Chinese Journal of Tissue Engineering Research ›› 2016, Vol. 20 ›› Issue (46): 6963-6969.doi: 10.3969/j.issn.2095-4344.2016.46.017
Previous Articles Next Articles
Correlation of osteoblasts and osteoclasts with alcohol-induced femoral head necrosis: a new strategy of prevention and target therapy
Chen Jun-yu1, 2, Wang Jian-zhong1, 2
- 1Inner Mongolia Medical University, Hohhot 010030, Inner Mongolia Autonomous Region, China; 2First Department of Traumatology, the Second Affiliated Hospital of Inner Mongolia Medical University, Hohhot 010030, Inner Mongolia Autonomous Region, China
-
Received:2016-09-04Online:2016-11-11Published:2016-11-11 -
Contact:Wang Jian-zhong, M.D., Chief physician, Inner Mongolia Medical University, Hohhot 010030, Inner Mongolia Autonomous Region, China; First Department of Traumatology, the Second Affiliated Hospital of Inner Mongolia Medical University, Hohhot 010030, Inner Mongolia Autonomous Region, China -
About author:Chen Jun-yu, Studying for master’s degree, Inner Mongolia Medical University, Hohhot 010030, Inner Mongolia Autonomous Region, China; First Department of Traumatology, the Second Affiliated Hospital of Inner Mongolia Medical University, Hohhot 010030, Inner Mongolia Autonomous Region, China -
Supported by:the National Natural Science Foundation of China, No. 81160228
CLC Number:
Cite this article
Chen Jun-yu, Wang Jian-zhong. Correlation of osteoblasts and osteoclasts with alcohol-induced femoral head necrosis: a new strategy of prevention and target therapy[J]. Chinese Journal of Tissue Engineering Research, 2016, 20(46): 6963-6969.
share this article
2.1 酒精性股骨头坏死及其病理学基础 2.1.1 酒精性股骨头坏死概述 股骨头坏死患者中有10%)74%是由于长期大量饮酒造成的,即酒精性股骨头坏死[14-18]。酒精性股骨头坏死是一种难治性非创伤性股骨头坏死。该病的发生主要由于长期大量饮酒造成脂代谢异常,骨髓间充质干细胞分化成骨细胞及破骨细胞异常,从而造成骨吸收与骨形成的动态平衡紊乱,最终导致股骨头缺血坏死[19-20]。随着饮酒已成为一个全球性的危害人体健康的因素,世界卫生组织(WHO)指出大量酗酒是酒精性股骨头坏死的重要发病因素之一,而且在世界范围内其发病率呈上升趋势,其患病人数占非创伤性股骨头坏死的比重也越来越大,北京积水潭医院在1996)2000年间对306例成人非创伤性股骨头坏死调研发现其中46%是由过量饮酒引起的,超过激素引起的股骨头坏死(占34%)[21]。早期酒精性股骨头坏死患者常感患肢无力,髋关节疼痛,慢性钝痛或剧痛,夜间和劳累加重,可放射到膝关节、大腿内侧、腹股沟等;到了中晚期酒精性股骨头坏死时,患者出现髋关节功能活动受限,以外展、内旋及屈曲等功能主。下蹲、穿鞋困难、行走步幅小、跛行、4字实验、托马氏征阳性及患侧下肢肌肉萎缩。治疗不及时者最终发生股骨头缺血性坏死且一旦发生很难逆转。 2.1.2 酒精性股骨头坏死的病理学变化 酒精性股骨头坏死的病理学变化是由多种因素综合作用的结果,已熟知的有关酒精性股骨头坏死的病理机制如脂质代谢紊乱,骨质疏松,凝血异常,脂肪栓塞,骨内高压,骨细胞脂肪变性,骨髓基质细胞成脂分化及骨代谢等假说[22],且假说中多涉及酒精所引起的脂肪代谢紊乱为主的病理过程。随着细胞生物学的不断深入研究,从细胞生物学及细胞代谢角度分析,该病的病理过程可概括为:大量的酒精摄入导致血脂代谢异常、股骨头髓内脂肪细胞增殖,引起脂肪细胞分化增加及变性坏死并沉积于股骨头软骨下的骨细胞内;另外,酒精刺激使骨髓间充质干细胞分化成骨细胞异常,则会影响体内成骨/破骨细胞紊乱,影响破骨细胞介导的骨吸收与成骨细胞介导的骨形成过程,影响死骨清除与骨组织重建进程,引起骨循环中断、骨的活性成分死亡及随后修复的一系列复杂病理过程,进而导致骨小梁断裂,股骨头关节软骨进行性塌陷,股骨头血液灌注量减少,引发股骨头坏死[19-20]。 2.2 成骨细胞、破骨细胞及其在骨代谢中的生物学功能 成骨细胞与破骨细胞是骨重建过程中的两种主要细胞,二者相互作用、相互影响,调节成骨细胞与破骨细胞的生成比例与生物活性,调控骨吸收与骨形成的动态平衡,影响骨代谢。 2.2.1 成骨细胞及其生物学功能 成骨细胞,即可产生骨质或基质的细胞,是参与骨形成和骨坏死后修复的主要功能细胞。成骨细胞在骨组织的生长发育、骨代谢动态平衡、骨形成、及骨损伤后的重建修复过程中都起重要作用,是参与骨形成的关键细胞,见图2。成骨细胞在骨形成过程中要经历4个阶段,即细胞增殖分化、细胞外基质成熟、细胞外基质矿化和细胞凋亡,尤其以成骨细胞分化为骨发生与骨形成、骨重建的前提。其主要的生物学功能可概括为以下3点:①负责骨基质的合成、分泌及矿化;②调控破骨细胞的骨吸收功能;③与破骨细胞共同维持骨代谢平衡。"
