Chinese Journal of Tissue Engineering Research ›› 2014, Vol. 18 ›› Issue (34): 5441-5448.doi: 10.3969/j.issn.2095-4344.2014.34.006
Previous Articles Next Articles
Acellular dermal matrix allograft combined with coralline hydroxyapatite repair periapical tissue defects
Xu Jun1, Wang Jin-tao2, Li Gang1, Shi Fang-chuan2, Zhong Liang-jun2
- 1 Periodontal & Mucosal Department, Center of Stomatology, the First Affiliated Hospital of Xinjiang Medical University, Urumqi 830054, Xinjiang Uygur Autonomous Region, China; 2 Department of Stomatology, the Affiliated Hospital of Hangzhou Normal University, Hangzhou 310015, Zhejiang Province, China
-
Revised:2014-06-05Online:2014-08-20Published:2014-08-20 -
Contact:Zhong Liang-jun, M.D., Professor, Chief physician, Department of Stomatology, the Affiliated Hospital of Hangzhou Normal University, Hangzhou 310015, Zhejiang Province, China -
About author:Xu Jun, Master, Lecturer, Attending physician, Periodontal & Mucosal Department, Center of Stomatology, the First Affiliated Hospital of Xinjiang Medical University, Urumqi 830054, Xinjiang Uygur Autonomous Region, China -
Supported by:a grant from Xinjiang Uygur Autonomous Region, No. 201091144
CLC Number:
Cite this article
Xu Jun, Wang Jin-tao, Li Gang, Shi Fang-chuan, Zhong Liang-jun. Acellular dermal matrix allograft combined with coralline hydroxyapatite repair periapical tissue defects[J]. Chinese Journal of Tissue Engineering Research, 2014, 18(34): 5441-5448.
share this article

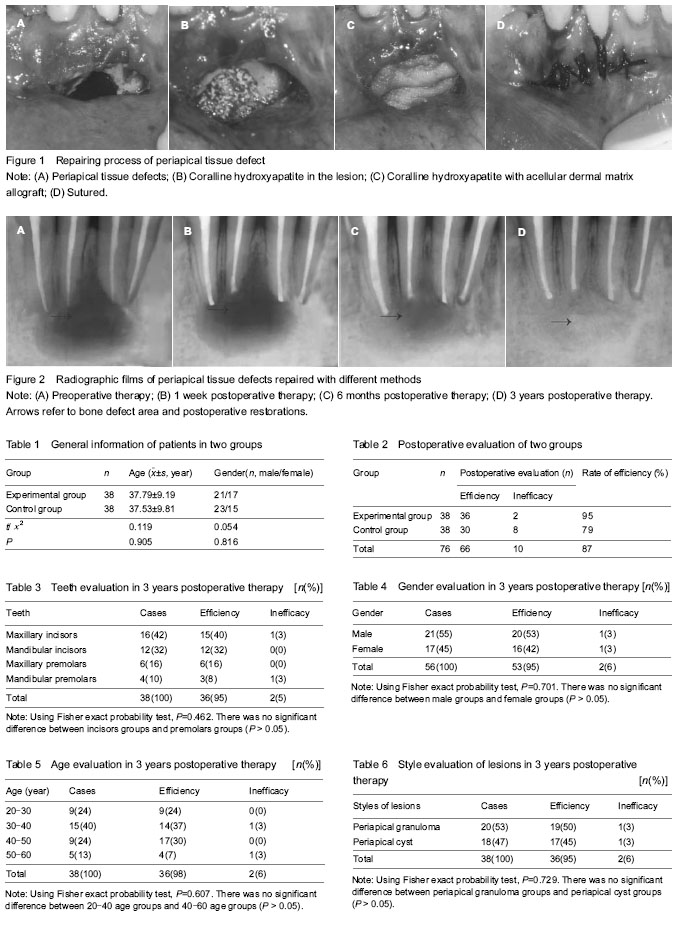
Quantitative analysis of subjects All patients in both groups were included in following analysis. Clinical observation of periapical tissue defects repaired with different methods The complaints of patients, the degree of pain when percussed the crown vertically or laterally and the swelling degree of the mucous membranes was observed. The wounds were all primary healing. One week after operation, no significant discomfort was observed in patients. At 1 month, all acellular dermal matrix allografts survived, moreover, the defect of gingival tissues that caused by repairing fistula had been healed. As shown in Table 1, there was no significant difference between two groups in 3 years postoperative therapy (P > 0.05). As shown in Table 2, the rate of efficiency was 95% in the experimental group, and 79% in the control group, there was a significant difference between two groups in 3 years postoperative therapy (χ2=4.15, P < 0.05). There was no significant difference in the teeth, gender, age and style of lesions in 3 years postoperative therapy in the experimental group (Tables 3-6). Analysis of radiographic films of periapical tissue defects repaired with different methods Due to the large range of bone destruction, we shot periapical films to observe the tiny changes in periodontal tissue and compare the curative effect. As shown in radiographic films, we can see that there was a large scope of bone defect area before operation. The scope in Figure 2A was about 1.8 cm × 1.4 cm. The bone defect disappeared 6 months after operation, the transmission of coralline hydroxyapatite particles decreased, and, there were some fuzzy images of compact density. It suggested that new bone was growing. The density of coralline hydroxyapatite particle was similar to normal bone tissue after 3 years (Figure 2), and there were transitional changes of density between coralline hydroxyapatite with normal bone, which suggested that it began to combine with the alveolar bone."

