Chinese Journal of Tissue Engineering Research ›› 2017, Vol. 21 ›› Issue (19): 3072-3079.doi: 10.3969/j.issn.2095-4344.2017.19.019
Previous Articles Next Articles
Unicompartmental knee arthroplasty: the best technique and curative efficacy
Feng Shuo, Zha Guo-chun, Guo Kai-jin, Cai Peng, Chen Xiang-yang
- Department of Orthopedics, Affiliated Hospital of Xuzhou Medical University, Xuzhou 221000, Jiangsu Province, China
-
Online:2017-07-08Published:2017-08-10 -
Contact:Chen Xiang-yang, M.D., Chief physician, Department of Orthopedics, Affiliated Hospital of Xuzhou Medical University, Xuzhou 221000, Jiangsu Province, China -
About author:Feng Shuo, Studying for master’s degree, Department of Orthopedics, Affiliated Hospital of Xuzhou Medical University, Xuzhou 221000, Jiangsu Province, China -
Supported by:the Project of Young Medical Talents of Jiangsu Province, No. QNRC2016800; the Scientific and Technological Project of Xuzhou, No. KC16SL111; the General Project of Health and Family Planning Commission of Jiangsu Province, No. H201528; the Jiangsu Provincial Social Development Project, No. BE2015627; the Scientific and Technological Project of Xuzhou, No.KC14SH091
CLC Number:
Cite this article
Feng Shuo, Zha Guo-chun, Guo Kai-jin, Cai Peng, Chen Xiang-yang. Unicompartmental knee arthroplasty: the best technique and curative efficacy [J]. Chinese Journal of Tissue Engineering Research, 2017, 21(19): 3072-3079.
share this article
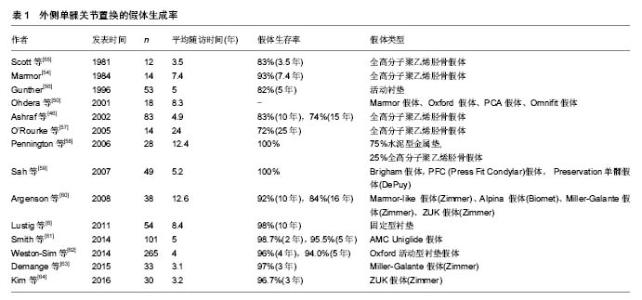
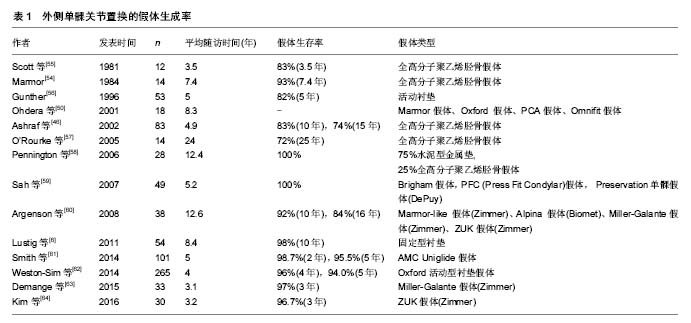
2.1 单髁膝关节置换的发展历史 2.1.1 单髁假体的发展历史 1955年,McKeever[7]开创了单髁关节置换的先河。随后MacIntosh等[8]临床应用了一种由钴铬合金制成的胫骨平台假体,用于置换胫骨关节面,但手术未对股骨表面进行处理,造成这种胫骨的半关节假体术后膝关节功能较差,但这种半关节假体也能在一定程度上缓解患者的疼痛。1968 年,Gunston[9]引入单髁假体的早期的设计理念,建立了一种限制性假体,并于1971年报道其临床效果。 真正意义上的人工单髁膝关节假体则是1973 年Marmor[10]所设计的,Marmor假体与MacIntosh假体的相比,不仅引入了股骨部分的处理还增加了胫骨假体的横径,还在在一定程度上减少了胫骨假体的下沉概率[11]。Marmor假体也成为固定衬垫设计的基石。目前固定假体的代表M/G(Zimmer)假体就是在Marmor假体的基础之上,经历几十年的发展,才在临床上的应用获得成功。 1978年,Goodfellow等[12]在前人的基础上,设计了Oxford活动衬垫承载单髁假体,这是单髁假体发展的里程碑。虽然早期容易出现松动且有着较高脱位率等缺点,但Goodfellow所引入的设计理念是现在临床广为应用的Oxford假体发展的前提,他创造性的将假体分成3个部分:弧形的股骨假体、胫骨假体和聚乙烯衬垫。Oxford活动衬垫单髁假体巨大的改进是弧形的股骨假体与衬垫表面可以进行高度的吻合,这种设计的优点可以明显减少接触应力,也降低聚乙烯的磨损,增加假体寿命。 目前Oxford假体已经发展到第3代,是临床上活动性假活动衬垫假体的杰出代表。单髁关节置换难度较大,有鉴于此,一种可以降低手术难度的多孔表面解剖型假体于20世纪80年代诞生,其将经典的假体的胫骨假体和聚乙烯衬垫有机的进行结合,而股骨假体不变,使假体变成2个部分,明显方便了手术的操作[13]。 2.1.2 手术技术发展历史 自单髁关节置换的理念提出到20世纪80年代可降低手术难度的多孔表面解剖型假体的问世,基本的术式是传统的单髁关节置换,这种手术方法和全膝关节置换的步骤类似,开放的创口较大,出血量很多,加上早期假体设计的缺陷,使得单髁关节置换中长期疗效比全膝关节置换差,优势并未得到体现[14-15]。 20世纪90年代末期,Repicci等[16]采用小切口行单髁关节置换,采用内侧髌骨旁入路,长7-10 cm,这种小切口术式逐渐成熟流行,被称为MIS-UKA。MIS-UKA相较于传统的术式切口小,无需将髌骨进行外翻处理,可以较好的保护伸膝装置,加上第3代Oxford假体进入临床的应用,因此,患者在术后恢复快、恢复锻炼相对容易,单髁手术成功率及术后中长期疗效较前有了长足的进步[17-20]。MIS-UKA手术虽然减少软组织的创伤,但也有一定的缺憾,微小的切口不仅影响医生手术的操作空间而且丧失了良好的视野,无疑会增加手术的难度,加大了学习曲线。 进入21世纪后,由于计算机等数字化技术在外科的发展,计算机导航辅助以及机器人辅助系统MAKO系统逐渐应用MIS-UKA中,方便了单髁关节置换的进行。但目前,由于这种设备价格昂贵,并未在临床上大规模普及,加之术后患者缺乏长时间的随访,其安全性,适用性等问题仍值得进一步探索。 2.2 膝关节单髁关节置换在治疗膝关节骨性关节炎外科治疗中的地位 2.2.1 单髁关节置换与胫骨高位截骨 胫骨高位截骨之所以可以成为治疗骨性关节炎的一种非常有效的方法,一方面其矫正了下肢负重力线,使膝关节的负重分布发生变化,降低患侧胫骨上端的压力,同时也改善局部的血运;另一方面由于髌韧带被松解,故减轻了髌股关节面的压力和胫骨扭转从而减轻膝部疼痛症状[21]。研究发现年龄会影响胫骨高位截骨的效果[21-23],随着年龄的增高,手术失败率也随之增高,因此建议年龄小于60岁,适行胫骨高位截骨。相较于胫骨高位截骨,传统单髁关节置换往往选择年龄大于60岁的患者,单髁关节置换对于老年患者则有更高的性价比[24-25]。胫骨高位截骨和单髁关节置换也有共同的适应证:都要求患者不超重,且膝关节活动度≥90°,内翻畸形≤10°或外翻畸形≤15°,膝关节稳定。