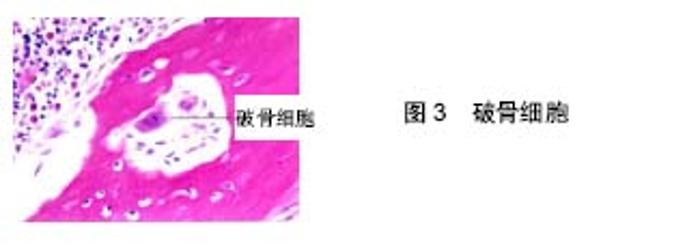
成骨细胞的来源是多源的,据可靠研究证明,颅骨或胚胎颅骨、骨膜源性细胞及间充质干细胞都具有很强的分化成骨细胞的能力[23-27],其中以间充质干细胞的分化为主要来源。使用光镜或者电镜可以观察到成骨细胞的主要形态学特征:在光镜下成骨细胞一般呈现出锥形、圆形或立方形,细而短的突起从成骨细胞伸出与邻近的细胞相连,细胞核大而圆且位于细胞的一端,线粒体形态细长且分散存在于细胞浆内;在电镜下,粗面内质网基本占据了成骨细胞的包浆,形成一个由核糖体附着的膜状管形物。正常情况下,圆形或细长的线粒体黏附于粗面内质网上且部分线粒体中含有矿化小粒。 2.2.2 破骨细胞及其生物学功能 破骨细胞又称为骨吸收细胞(bone-resorbing cells),是骨组织成分的一种,行使骨吸收的功能。破骨细胞属于单核巨噬细胞,其细胞内有2-20个不等的细胞核,但多数情况下每个细胞内含有10-20个细胞核。此外, 破骨细胞内含有大量溶酶体、广泛分布于近核区的高尔基体、众多游离的核糖体与少量的粗面内质网,还有伪足及突起的形态不规则的细胞,见图3。在电镜下观察可发现破骨细胞的褶皱膜含有很多构成完全不同的亚结构,这些亚结构相互作用配合,保证破骨细胞介导的骨吸收过程的顺利进行[28]。破骨细胞是人体惟一具有溶解骨组织能力的细胞,在骨重建中有重要作用。高表达抗酒石酸酸性磷酸酶和组织蛋白酶K是破骨细胞的主要标志。破骨细胞的起源与成骨细胞完全不同,是由起源于骨髓造血系统的特定的破骨细胞前体在趋化因子的作用下进入血液循环,到达处于骨吸收状态的骨组织部位,即骨重建单位时,在一系列趋化因子与细胞因子的作用下进入骨组织并分化成为成熟的破骨细胞。其介导的骨吸收功能在人体骨组织重建、维持骨骼系统完整性、骨组织内矿物质稳态及维持骨代谢平衡中均发挥关键作用。此外,破骨细胞还与局部性或者全身性骨质疏松、坏死有关。"
| [1] uo W, Sun W, Zhao D, et al. Investigating Clinical Failure of Bone Grafting through a Window at the Femoral Head Neck Junction Surgery for the Treatment of Osteonecrosis of the Femoral Head. PLoS One. 2016;11(6): e0156903. [2] Glueck CJ, Freiberg RA, Sieve L, et al. Enoxaparin prevents progression of stages I and II osteonecrosis of the hip. Clin Orthop Relat Res. 2005;(435): 164-170. [3] Mont MA, Jones LC, Hungerford DS. Nontraumatic osteonecrosis of the femoral head: ten years later. J Bone Joint Surg Am. 2006;88(5): 1117-1132. [4] Hirata T, Fujioka L, Takahashi KA, et al. Low molecular weight phenotype of Apo(a) is a risk factor of corticosteroid-induced osteonecrosis of the femoral head after renal transplant. J Rheumatol. 2007;34(3): 516-522. [5] Jones LC, Mont MA, Le TB, et al. Procoagulants and osteonecrosis. J Rheumatol. 2003;30(4): 783-791. [6] Wang BL, Yue DB, Liu BX, et al. Quality of sexual life after total hip arthroplasty in male patients with osteonecrosis of femoral head. Eur J Orthop Surg Traumatol. 2014;24(7): 1217-1221. [7] Mont MA, Marulanda GA, Jones LC, et al. Systematic analysis of classification systems for osteonecrosis of the femoral head. J Bone Joint Surg Am. 2006;88 Suppl 3:16-26. [8] Gagala J, Buraczynska M, Mazurrkiewicz T, et al. Endothelial nitric oxide synthase gene intron 4 polymorphism in non-traumatic osteonecrosis of the femoral head. Int Orthop. 2013;37(7):1381-1385. [9] 李子荣.科学诊断和治疗股骨头坏死[J].中国修复重建外科杂志, 2005,19(9): 685-686. [10] 王义生,张春霖,王利民,等.双支撑骨柱移植术治疗成人晚期股骨头缺血性坏死(附22例报告)[J].