Biocompatibility of different methods for repairing periapical tissue defects Acellular dermal matrix allograft is derived from the human or animal skin tissue, and is treated through physical and chemical treatment. The treatment may remove all the components that may cause immune rejection after implantation, and maintain three-dimensional scaffold structure of original tissue. As the cytoskeleton, it can induce tissue formation, and can be recognized as autologous tissue after implanted into the human body, subsequently neovascularization and fibroblast ingrowth occur, which guide the orderly growth of the cells along its collagen framework to supplement, repair and even reconstruct the tissues. Acellular dermal matrix allograft has no toxicity, no antigenicity, and good biocompatibility. After implantation, acellular dermal matrix allograft induces fewer inflammatory reactions than the mucosa transplantation. Due to excellent biocompatibility, acellular dermal matrix allograft has been widely used as a scaffold for the construction of artificial composite materials and the repair of maxillofacial mucosal defect. No immune response of the host is found. The results of this study revealed no abnormalities."

| [1] Tronstad L, Barnett F, Cervone F. Periapical bacterial plaque in teeth refractory to endodontic treatment. Endod Dent Traumatol. 1990;6(2):73-77. [2] Sen BH, Piskin B, Demirci T. Observation of bacteria and fungi in infected root canals and dentinal tubules by SEM. Endod Dent Traumatol. 1995;11(1):6-9. [3] Ng YL, Mann V, Gulabivala K. Tooth survival following non-surgical root canal treatment: a systematic review of the literature. Int Endod J. 2010;43(3):171-189. [4] Tsesis I, Rosen E, Tamse A, et al. Effect of guided tissue regeneration on the outcome of surgical endodontic treatment: a systematic review and meta-analysis. J Endod. 2011;37(8):1039-1045. [5] Goyal B, Tewari S, Duhan J, et al. Comparative evaluation of platelet-rich plasma and guided tissue regeneration membrane in the healing of apicomarginal defects: a clinical study. J Endod. 2011;37(6):773-780. [6] Kovác J, Kovác D. Histopathology and etiopathogenesis of chronic apical periodontitis--periapical granuloma. Epidemiol Mikrobiol Imunol. 2011;60(2):77-86. [7] Nair PN. Pathogenesis of apical periodontitis and the causes of endodontic failures. Crit Rev Oral Biol Med. 2004; 15(6):348-381. [8] Kawaguchi H, Kurihara H. Clinical trial of periodontal tissue regeneration. Nihon Rinsho. 2008;66(5):948-954. [9] Ng YL, Mann V, Gulabivala K. A prospective study of the factors affecting outcomes of non-surgical root canal treatment: part 2: tooth survival. Int Endod J. 2011;44(7): 610-625. [10] Ma J, Al-Ashaw AJ, Shen Y, et al. Efficacy of ProTaper Universal Rotary Retreatment system for gutta-percha removal from oval root canals: a micro-computed tomography study. J Endod. 2012;38(11):1516-1520. [11] García CC, Sempere FV, Diago MP, et al. The post-endodontic periapical lesion: histologic and etiopathogenic aspects. Med Oral Patol Oral Cir Bucal. 2007;12(8):E585-590. [12] Maddalone M, Gagliani M. Periapical endodontic surgery: a 3-year follow-up study. Int Endod J. 2003;36(3):193-198. [13] von Arx T. Apical surgery: A review of current techniques and outcome. Saudi Dent J. 2011;23(1):9-15. [14] Lindeboom JA. Apical endodontic surgery. Ned Tijdschr Tandheelkd. 