Chinese Journal of Tissue Engineering Research
Previous Articles Next Articles
Vascularization of heparin-chitosan-coated acellular bone matrix combined with vascular bundles in repair of segmental bone defects
Zhang Chun-mei1, Tian Hong-ling2, Zhao Jie1, Teng Yun1, Yu Shao-fen1, Sun Xin-jun1
- 1 Research Institute of Orthopedics Surgery, the 89th Hospital of PLA, Weifang 261021, Shandong Province, China
2 Health Center of Material Procurement Station, Logistics Department of Jinan Military Region, