and posterolateral femoral condylar chamfer cuts in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc.2014;22(12): 2989-2994.[34] Dennis DA, Komistek RD, Colwell CE Jr, et al.In vivo anteroposterior femorotibial translation of total knee arthroplasty: a multicenter analysis.Clin Orthop Relat Res. 1998(356):47-57.[35] Takayama K, Matsumoto T, Kubo S, et al.Influence of intra-operative joint gaps on post-operative flexion angle in posterior cruciate-retaining total knee arthroplasty. Knee Surgery, Sports Traumatology, Arthroscopy.2011;20(3): 532-537.[36] Onodera T, Majima T, Nishiike O,et al.Posterior femoral condylar offset after total knee replacement in the risk of knee flexion contracture. J Arthroplasty. 2013; 28(7): 1112-1126.[37] Babazadeh S, Dowsey MM, Swan JD, et al.Joint line position correlates with function after primary total knee replacement: a randomised controlled trial comparing conventional and computer-assisted surgery. J Bone Joint Surg Br.2011;93(9): 1223-1231.[38] König C, Sharenkov A, Matziolis G, et al.Joint line elevation in revision TKA leads to increased patellofemoral contact forces. J Orthop Res. 2010;28(1):1-5. |
| [1] | Wang Jianping, Zhang Xiaohui, Yu Jinwei, Wei Shaoliang, Zhang Xinmin, Xu Xingxin, Qu Haijun. Application of knee joint motion analysis in machanism based on three-dimensional image registration and coordinate transformation [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(在线): 1-5. |
| [2] | Xu Xinzhong, Wu Zhonghan, Yu Shuisheng, Zhao Yao, Xu Chungui, Zhang Xin, Zheng Meige, Jing Juehua. Biomechanical analysis of different ways of inserting Steinmann Pins into the femoral head [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1313-1317. |
| [3] | Wei Guoqiang, Li Yunfeng, Wang Yi, Niu Xiaofen, Che Lifang, Wang Haiyan, Li Zhijun, Shi Guopeng, Bai Ling, Mo Kai, Zhang Chenchen, Xu Yangyang, Li Xiaohe. Biomechanical analysis of non-uniform material femur under different loads [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1318-1322. |
| [4] | Zhang Jichao, Dong Yuefu, Mou Zhifang, Zhang Zhen, Li Bingyan, Xu Xiangjun, Li Jiayi, Ren Meng, Dong Wanpeng. Finite element analysis of biomechanical changes in the osteoarthritis knee joint in different gait flexion angles [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1357-1361. |
| [5] | Yao Xiaoling, Peng Jiancheng, Xu Yuerong, Yang Zhidong, Zhang Shuncong. Variable-angle zero-notch anterior interbody fusion system in the treatment of cervical spondylotic myelopathy: 30-month follow-up [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1377-1382. |
| [6] | Zhuang Zhikun, Wu Rongkai, Lin Hanghui, Gong Zhibing, Zhang Qianjin, Wei Qiushi, Zhang Qingwen, Wu Zhaoke. Application of stable and enhanced lined hip joint system in total hip arthroplasty in elderly patients with femoral neck fractures complicated with hemiplegia [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1429-1433. |
| [7] | Zhang Lichuang, Xu Hao, Ma Yinghui, Xiong Mengting, Han Haihui, Bao Jiamin, Zhai Weitao, Liang Qianqian. Mechanism and prospects of regulating lymphatic reflux function in the treatment of rheumatoid arthritis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1459-1466. |
| [8] | Wu Bingshuang, Wang Zhi, Tang Yi, Tang Xiaoyu, Li Qi. Anterior cruciate ligament reconstruction: from enthesis to tendon-to-bone healing [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1293-1298. |
| [9] | An Weizheng, He Xiao, Ren Shuai, Liu Jianyu. Potential of muscle-derived stem cells in peripheral nerve regeneration [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1130-1136. |
| [10] | Zhang Jinglin, Leng Min, Zhu Boheng, Wang Hong. Mechanism and application of stem cell-derived exosomes in promoting diabetic wound healing [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1113-1118. |
| [11] | Liu Dongcheng, Zhao Jijun, Zhou Zihong, Wu Zhaofeng, Yu Yinghao, Chen Yuhao, Feng Dehong. Comparison of different reference methods for force line correction in open wedge high tibial osteotomy [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 827-831. |
| [12] | Shao Yangyang, Zhang Junxia, Jiang Meijiao, Liu Zelong, Gao Kun, Yu Shuhan. Kinematics characteristics of lower limb joints of young men running wearing knee pads [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 832-837. |
| [13] | Huang Hao, Hong Song, Wa Qingde. Finite element analysis of the effect of femoral component rotation on patellofemoral joint contact pressure in total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 848-852. |
| [14] | Li Shuo, Su Peng, Zhang Li, Wu Qiulong, Hu Xiangyu, Lai Yuliang. Positive effect of supracondylar femoral osteotomy on the correction of knee varus based on three-dimensional reconstruction and finite element analysis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 858-863. |
| [15] | Yuan Jing, Sun Xiaohu, Chen Hui, Qiao Yongjie, Wang Lixin. Digital measurement and analysis of the distal femur in adults with secondary knee valgus deformity [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 881-885. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||