2004;111(4):146-151. [15] Pawar AM, Kokate SR, Shah RA. Management of a large periapical lesion using Biodentine(™) as retrograde restoration with eighteen months evident follow up. J Conserv Dent. 2013;16(6):573-575. [16] Bashutski JD, Wang HL. Periodontal and endodontic regeneration. J Endod. 2009;35(3):321-328. [17] Kinaia BM, Chogle SM, Kinaia AM, et al. Regenerative therapy: a periodontal-endodontic perspective. Dent Clin North Am. 2012;56(3): 537-547. [18] Pecora G, De Leonardis D, Ibrahim N, et al. The use of calcium sulphate in the surgical treatment of a 'through and through' periradicular lesion. Int Endod J. 2001;34(3): 189-197. [19] Lin L, Chen MY, Ricucci D, et al. Guided tissue regeneration in periapical surgery. J Endod. 2010;36(4): 618-625. [20] Naylor J, Mines P, Anderson A, et al. The use of guided tissue regeneration techniques among endodontists: a web-based survey. J Endod. 2011;37(11):1495-1498. [21] Tobón SI, Arismendi JA, Marín ML, et al. Comparison between a conventional technique and two bone regeneration techniques in periradicular surgery. Int Endod J. 2002;35(7):635-641. [22] von Arx T, Cochran DL. Rationale for the application of the GTR principle using a barrier membrane in endodontic surgery: a proposal of classification and literature review. Int J Periodontics Restorative Dent. 2001;21(2):127-139. [23] Taschieri S, Corbella S, Tsesis I, et al. Effect of guided tissue regeneration on the outcome of surgical endodontic treatment of through-and-through lesions: a retrospective study at 4-year follow-up. Oral Maxillofac Surg. 2011; 15(3): 153-159. [24] Marín-Botero ML, Domínguez-Mejía JS, Arismendi-Echavarría JA, et al. Healing response of apicomarginal defects to two guided tissue regeneration techniques in periradicular surgery: a double-blind, randomized-clinical trial. Int Endod J. 2006;39(5):368-377. [25] Sánchez-Torres A, Sánchez-Garcés MA, Gay-Escoda C. Materials and prognostic factors of bone regeneration in periapical surgery: A systematic review. Med Oral Patol Oral Cir Bucal. 2014. in press. [26] Baran ET, Tuzlakoglu K, Salgado AJ, et al. Multichannel mould processing of 3D structures from microporous coralline hydroxyapatite granules and chitosan support materials for guided tissue regeneration/engineering. J Mater Sci Mater Med. 2004;15(2):161-165. [27] Swetha M, Sahithi K, Moorthi A, et al. Biocomposites containing natural polymers and hydroxyapatite for bone tissue engineering. Int J Biol Macromol. 2010;47(1):1-4. [28] Zhang L, Tang P, Zhang W, et al. Effect of chitosan as a dispersant on collagen-hydroxyapatite composite matrices. Tissue Eng Part C Methods. 2010;16(1):71-79. [29] Venkatesan J, Kim SK. Chitosan composites for bone tissue engineering--an overview. Mar Drugs. 2010;8(8):2252-2266. [30] Chen L, Hu J, Shen X, et al. Synthesis and characterization of chitosan-multiwalled carbon nanotubes/hydroxyapatite nanocomposites for bone tissue engineering. J Mater Sci Mater Med. 2013;24(8):1843-1851. [31] Pighinelli L, Kucharska M. Chitosan-hydroxyapatite composites. Carbohydr Polym. 2013;93(1):256-262. [32] Zigdon H, Horwitz J. Using acellular dermal matrix (ADM) allograft in periodontal surgery--a literature review and case reports. Refuat Hapeh Vehashinayim. 2006;24(3):19-29, 92. [33] Tal H. Subgingival acellular dermal matrix allograft for the treatment of gingival recession: a case report. J Periodontol. 1999;70(9):1118-1124. [34] de Souza SL, Novaes AB Jr, Grisi DC, et al. Comparative clinical study of a subepithelial connective tissue graft and acellular dermal matrix graft for the treatment of gingival recessions: six- to 12-month changes. J Int Acad Periodontol. 2008;10(3):87-94. [35] Rahmani ME, Lades MA. Comparative clinical evaluation of acellular dermal matrix allograft and connective tissue graft for the treatment of gingival recession. J Contemp Dent Pract. 2006;7(2):63-70. [36] Novaes AB Jr, de Barros RR. Acellular dermal matrix allograft. The results of controlled randomized clinical studies. J Int Acad Periodontol. 2008;10(4):123-129. [37] Moslemi N, Mousavi Jazi M, Haghighati F, et al. Acellular dermal matrix allograft versus subepithelial connective tissue graft in treatment of gingival recessions: a 5-year randomized clinical study. J Clin Periodontol. 2011; 38(12): 1122-1129. [38] Fotek PD, Neiva RF, Wang HL. Comparison of dermal matrix and polytetrafluoroethylene membrane for socket bone augmentation: a clinical and histologic study. J Periodontol. 2009;80(5):776-785. [39] Froum S, Cho SC, Elian N, et al. Extraction sockets and implantation of hydroxyapatites with membrane barriers: a histologic study. Implant Dent. 2004;13(2):153-164. [40] Terino EO. Alloderm acellular dermal graft: applications in aesthetic soft-tissue augmentation. Clin Plast Surg. 2001; 28(1):83-99. [41] Barros RR, Novaes AB, Grisi MF, et al. A 6-month comparative clinical study of a conventional and a new surgical approach for root coverage with acellular dermal matrix. J Periodontol. 2004;75(10):1350-1356. [42] Sclafani AP, Romo T 3rd, Jacono AA, et al. Evaluation of acellular dermal graft (AlloDerm) sheet for soft tissue augmentation: a 1-year follow-up of clinical observations and histological findings. Arch Facial Plast Surg. 2001;3(2): 101-103. [43] Orstavik D, Kerekes K, Eriksen HM. The periapical index: a scoring system for radiographic assessment of apical periodontitis. Endod Dent Traumatol. 1986;2(1):20-34. [44] Friedman S, Abitbol S, Lawrence HP. Treatment outcome in endodontics: the Toronto Study. Phase 1: initial treatment. J Endod. 2003;29(12):787-793. [45] Lin L, Chen MY, Ricucci D, et al. Guided tissue regeneration in periapical surgery. J Endod. 2010;36(4): 618-625. [46] Moreira-Gonzalez A, Jackson IT, Miyawaki T, et al. Augmentation of the craniomaxillofacial region using porous hydroxyapatite granules. Plast Reconstr Surg. 2003;111(6):1808-1817. [47] Damien E, Revell PA. Coralline hydroxyapatite bone graft substitute: A review of experimental studies and biomedical applications. J Appl Biomater Biomech. 2004;2(2):65-73. [48] Ducheyne P, Qiu Q. Bioactive ceramics: the effect of surface reactivity on bone formation and bone cell function. Biomaterials. 1999;20(23-24):2287-2303. [49] Luo ZB, Zhang QB, Zhang ZQ, et al. Performance of coralline hydroxyapatite in sinus floor augmentation: a retrospective study. Clin Oral Investig. 2013;17(9): 2003-2010. [50] Fu K, Xu Q, Czernuszka J, et al. Characterization of a biodegradable coralline hydroxyapatite/calcium carbonate composite and its clinical implementation. Biomed Mater. 