但单髁关节置换对于屈曲挛缩在中要求更高,要求行单髁关节置换的患者屈曲挛缩应小于5°。关于胫骨高位截骨和单髁关节置换的疗效,Yim等[25]随访3年的短期结果来看结果无显著差异。 在患者选择适当的情况下,2种术式在中长期随访结果来看所取得的的结果都能获得满意的结果。尽虽如此,目前临床医生更加偏爱单髁关节置换,究其原因,很多医生认为胫骨高位截骨后仅仅可以减轻疼痛,可产生很多并发症,如因胫骨截骨不足或距离关节面太近,发生关节内骨折和胫骨外侧皮质骨折的可能,还有矫正角度丢失、固定失败、膝关节不稳定等的并发症[26-27];而患者行单髁关节置换则可以从根本上解决单间室骨性关节炎疼痛和功能活动受限等问题,且单髁关节置换后可快速康复,早期下地负重,恢复周期较短等的优点也受到了患者的青睐[28-29]。 2.2.2 单髁关节置换与全膝关节置换 自临床应用单髁关节置换治疗单间室骨性关节炎以来,单髁关节置换与全膝关节置换之间的比较和争议一直未曾停止[30-32],20世纪80年代前期由于单髁关节置换本身假体的设计问题或患者选择不当,且手术采用了很多全膝关节置换原则,以至于早期报道单髁关节置换远期随访效果不如全膝关节置换。因此,在这一期间,单髁关节置换遭到了很多医生的摒弃。临床上认为由于骨性关节炎的发展,单髁关节置换仅仅的解决患侧间室问题,最终会因关节病变终究将累及到正常的间室而失败,需要进行翻修,严重的内侧间室骨性关节炎患者,临床上并非仅仅累及单间室,常累及其他间室。对于此,全膝关节置换是一种更好的选择。 近年来单髁关节置换取得的优良疗效,与全膝关节置换相比有很多优势,如创伤小,恢复快,膝关节活动度好等[20,33]。单髁关节置换截骨较少,保留的骨量利于后期翻修,保存了交叉韧带等组织使得膝关节更加稳定[19]。Dennis等[34]研究表明,正常膝关节的运动中,深屈位时膝胫骨相对于股骨内旋平均为 16.5°,而在行走中平均为5.7°,全膝关节置换患者在深屈膝和行走时内旋角度均有减小。Hanson等[35-36]的研究表明,在运动中单髁关节置换更接近于与正常膝,单髁关节置换患者术后屈曲最大时胫骨内旋角度为 13.2°,而全膝关节置换则为6°。Price等[37]则对比了单髁关节置换和全膝关节置换在髌股关节运动学的差异,表明单髁关节置换对髌股关节运动学影响更小。单髁关节置换患者术后深静脉血栓发生率、输血率等并发症的发生率更低[5]。单髁关节置换假体设计理念的更新以及新型材料科学的发展,单髁关节置换成功率不断提高,Ackroyd等[38]对939例行两种术式的患者进行10年随访,结果表明单髁关节置换优良率为要高于全膝关节置换。1998年Newman等[39]报道了单髁关节置换在5年内的翻修率明显高于全膝关节置换,而2009年Newman等[5]经过15年的随访结果,显示2种手术方式的翻修率相当。但2008年Koskinen等[15]报道,单髁关节置换及全膝关节置换15年后生存率分别为60%和80%,前者的长期生存率明显低于后者。但对于单髁关节置换和全膝关节置换的远期效果仍然需要大样本多中心的研究。 作为治疗骨性关节炎最主要的2种治疗手段,选择哪种术式,不仅要严格的掌控手术适应证,还必须要考虑患者的自身情况如年龄,膝关节退变的程度,日常活动量,对于大手术的耐受程度以及及患者的期望值。 2.3 膝关节单髁关节置换的手术指征 2.3.1 内侧单髁关节置换的手术指征的传统观点 内侧单髁关节置换的手术指证最早由Kozinn和Scott[40]所提出:需被诊断为膝关节单间室骨关节炎或骨坏死,且主要表现为活动后疼痛,体质量小于82 kg,日常活动量低,膝关节活动度至少90°,屈曲挛缩畸形小于5°;膝关节内外翻畸形小于15°且术前可以被动纠正,年龄大于60岁的患者可行单髁关节置换。而过度肥胖,严重关节畸形,重体力劳动,被诊断为膝关节感染,炎性关节病(如类风湿性关节炎),或患有严重的骨质疏松症,膝关节多间室的骨关节炎,发生骨性融合的患者被列为禁忌。 2.3.2 内侧单髁关节置换的手术指征的现代观点 目前,对于行单髁关节置换患者争议很大的是年龄和体质量。一些临床研究适当扩大了患者年龄和体质量范围,所获临床效果也是令人满意的[41-42]。 单髁关节置换年龄小于60岁的患者中有保留骨量多易于后期翻修,而且术后活动好,使膝关节更加贴近正常膝的优势。Pennington等[42]对一组行单髁关节置换的35-60岁患者进行11年的随访,其术后有效率达到92%。对于高龄患者而言,相比全膝关节置换,单髁关节置换对患者创伤小,耐受性更好。 经典的单髁关节置换适应症患者体质量应小于82 kg,前期由于固定平台型假体的应用的原因,体质量的增加会使假体加快磨损和松动[43-44]。由于Oxford活动性衬垫假体临床应用的扩大,Murray等[41]对体质量不同的Oxford活动性衬垫假体患者进行随访,结果显示不同体质量患者的生存率接近,肥胖患者行单髁关节置换也取得满意的临床疗效。 2.3.3 外侧单髁关节置换的传统适应证 术前诊断为外侧胫股间室骨性关节炎,骨坏死,创伤性关节炎,外侧部分或全部半月板切除后且下肢外翻角<20°,无症状的髌股关节骨性关节炎,膝关节活动可完全伸直,屈曲90°以上,体质量小于85 kg,年龄60-70岁,前交叉韧带完好的患者可行外侧单髁关节置换。有症状的内侧及髌股关节骨性关节炎伴有关节间隙狭窄,且膝关节内外翻畸形小于15°且术前不能被动纠正的患者为外侧单髁关节置换的绝对禁忌[45]。 2.3.4 外侧单髁关节置换适应证的现代观点 通常认为适合于行外侧单髁关节置换患者年龄为60-70岁。但Van等[45]建议年龄>70岁也可行外侧单髁关节置换,并认为老年患者对于单髁关节置换有良好的耐受性,术中减少失血少,保存更多骨组织,并发症较少,缩短住院时间,且术后可以快速康复,单髁关节置换的疗效也完全满足老年患者的需要;此外,Van等[45]认为年龄>70岁的患者,前交叉韧带若不完整,也可行外侧的单髁关节置换,尽管前交叉韧带不足会破坏单髁关节置换的临床结果,年龄在70岁以上患者,他们的膝关节功能要求较低,且活动量会逐步减少,因此也可行单髁关节置换,但要求术前患者膝关节在伸直不受限,屈曲90°以上。对于风湿病能否行外侧的单髁关节置换还有很大争议[46]。 2.4 外侧单髁关节置换与内侧单髁关节置换的差异 外侧膝关节骨性关节炎并非如内侧骨性关节炎常见,外侧单髁关节置换仅为内侧单髁关节置换的5%-10%,在所有膝关节置换中占比仅为1%[47]。大多数研究关注内侧单髁关节置换,而外侧单髁关节置换由于较低的发病率本身受到较少的关注。 2.4.1 内外侧间室在解剖和生物力学之间差异 胫骨随着屈曲的增加而内旋,而股骨外侧髁相对向后方运动,这时所对应于外侧股骨髁的后向平移。由于胫骨内旋以内侧为轴,因而胫骨内侧骨性关节要比外侧更易形成。膝关节特殊的运动学与生理学不同解释了软骨的磨损程度差异模,同时也可以解释全膝关节置换患者聚乙烯的磨损方式。研究表明,内侧骨性关节炎胫骨磨损主要在前方区域,股骨则为下方关节面;在外侧骨性关节炎中,胫骨磨损在中央及后部区域更为明显,而股骨主要累及后方关节面[48-49]。Ohdera等[50]研究表明,在内翻膝中,患者在正常步行和静态(单腿站立)下肢力线通过内侧间室;外翻膝中,静止状态机械轴通过外侧间室,但在动态时则转向内侧间室,这种机械轴的转换有利于外侧单髁关节置换假体的寿命的延长。 2.4.2 内外侧单髁关节置换的技术之间差异 外侧单髁关节置换在技术上要求比内侧单髁关节置换更苛刻。外侧单髁关节置换的操作可以通过标准的髌旁内侧入路进行,髌旁内侧入路的优点是术中转换为全膝关节置换更容易。