| [1]Harms J,Melcher RP.Posterior C1-C2 fusion with polyaxial screw and rod fixation. Spine. 2001;26(22): 2467-2471.
[2]马向阳,钟世镇,刘景发,等.寰枢椎后路椎弓根螺钉固定的生物力学评价[J].中国脊柱脊髓杂志, 2003,13(12): 735-738.
[3]Richter M,Schmidt R,Claes L,et al.Posterior atlantoaxial fixation: biomechanical in vitro comparison of six different techniques.Spine. 2002;27(16): 1724-1732.
[4]潘军伟,黄大耿,郝定均.寰枢椎失稳症的外科治疗研究进展[J].中国骨与关节损伤杂志,2014,29(3):308-309.
[5]Larcock PA,Cooper JJ.Adverse reactions of artificial bone graft substitutes: lessons learned from using tricalcium phosphate geneX.Clin Orthop Relat Res. 2014;472(2):765-766.
[6]Ma XY,Yin QS,Wu ZH,et al.Anatomic considerations for the pedicle screw placement in the first cervical vertebra.Spine.2005;30(13):1519-1523.
[7]Yang SY,Boniello AJ,Poorman CE,et al.A review of the diagnosis and treatment of atlantoaxial dislocations.Global Spine J.2014;4(3):197-210.
[8]Behari S,Bhargava V,Nayak S,et al.Congenital reducible atlantoaxial dislocation: classification and surgical considerations.Acta Neurochir. 2002;144(11): 1165-1177.
[9]窦以宝,罗学勤,尹玉荣,等.寰枢椎椎弓根螺钉内固定治疗Ⅱ型齿突骨折合并寰枢椎脱位[J].脊柱外科杂志, 2014, 6(3):165-168.
[10]Yang JC,Ma XY,Xia H,et al.Clinical application of computer-aided design-rapid prototyping in C1-C2 operation techniques for complex atlantoaxial instability.J Spinal Disord Tech.2014;27(4):E143-E150.
[11]王建华,尹庆水,夏虹,等.数字骨科技术在寰枢椎个体化置钉手术中的应用[J].脊柱外科杂志,2011,9(3):165-168.
[12]Jun SH,Lee EJ,Jang TS,et al.Bone morphogenic protein-2(BMP-2) loaded hybrid coating on porous hydroxyapatite scaffolds for bone tissue engineering.J Mater Sci Mater Med.2013;24(3):773-782.
[13]贾桂平,张建华,贾贵军.复杂颅颈交界区畸形合并寰枢椎脱位后路减压复位内固定术的护理配合[J].护理研究, 2014,7(12):4429-4430.
[14]邓淼,权正学,罗小辑.寰枢椎椎弓根螺钉治疗寰枢椎不稳及脱位的临床效果[J].创伤外科杂志,2016,4(1):28-31.
[15]艾福志.寰枢椎脱位前路手术治疗-TARP内固定手术寰枢椎脱位系列讲座[J].中国骨科临床与基础研究杂志, 2015,7(4):243-251.
[16]Brooks AL,Jenkins EB.Atlanto-axial arthrodesis by the wedge compression method.J Bone Joint Surg Am. 1978;60(3):279-284.
[17]Magerl F,Seeman PS.Stable posterior fusion of the atlas and axis by transarticular screw fixation// Kehr P,Weidner A.Cervical Spine.New York:Spinger Verlag, 1985:322-327.
[18]Goel A,Laheri V.Plate and screw fixation for atlanto-axial subluxation.Acta Neurochir. 1994;129(1-2):47-53.
[19]Goel A,Desai KI,Muzumdar DP.Atlantoaxial fixation using palte and screw method: a report of 160 treated patients.Neurosurgery.2002;51(6):1351-1357.
[20]谭明生.寰枢椎脱位外科治疗的现状与思考[J].中华骨科杂志,2015,35(35):463-464.
[21]郭胜利,乔广宇,余新光,等.自发性寰枢椎脱位内固定技术的研究进展[J].中华神经外科杂志,2015,31(7):750-751.
[22]范军界,金正帅,殷国勇,等.寰枢椎椎弓根螺钉系统在寰枢椎骨折脱位中的应用[J].江苏医药, 2015,41(9): 1067-1069.
[23]Benke M,Yu WD,Peden SC,et al.Occipitocervical junction: imaging, pathology, instrumentation.Am J Orthop (Belle Mead NJ).2011;40(10):E205-215.
[24]刘斐文,张彤,孙川江,等.后路寰枢椎椎弓根螺钉短节段内固定治疗齿状突骨折并寰枢椎脱位[J].四川医学, 2014, 35(2):221-223.
[25]丁英胜,张文志,段丽群,等.后路寰枢椎椎弓根固定融合治疗寰枢椎不稳或脱位[J].临床骨科杂志,2015,18(1):1-4.
[26]王明飞,纪斌,王健,等.寰枢椎后路线缆内固定融合术治疗寰枢椎不稳的长期疗效分析[J].中国矫形外科杂志, 2015, 23(11):972-975.
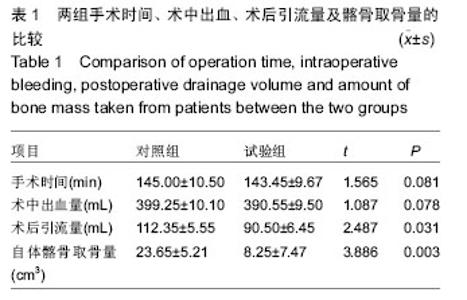
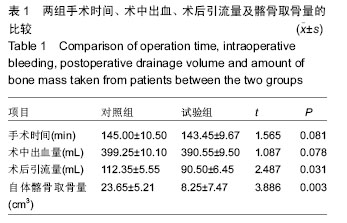
[27]马向阳,杨进城,邱锋,等.寰枢椎脱位后路植骨材料的选择与融合效果评价[J].中国骨科临床与基础研究杂志, 2015, 7(1):5-9.
[28]Chen Z,Ba G,Shen T,et al.Recombinant human bone morphogenetic protein-2 versus autogenous iliac crest bone graft for lumbar fusion: a meta-analysis of ten randomized controlled trials.Arch Orthop Trauma Surg. 2012;132(12):1725-1740.
[29]张志宏,刘志礼,高志增,等.骨修复材料修复骨缺损的选择与应用[J].中国组织工程研究,2012,16(52):9836-9843.
[30]梁必如,严坚强,孙奎,等.颅骨牵引联合短节段枕颈固定颗粒状植骨融合治疗寰枕融合畸形并寰枢椎脱位[J].中国骨与关节损伤杂志,2014,29(5):472-473. |