2013;8(6):065007. [51] Markel DC, Guthrie ST, Wu B, et al. Characterization of the inflammatory response to four commercial bone graft substitutes using a murine biocompatibility model. J Inflamm Res. 2012;5:13-18. [52] Moslemi N, Mousavi Jazi M, Haghighati F, et al. Acellular dermal matrix allograft versus subepithelial connective tissue graft in treatment of gingival recessions: a 5-year randomized clinical study. J Clin Periodontol. 2011;38(12): 1122-1129. [53] Thombre V, Koudale SB, Bhongade ML. Comparative evaluation of the effectiveness of coronally positioned flap with or without acellular dermal matrix allograft in the treatment of multiple marginal gingival recession defects. Int J Periodontics Restorative Dent. 2013;33(3):e88-94. [54] Wagshall E, Lewis Z, Babich SB, et al. Acellular dermal matrix allograft in the treatment of mucogingival defects in children: illustrative case report. ASDC J Dent Child. 2002; 69(1):39-43, 11. [55] Batista EL Jr, Batista FC. Managing soft tissue fenestrations in bone grafting surgery with an acellular dermal matrix: a case report. Int J Oral Maxillofac Implants. 2001;16(6):875-879. [56] Koudale SB, Charde PA, Bhongade ML. A comparative clinical evaluation of acellular dermal matrix allograft and sub-epithelial connective tissue graft for the treatment of multiple gingival recessions. J Indian Soc Periodontol. 2012; 16(3):411-416. [57] Zuolo ML, Ferreira MO, Gutmann JL. Prognosis in periradicular surgery: a clinical prospective study. Int Endod J. 2000;33(2):91-98. [58] Luczyszyn SM, Papalexiou V, Novaes AB Jr, et al. Acellular dermal matrix and hydroxyapatite in prevention of ridge deformities after tooth extraction. Implant Dent. 2005;14(2): 176-184. [59] Sàndor GK, Kainulainen VT, Queiroz JO, et al. Preservation of ridge dimensions following grafting with coral granules of 48 post-traumatic and post-extraction dento-alveolar defects. Dent Traumatol. 2003;19(4):221-227. [60] Fowler EB, Breault LG. Ridge augmentation with a folded acellular dermal matrix allograft: a case report. J Contemp Dent Pract. 2001;2(3):31-40. [61] Sadat Mansouri S, Ayoubian N, Eslami Manouchehri M. A comparative 6-month clinical study of acellular dermal matrix allograft and subepithelial connective tissue graft for root coverage. J Dent (Tehran). 2010;7(3):156-164. [62] Artzi Z, Wasersprung N, Weinreb M, et al. Effect of guided tissue regeneration on newly formed bone and cementum in periapical tissue healing after endodontic surgery: an in vivo study in the cat. J Endod. 2012;38(2):163-169. [63] Steele MH, Seagle MB. Palatal fistula repair using acellular dermal matrix: the University of Florida experience. Ann Plast Surg. 2006;56(1):50-53. [64] de Souza SL, Novaes AB Jr, Grisi DC, et al. Comparative clinical study of a subepithelial connective tissue graft and acellular dermal matrix graft for the treatment of gingival recessions: six- to 12-month changes. J Int Acad Periodontol. 2008;10(3):87-94. [65] Thomas LJ, Emmadi P, Thyagarajan R, et al. A comparative clinical study of the efficacy of subepithelial connective tissue graft and acellular dermal matrix graft in root coverage: 6-month follow-up observation. J Indian Soc Periodontol. 2013;17(4):478-483. |
| [1] | Zhang Mi, Wu Saixuan, Dong Ming, Lu Ying, Niu Weidong. Expression of interleukin-24 in a mouse model of periapical periodontitis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 679-684. |