最近,一种通过劈开股骨外肌的微创切口受到大家的提倡,但在安放假体时,由于患者往往存在外翻畸形,且髌骨的运动轨迹经常趋于外侧,应避免股骨侧假体与髌骨发生撞击。在外翻膝中,通常存在股骨发育不良,对于此可以采用有较厚的胫骨平台或较厚的股骨假体部件。有研究显示,当胫骨后倾斜角度超过7°时,单髁关节置换的失败率增加,因此建议外侧单髁关节置换最佳胫骨后倾角度是3°-5°,而内侧单髁关节置换一般为7°左右[51]。 2.5 外侧单髁关节置换的应用进展 20世纪70年代,Skolnick等[52]首次对外侧单髁关节置换进行报道,14膝(13例)经过1年随访,结果显示没有重大并发症。Marmor[53]在1976年报道了外侧单髁关节置换效果不佳的临床病例,随后汲取之前外翻畸形过度致手术失败的基础上,Marmor[54]又在1984年报道了一组14例外侧间室单髁关节置换的病例,其中11例患者获得了较好的临床疗效。 自此外侧单髁关节置换逐步在临床上被应用,进入21世纪后,对于适应证的把握和手术技术的发展,假体生存率得到了长足的发展。最近Lustig等[6]的一项长达10年的随访,术中使用的是固定型衬垫,假体的10年存活率为98%,效果满意。结合膝关节外侧髁的运动学,选择固定型衬垫更贴近正常的膝生理。 尽管如此,外侧单髁关节置换具有较大的技术难度更长的学习曲线。目前对于外侧单髁关节置换的疗效仍缺少大样本、多中心、长时间的临床研究。在外侧骨性关节炎的术式选择上,选择单髁关节置换或全膝关节置换很大程度上取决于外科医生的对于每种手术理解和熟练程度。表1为外侧单髁关节置换的假体生存率。"

2.6 计算机及机器人辅助导航技术的应用 精准和微创是医学发展的主要趋势,单髁关节置换中假体安放位置不准确,导致过度矫正或者矫正不足,聚乙烯磨损的增快,导致手术失败[65]。骨科医生更加关注到单髁关节置换后的力线,良好的力线可以增加假体的寿命,提高患者满意度。 一种计算机辅助外科导航已经问世,单髁关节置换目前采用微小切口,由于暴露有限,导航系统有助于实现精确假体定位,提高术后的力线的准确性[66-68]。在对于力线要求苛刻的外侧单髁关节置换导航技术中尤为重要。Jenny等[69]报道前瞻性地研究了60例微创导航单髁关节置换患者,并将他们与早期60例接受开放导航单髁关节置的患者进行比较,结果显示微创导航没有降低假体植入精度,也无严重的并发症。2006年,MAKO外科公司研发的一种触觉机器人臂,并获得美国食品和药物管理局的批准,这种新型的机器人辅助系统是精准外科的最新进展。MAKO骨科关节机器人是目前世界上最先进的骨关节微创手术设备之一,可以明显减少了术中出血和软组织损伤,实现真正的微创,有利于患者术后快速康复锻炼[70-71]。患者在行MAKO骨科关节机器人单髁手术前需行MRI或CT扫描,以重建膝关节三维模型,还需对患者进行个性化的术前设计,而后编程到RIO系统,系统将自动创建截骨的安全区。MAKO骨科关节机器人打破了传统的截骨模式,术中医生需要操作机械臂带动着磨钻对患者的膝关节胫骨和股骨进行精准磨锉。手术的切口更小,约5 cm,机械臂自带摄像机,打磨过程不仅可以可以通过实时的3D画面,清晰了解打磨的深度和范围,而且当截骨超出计划区域外时提供声音和触觉反馈,可以实时精确调整假体植入位置和角度从而获得更好的膝关节力线和软组织平衡。 Coon等[72]将36例接受机器人手臂辅助单髁置换术的患者与45例接受MIS-UKA的患者临床结果进行比较,结果显示,在术后平均的KSS评分、手术前后的KSS评分平均变化以及Marmor评分方面没有明显差异,两种术式取得相似的临床结果,也表明机器人手臂辅助外科这项新技术对于临床医生而言也是相对容易接受的。Roche等[73]报告了一组73例患者接受机器人手臂辅助行UKA临床结果,其中男42例,女31例,平均年龄(71±10)岁,体质量指数平均为29 kg/m2,其中有38%患者诊断为肥胖,患者术前屈曲活动度为123°,术后2年则增加到129°,且术后KSS评分也从术前的43.8分增加到96.8分,术后膝关节功能评分从术前63.9分增加到80分。Mofidi等[74]的研究中发现,对于内侧单髁关节置换的机器人辅助手术导致平均误差为(2.2±1.7)°至(3.6±3.3)°,并认为这些误差取决于一方面术前计划中对放射X射线的等测量差异,另一方面为安放固定假体技术不当有关。Bell等[75]随访了120例患者,其中62例接受MAKO RIO的机器人辅助单髁置换手术,58例接受传统单髁置换,结果发现使用MAKO RIO的机器人辅助外科手术的患者假体植入物组间的定位精度较传统单髁置换手术患者得到了明显提高。 2016年MAKO骨科关节机器人被引入中国,但由于实施病例较少,且缺乏中长期的随访。在提高假体生存率及临床效果方面,仍有待进一步研究。"

| [1] Vielgut I, Leitner L, Kastner N, et al. Sports Activity after Low-contact-stress Total Knee Arthroplasty - A long term follow-up study. Sci Rep. 2016;6:24630. [2] Thienpont E. Conversion of a unicompartmental knee arthroplasty to a total knee arthroplasty: can we achieve a primary result? Bone Joint J. 2017;99-B(1 Supple A):65-69.[3] Horikawa A, Miyakoshi N, Shimada Y, et al. Comparison of clinical outcomes between total knee arthroplasty and unicompartmental knee arthroplasty for osteoarthritis of the knee: a retrospective analysis of preoperative and postoperative results. J Orthop Surg Res. 2015;10:168. [4] Arirachakaran A, Choowit P, Putananon C, et al. Is unicompartmental knee arthroplasty (UKA) superior to total knee arthroplasty (TKA)? A systematic review and meta-analysis of randomized controlled trial. Eur J Orthop Surg Traumatol. 2015;25(5):799-806. [5] Newman J, Pydisetty RV, Ackroyd C. Unicompartmental or total knee replacement: the 15-year results of a prospective randomised controlled trial. J Bone Joint Surg Br. 2009;91(1): 52-57.[6] Lustig S, Elguindy A, Servien E, et al. 5- to 16-year follow-up of 54 consecutive lateral unicondylar knee arthroplasties with a fixed-all polyethylene bearing. J Arthroplasty. 2011;26(8): 1318-1325. [7] McKeever DC. The choice of prosthetic materials and evaluation of results. Clin Orthop. 1955;6:17-21.[8] MacIntosh DL, Hunter GA. The use of the hemiarthroplasty prosthesis for advanced osteoarthritis and rheumatoid arthritis of the knee. J Bone Joint Surg Br. 1972;54(2):244-255.[9] Gunston FH. Polycentric knee arthroplasty. Prosthetic simulation of normal knee movement. J Bone Joint Surg Br. 1971;53(2):272-277.[10] Marmor L. The modular knee. Clin Orthop Relat Res. 1973; (94):242-248.[11] Marmor L. Marmor modular knee in unicompartmental disease. Minimum four-year follow-up. J Bone Joint Surg Am. 1979;61(3):347-353.[12] Goodfellow J, O'Connor J. The mechanics of the knee and prosthesis design. J Bone Joint Surg Br. 1978;60-B(3):358-369.[13] Feng EL, Stulberg SD, Wixson RL. Progressive subluxation and polyethylene wear in total knee replacements with flat articular surfaces.Clin Orthop Relat Res.1994;(299):60-71.[14] Kim YH, Oh JH, Oh SH. Osteolysis around cementless porous-coated anatomic knee prostheses. J Bone Joint Surg Br. 1995;77(2):236-241.[15] Koskinen E, Eskelinen A, Paavolainen P, et al. Comparison of survival and cost-effectiveness between unicondylar arthroplasty and total knee arthroplasty in patients with primary osteoarthritis: a follow-up study of 50,493 knee replacements from the Finnish Arthroplasty Register. Acta Orthop. 2008;79(4):499-507. [16] Repicci JA, Eberle RW. Minimally invasive surgical technique for unicondylar knee arthroplasty. J South Orthop Assoc. 1999;8(1):20-27; discussion 27.[17] Pandit H, Jenkins C, Barker K, et al. The Oxford medial unicompartmental knee replacement using a minimally-invasive approach. J Bone Joint Surg Br. 2006; 88(1):54-60.[18] Pandit HG, Campi S, Hamilton TW, et al. Five-year experience of cementless Oxford unicompartmental knee replacement. Knee Surg Sports Traumatol Arthrosc. 2017; 25(3):694-702. [19] Pandit H, Jenkins C, Gill HS, et al. Minimally invasive Oxford phase 3 unicompartmental knee replacement: results of 1000 cases. J Bone Joint Surg Br. 2011;93(2):198-204.[20] Faour-Martín O, Valverde-García JA, Martín-Ferrero MA, et al. Oxford phase 3 unicondylar knee arthroplasty through a minimally invasive approach: long-term results. Int Orthop. 2013;37(5):833-838.[21] Akizuki S, Shibakawa A, Takizawa T, et al. The long-term outcome of high tibial osteotomy: a ten- to 20-year follow-up. J Bone Joint Surg Br. 2008;90(5):592-596. [22] van Raaij T, Reijman M, Brouwer RW, et al. Survival of closing-wedge high tibial osteotomy: good outcome in men with low-grade osteoarthritis after 10-16 years. Acta Orthop. 2008;79(2):230-234. [23] Billings A, Scott DF, Camargo MP, et al. High tibial osteotomy with a calibrated osteotomy guide, rigid internal fixation, and early motion. Long-term follow-up. J Bone Joint Surg Am. 2000;82(1):70-79.[24] Nwachukwu BU, McCormick FM, Schairer WW, et al. Unicompartmental knee arthroplasty versus high tibial osteotomy: United States practice patterns for the surgical treatment of unicompartmental arthritis. J Arthroplasty. 2014;29(8):1586-1589. [25] Yim JH, Song EK, Seo HY, et al. Comparison of high tibial osteotomy and unicompartmental knee arthroplasty at a minimum follow-up of 3 years. J Arthroplasty. 