中华骨科杂志, 1995,15(9): 584-587. [11] Fukushima W, Fujioka M, Kubo T, et al. Nationwide epidemiologic survey of idiopathic osteonecrosis of the femoral head. Clin Orthop Relat Res. 2010;468(10): 2715-2724. [12] Kang JS, Park S, Song JH, et al. Prevalence of osteonecrosis of the femoral head: a nationwide epidemiologic analysis in Korea. J Arthroplasty. 2009; 24(8): 1178-1183. [13] Jones JP Jr. Concepts of etiology and early pathogenesis of osteonecrosis. Instr Course Lect. 1994;43: 499-512. [14] Agarwal R, Gupta R, Singh S, et al. Avascular necrosis of humeral head in an elderly patient with tuberculosis: a case report. J Med Case Rep. 2008;2: 361. [15] Lee JS, Lee JS, Roh HL, et al. Alterations in the differentiation ability of mesenchymal stem cells in patients with nontraumatic osteonecrosis of the femoral head: comparative analysis according to the risk factor. J Orthop Res. 2006;24(4): 604-609. [16] Wang Y, Yin L, Li Y, et al. Preventive effects of puerarin on alcohol-induced osteonecrosis. Clin Orthop Relat Res. 2008;466(5): 1059-1067. [17] Suh KT, Kim SM, Roh HL, et al. Decreased osteogenic differentiation of mesenchymal stem cells in alcohol-induced osteonecrosis. Clin Orthop Relat Res. 2005;(431): 220-225. [18] Moon JG, Shetty GM, Biswal S, et al. Alcohol-induced multifocal osteonecrosis: a case report with 14-year follow-up. Arch Orthop Trauma Surg. 2008;128(10): 1149-1152. [19] Seamon J, Keller T, Saleh J, et al. The pathogenesis of nontraumatic osteonecrosis. Arthritis. 2012;2012: 601763. [20] Okazaki S, Nagoya S, Tateda K, et al. Experimental rat model for alcohol-induced osteonecrosis of the femoral head. Int J Exp Pathol. 2013; 94(5): 312-319. [21] Wang Y, Li Y, Mao K, et al. Alcohol-induced adipogenesis in bone and marrow: a possible mechanism for osteonecrosis. Clin Orthop Relat Res. 2003;(410):213-224. [22] Mont MA, Einhorn TA, Sponseller PD, et al. The trapdoor procedure using autogenous cortical and cancellous bone grafts for osteonecrosis of the femoral head. J Bone Joint Surg Br. 1998;80(1): 56-62. [23] Declercq H, Van den Vreken N, De Maeyer E, et al. Isolation, proliferation and differentiation of osteoblastic cells to study cell/biomaterial interactions: comparison of different isolation techniques and source. Biomaterials. 2004;25(5): 757-768. [24] Ng AM, Saim AB, Tan KK, et al. Comparison of bioengineered human bone construct from four sources of osteogenic cells. J Orthop Sci.2005; 10(2): 192-199. [25] Cowan CM, Shi YY, Aalami OO, et al. Adipose-derived adult stromal cells heal critical-size mouse calvarial defects. Nat Biotechnol. 2004; 22(5): 560-507. [26] Wan DC, Siedhoff MT, Kwan MD, et al. Refining retinoic acid stimulation for osteogenic differentiation of murine adipose-derived adult stromal cells. Tissue Eng. 2007;13(7): 1623-1631. [27] Wan C, He Q, Li G. Allogenic peripheral blood derived mesenchymal stem cells (MSCs) enhance bone regeneration in rabbit ulna critical-sized bone defect model. J Orthop Res. 2006;24(4): 610-618. [28] Mulari MT, Zhao H, Lakkakorpi PT, et al. Osteoclast ruffled border has distinct subdomains for secretion and degraded matrix uptake. Traffic. 2003;4(2): 113-125. [29] Deal C. Potential new drug targets for osteoporosis. Nat Clin Pract Rheumatol. 2009;5(1): 20-27. [30] Atanga E, Dolder S, Dauwalder T, et al. TNFalpha inhibits the development of osteoclasts through osteoblast-derived GM-CSF. Bone. 2011;49(5): 1090-1100. [31] Park H, No AL, Lee JM, et al. PDE4 inhibitor upregulates PTH-induced osteoclast formation via CRE-mediated COX-2 expression in osteoblasts. FEBS Lett. 2010;584(1): 173-180. [32] 杨德鸿,金大地,陈建庭,等.共育体系中成骨细胞和破骨细胞生物学特性观察[J].中华骨科杂志, 2001,21(11): 32-36. [33] 刘文佳,王晓庚,周洪,等.体外大鼠成骨细胞对破骨细胞形成的影响[J].西安交通大学学报(医学版), 2008,29(3): 281-284. [34] Lee SW, Kwak HB, Chung WJ, et al. Participation of protein kinase C beta in osteoclast differentiation and function. Bone. 2003;32(3): 217-227. [35] 张立智,张先龙,王琦,等.骨关节炎软骨下骨的成骨细胞生物学表型研究[J].第三军医大学学报, 2011,33(10): 1003-1007. [36] Wang Y, Cao Y, Li Y, et al. Genetic association of the ApoB and ApoA1 gene polymorphisms with the risk for alcohol-induced osteonecrosis of femoral head. Int J Clin Exp Pathol. 2015;8(9): 11332-11339. [37] Odkhuu E, Koide N, Haque A, et al. Inhibition of receptor activator of nuclear factor-kappaB ligand (RANKL)- induced osteoclast formation by pyrroloquinoline quinine (PQQ). Immunol Lett. 2012;142(1-2): 34-40. [38] Roohani-Esfahani SI, No YJ, Lu Z, et al. A bioceramic with enhanced osteogenic properties to regulate the function of osteoblastic and osteocalastic cells for bone tissue regeneration. Biomed Mater. 2016; 11(3): 035018. |
| [1] | Zhang Tongtong, Wang Zhonghua, Wen Jie, Song Yuxin, Liu Lin. Application of three-dimensional printing model in surgical resection and reconstruction of cervical tumor [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1335-1339. |
| [2] | Chen Jiming, Wu Xiaojing, Liu Tianfeng, Chen Haicong, Huang Chengshuo. Effects of silymarin on liver injury and bone metabolism induced by carbon tetrachloride in mice [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1224-1228. |
| [3] | Geng Qiudong, Ge Haiya, Wang Heming, Li Nan. Role and mechanism of Guilu Erxianjiao in treatment of osteoarthritis based on network pharmacology [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1229-1236. |
| [4] | Zeng Yanhua, Hao Yanlei. In vitro culture and purification of Schwann cells: a systematic review [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1135-1141. |