| [2] | Yang Caihui, Liu Qicheng, Dong Ming, Wang Lina, Zuo Meina, Lu Ying, Niu Weidong. Serine/threonine protein kinases can promote bone destruction in mouse models of chronic periapical periodontitis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(23): 3654-3659. |
| [3] | Xu Nuo, Cao Zhen, Li Xiaojie, Shi Chun. MicroRNA-21 regulates proliferation and differentiation of osteoclasts in periodontitis [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(8): 1225-1230. |
| [4] | Zhou Pengfei, Lin Jing, Chen Yuying, Lin Minkui. Canine dental pulp stem cells-polyglycolic acid scaffold complex for canine periodontal tissue defect [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(34): 5526-5531. |
| [5] | Wu Dalei, Zhou Shouheng, Yan Jianwei, Li Bo, Xu Nuo, Shi Chun, Gao Yang. Alcohol extract of Eucommia ulmoides Oliv. promotes bone healing in rats with periapical periodontitis [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(23): 3685-3689. |
| [6] | Wu Hui, Xu Nuo, Wang Qian, Shi Chun, Jiang Long. Screening chronic periodontitis-related genes using whole-genome expression profiling [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(23): 3615-3620. |
| [7] |
Zhang Yujing, Peng Yuzhi, Liu Baozhen, Jing Fang.
Effect of Xianling Gubao Capsule
on alveolar bone mass in postmenopausal women with periodontitis: a cone-beam
CT evaluation
|
| [8] | Xu Huijun, Shi Dongmei, Zhang Mi, Wu Saixuan, Dong Ming, Lu Ying, Niu Weidong. Effect of sex combing protein 1 on proliferation and differentiation of osteoblasts in inflammatory microenvironment#br# [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(1): 130-135. |
| [9] | Yang Chunhe, Zhang Hong, Dong Ming, Wang Lina, Niu Weidong. Expression of PLCgamma2 in a wild-type mouse model of chronic periapical periodontitis [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(7): 1057-1062. |
| [10] | Zuo Meina1, Wang Lina1, Han Shujuan2, Dong Ming3, Niu Weidong1. Expression of myeloid differentiation factor 88 in a rat model of experimental periapical periodontitis [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(7): 1068-1072. |
| [11] | Zhao Xiangyu, Zhang Guirong, Guo Chuanbo, Shi Chun, Wu Liuzhong. Increased expression of long-chain non-coding RNA LINC00511 in periodontitis promotes osteoclast proliferation [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(33): 5360-5365. |
| [12] | Zhang Hong, Ye Dandan, Dong Ming, Niu Weidong. Expression of RANKL in chronic periapical periodontitis in mice [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(3): 391-395. |
| [13] | Yang Na1, Bao Pingping2, Lei Tao2. Adiponectin levels in plasma and periodontal tissue of mouse models of diabetic periodontitis treated by adiponectin [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(23): 3692-3697. |
| [14] | Du Shasha, Cai Zhiguo, Yang Kun, Liu Qi. Dental-derived mesenchymal stem cells promote periodontal tissue regeneration: possibility and prospects [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(17): 2782-2788. |
| [15] | Ma Jinbao1, Wang Qian2, Dong Ming3, Bai Hua2. Expression of autophagy-associated protein light chain 3B in human pulpitis and periapical periodontitis [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(15): 2364-2368. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||