2013;28(2): 243-247. [26] Atrey A, Morison Z, Tosounidis T, et al. Complications of closing wedge high tibial osteotomies for unicompartmental osteoarthritis of the knee. Bone Joint Res. 2012;1(9):205-209. [27] Mont MA, Stuchin SA, Paley D, et al. Different surgical options for monocompartmental osteoarthritis of the knee: high tibial osteotomy versus unicompartmental knee arthroplasty versus total knee arthroplasty: indications, techniques, results, and controversies. Instr Course Lect. 2004;53:265-283.[28] Rodriguez-Merchan EC. Unicompartmental Knee Osteoarthritis (UKOA): Unicompartmental Knee Arthroplasty (UKA) or High Tibial Osteotomy (HTO)? Arch Bone Jt Surg. 2016;4(4):307-313.[29] Dettoni F, Bonasia DE, Castoldi F, et al. High tibial osteotomy versus unicompartmental knee arthroplasty for medial compartment arthrosis of the knee: a review of the literature. Iowa Orthop J. 2010;30:131-140.[30] Longo UG, Loppini M, Trovato U, et al. No difference between unicompartmental versus total knee arthroplasty for the management of medial osteoarthtritis of the knee in the same patient: a systematic review and pooling data analysis. Br Med Bull. 2015;114(1):65-73. [31] van der List JP, Chawla H, Zuiderbaan HA, et al. Patients with isolated lateral osteoarthritis: Unicompartmental or total knee arthroplasty? Knee. 2016;23(6):968-974.[32] van der List JP, Chawla H1, Villa JC1, et al. The Role of Patient Characteristics on the Choice of Unicompartmental versus Total Knee Arthroplasty in Patients With Medial Osteoarthritis. J Arthroplasty. 2017;32(3):761-766. [33] Kulshrestha V, Datta B, Kumar S, et al. Outcome of Unicondylar Knee Arthroplasty vs Total Knee Arthroplasty for Early Medial Compartment Arthritis: A Randomized Study. J Arthroplasty. 2017;32(5):1460-1469. [34] Dennis DA, Komistek RD, Mahfouz MR, et al. A multicenter analysis of axial femorotibial rotation after total knee arthroplasty. Clin Orthop Relat Res. 2004;(428):180-189.[35] Hanson GR, Moynihan AL, Suggs JF, et al. Kinematics of medial unicondylar knee arthroplasty: an in vivo investigation. J Knee Surg. 2009;22(3):237-242.[36] Hanson GR, Suggs JF, Freiberg AA, et al. Investigation of in vivo 6DOF total knee arthoplasty kinematics using a dual orthogonal fluoroscopic system. J Orthop Res. 2006;24(5): 974-981.[37] Price AJ, Oppold PT, Murray DW, et al. Simultaneous in vitro measurement of patellofemoral kinematics and forces following Oxford medial unicompartmental knee replacement. J Bone Joint Surg Br. 2006;88(12):1591-1595.[38] Ackroyd CE, Whitehouse SL, Newman JH, et al. A comparative study of the medial St Georg sled and kinematic total knee arthroplasties. Ten-year survivorship. J Bone Joint Surg Br. 2002;84(5):667-672.[39] Newman JH, Ackroyd CE, Shah NA. Unicompartmental or total knee replacement? Five-year results of a prospective, randomised trial of 102 osteoarthritic knees with unicompartmental arthritis. J Bone Joint Surg Br. 1998;80(5): 862-865.[40] Kozinn SC, Scott R. Unicondylar knee arthroplasty. J Bone Joint Surg Am. 1989;71(1):145-150.[41] Murray DW, Pandit H, Weston-Simons JS, et al. Does body mass index affect the outcome of unicompartmental knee replacement? Knee. 2013;20(6):461-465.