| [5] | Li Shibin, Lai Yu, Zhou Yi, Liao Jianzhao, Zhang Xiaoyun, Zhang Xuan. Pathogenesis of hormonal osteonecrosis of the femoral head and the target effect of related signaling pathways [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 935-941. |
| [6] | Zheng Xiaolong, He Xiaoming, Gong Shuidi, Pang Fengxiang, Yang Fan, He Wei, Liu Shaojun, Wei Qiushi. Bone turnover characteristics in patients with alcohol-induced osteonecrosis of the femoral head [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 657-661. |
| [7] | Xu Dongzi, Zhang Ting, Ouyang Zhaolian. The global competitive situation of cardiac tissue engineering based on patent analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 807-812. |
| [8] | Wu Zijian, Hu Zhaoduan, Xie Youqiong, Wang Feng, Li Jia, Li Bocun, Cai Guowei, Peng Rui. Three-dimensional printing technology and bone tissue engineering research: literature metrology and visual analysis of research hotspots [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 564-569. |
| [9] | Chang Wenliao, Zhao Jie, Sun Xiaoliang, Wang Kun, Wu Guofeng, Zhou Jian, Li Shuxiang, Sun Han. Material selection, theoretical design and biomimetic function of artificial periosteum [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 600-606. |
| [10] | Liu Fei, Cui Yutao, Liu He. Advantages and problems of local antibiotic delivery system in the treatment of osteomyelitis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 614-620. |
| [11] | Li Xiaozhuang, Duan Hao, Wang Weizhou, Tang Zhihong, Wang Yanghao, He Fei. Application of bone tissue engineering materials in the treatment of bone defect diseases in vivo [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 626-631. |
| [12] | Zhang Zhenkun, Li Zhe, Li Ya, Wang Yingying, Wang Yaping, Zhou Xinkui, Ma Shanshan, Guan Fangxia. Application of alginate based hydrogels/dressings in wound healing: sustained, dynamic and sequential release [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 638-643. |
| [13] | Chen Jiana, Qiu Yanling, Nie Minhai, Liu Xuqian. Tissue engineering scaffolds in repairing oral and maxillofacial soft tissue defects [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 644-650. |
| [14] | Xing Hao, Zhang Yonghong, Wang Dong. Advantages and disadvantages of repairing large-segment bone defect [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 426-430. |
| [15] | Yang Caihui, Liu Qicheng, Dong Ming, Wang Lina, Zuo Meina, Lu Ying, Niu Weidong. Serine/threonine protein kinases can promote bone destruction in mouse models of chronic periapical periodontitis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(23): 3654-3659. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||