[42] Pennington DW, Swienckowski JJ, Lutes WB, et al. Unicompartmental knee arthroplasty in patients sixty years of age or younger. J Bone Joint Surg Am. 2003;85-A(10): 1968-1973.[43] Plate JF, Augart MA, Seyler TM, et al. Obesity has no effect on outcomes following unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2017; 25(3):645-651.[44] Kandil A, Werner BC, Gwathmey WF, et al. Obesity, morbid obesity and their related medical comorbidities are associated with increased complications and revision rates after unicompartmental knee arthroplasty. J Arthroplasty. 2015; 30(3):456-460. [45] Volpi P, Marinoni L, Bait C, et al. Lateral unicompartimental knee arthroplasty: indications, technique and short-medium term results. Knee Surg Sports Traumatol Arthrosc. 2007;15 (8):1028-1034. [46] Ashraf T, Newman JH, Evans RL, et al. Lateral unicompartmental knee replacement survivorship and clinical experience over 21 years. J Bone Joint Surg Br. 2002;84(8): 1126-1130.[47] Ollivier M, Abdel MP, Parratte S, et al. Lateral unicondylar knee arthroplasty (UKA): contemporary indications, surgical technique, and results. Int Orthop. 2014;38(2): 449-455. [48] Zhang Q, Guo W, Liu Z, et al. Risk factors for lateral compartmental cartilage wear in varus knee osteoarthritis. Zhonghua Wai Ke Za Zhi. 2015;53(5):357-361.[49] Weidow J, Pak J, Kärrholm J. Different patterns of cartilage wear in medial and lateral gonarthrosis. Acta Orthop Scand. 2002;73(3):326-329.[50] Ohdera T, Tokunaga J, Kobayashi A. Unicompartmental knee arthroplasty for lateral gonarthrosis: midterm results. J Arthroplasty. 2001;16(2):196-200.[51] Scott RD. Lateral unicompartmental replacement: a road less traveled. Orthopedics. 2005;28(9):983-984.[52] Skolnick MD, Bryan RS, Peterson LF. Unicompartmental polycentric knee arthroplasty: description and preliminary results. Clin Orthop Relat Res. 1975;(112):208-214.[53] Marmor L. The Modular (Marmor) knee: case report with a minimum follow-up of 2 years. Clin Orthop Relat Res. 1976; (120):86-94.[54] Marmor L. Lateral compartment arthroplasty of the knee. Clin Orthop Relat Res. 1984;(186):115-121.[55] Scott RD, Santore RF. Unicondylar unicompartmental replacement for osteoarthritis of the knee. J Bone Joint Surg Am. 1981;63(4):536-544.[56] Gunther TV, Murray DW, Miller R, et al. Lateral unicompartmental arthroplasty with the Oxford meniscal knee. Knee. 1996;51(3):33-39.[57] O'Rourke MR, Gardner JJ, Callaghan JJ, et al. The John Insall Award: unicompartmental knee replacement: a minimum twenty-one-year followup, end-result study. Clin Orthop Relat Res. 2005;440:27-37.[58] Pennington DW, Swienckowski JJ, Lutes WB, et al. Lateral unicompartmental knee arthroplasty: survivorship and technical considerations at an average follow-up of 12.4 years. J Arthroplasty. 2006;21(1):13-17.[59] Sah AP, Scott RD. Lateral unicompartmental knee arthroplasty through a medial approach. Study with an average five-year follow-up. J Bone Joint Surg Am. 2007; 89(9):1948-1954.[60] Argenson JN, Parratte S, Bertani A, et al. Long-term results with a lateral unicondylar replacement. Clin Orthop Relat Res. 2008;466(11):2686-2693. [61] Smith JR, Robinson JR, Porteous AJ, et al. Fixed bearing lateral unicompartmental knee arthroplasty--short to midterm survivorship and knee scores for 101 prostheses. Knee. 2014; 21(4):843-847.[62] Weston-Simons JS, Pandit H, Kendrick BJ, et al. The mid-term outcomes of the Oxford Domed Lateral unicompartmental knee replacement. Bone Joint J. 2014;96-B (1):59-64.[63] Demange MK, Von Keudell A, Probst C, et al. Patient-specific implants for lateral unicompartmental knee arthroplasty. Int Orthop. 2015;39(8):1519-1526. [64] Kim KT, Lee S, Kim J, et al. Clinical Results of Lateral Unicompartmental Knee Arthroplasty: Minimum 2-Year Follow-up. Clin Orthop Surg. 2016;8(4):386-392. [65] Hamilton WG, Collier MB, Tarabee E, et al. Incidence and reasons for reoperation after minimally invasive unicompartmental knee arthroplasty. J Arthroplasty. 2006; 21(6 Suppl 2):98-107.[66] Grant AL, Doma KD, Hazratwala K. Determination of the Accuracy of Navigated Kinematic Unicompartmental Knee Arthroplasty: A 2-Year Follow-Up. J Arthroplasty. 2017; 32(5):1443-1452. [67] Valenzuela GA, Jacobson NA, Geist DJ, et al. Implant and limb alignment outcomes for conventional and navigated unicompartmental knee arthroplasty. J Arthroplasty. 2013; 28(3):463-468. [68] van der List JP, Chawla H, Joskowicz L, et al. Current state of computer navigation and robotics in unicompartmental and total knee arthroplasty: a systematic review with meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2016; 24(11):3482-3495. [69] Jenny JY, Ciobanu E, Boeri C. The rationale for navigated minimally invasive unicompartmental knee replacement. Clin Orthop Relat Res. 2007;463:58-62.[70] Pearle AD, Kendoff D, Stueber V, et al. Perioperative management of unicompartmental knee arthroplasty using the MAKO robotic arm system (MAKOplasty). Am J Orthop (Belle Mead NJ). 2009;38(2 Suppl):16-19.[71] Jaffry Z, Masjedi M, Clarke S, et al. Unicompartmental knee arthroplasties: robot vs. patient specific instrumentation. Knee. 2014;21(2):428-434.[72] Coon T, Driscoll M, Conditt MA. Early Clinical Success of Novel Tactile Guided UKA Technique. 21st Congress of the ISTA. Sacremento, CA, 2008.[73] Roche MW, Horowitz S, Conditt MA. Four year outcomes of robotically guided UKA. 23rd Annual Congress of ISTA. Dubai, UAE, 2010.[74] Mofidi A, Plate JF, Lu B, et al. Assessment of accuracy of robotically assisted unicompartmental arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2014;22(8):1918-1925.[75] Bell SW, Anthony I, Jones B, et al. Improved Accuracy of Component Positioning with Robotic-Assisted Unicompartmental Knee Arthroplasty: Data from a Prospective, Randomized Controlled Study. J Bone Joint Surg Am. 2016;98(8):627-635. |
| [1] | Wang Jianping, Zhang Xiaohui, Yu Jinwei, Wei Shaoliang, Zhang Xinmin, Xu Xingxin, Qu Haijun. Application of knee joint motion analysis in machanism based on three-dimensional image registration and coordinate transformation [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(在线): 1-5. |
| [2] | Zhang Jichao, Dong Yuefu, Mou Zhifang, Zhang Zhen, Li Bingyan, Xu Xiangjun, Li Jiayi, Ren Meng, Dong Wanpeng. Finite element analysis of biomechanical changes in the osteoarthritis knee joint in different gait flexion angles [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1357-1361. |
| [3] | Yao Xiaoling, Peng Jiancheng, Xu Yuerong, Yang Zhidong, Zhang Shuncong. Variable-angle zero-notch anterior interbody fusion system in the treatment of cervical spondylotic myelopathy: 30-month follow-up [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1377-1382. |
| [4] | Zhuang Zhikun, Wu Rongkai, Lin Hanghui, Gong Zhibing, Zhang Qianjin, Wei Qiushi, Zhang Qingwen, Wu Zhaoke. Application of stable and enhanced lined hip joint system in total hip arthroplasty in elderly patients with femoral neck fractures complicated with hemiplegia [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1429-1433. |
| [5] | Jin Tao, Liu Lin, Zhu Xiaoyan, Shi Yucong, Niu Jianxiong, Zhang Tongtong, Wu Shujin, Yang Qingshan. Osteoarthritis and mitochondrial abnormalities [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1452-1458. |
| [6] | Zhang Lichuang, Xu Hao, Ma Yinghui, Xiong Mengting, Han Haihui, Bao Jiamin, Zhai Weitao, Liang Qianqian. Mechanism and prospects of regulating lymphatic reflux function in the treatment of rheumatoid arthritis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1459-1466. |
| [7] | Wang Baojuan, Zheng Shuguang, Zhang Qi, Li Tianyang. Miao medicine fumigation can delay extracellular matrix destruction in a rabbit model of knee osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1180-1186. |
| [8] | Wu Bingshuang, Wang Zhi, Tang Yi, Tang Xiaoyu, Li Qi. Anterior cruciate ligament reconstruction: from enthesis to tendon-to-bone healing [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1293-1298. |
| [9] | An Weizheng, He Xiao, Ren Shuai, Liu Jianyu. Potential of muscle-derived stem cells in peripheral nerve regeneration [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1130-1136. |
| [10] | Zhang Jinglin, Leng Min, Zhu Boheng, Wang Hong. Mechanism and application of stem cell-derived exosomes in promoting diabetic wound healing [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1113-1118. |
| [11] | Yang Kuangyang, Wang Changbing. MRI evaluation of graft maturity and knee function after anterior cruciate ligament reconstruction with autogenous bone-patellar tendon-bone and quadriceps tendon [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 963-968. |
| [12] | Liu Dongcheng, Zhao Jijun, Zhou Zihong, Wu Zhaofeng, Yu Yinghao, Chen Yuhao, Feng Dehong. Comparison of different reference methods for force line correction in open wedge high tibial osteotomy [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 827-831. |
| [13] | Shao Yangyang, Zhang Junxia, Jiang Meijiao, Liu Zelong, Gao Kun, Yu Shuhan. Kinematics characteristics of lower limb joints of young men running wearing knee pads [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 832-837. |
| [14] | Huang Hao, Hong Song, Wa Qingde. Finite element analysis of the effect of femoral component rotation on patellofemoral joint contact pressure in total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 848-852. |
| [15] | Yuan Jing, Sun Xiaohu, Chen Hui, Qiao Yongjie, Wang Lixin. Digital measurement and analysis of the distal femur in adults with secondary knee valgus deformity [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 881-885. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||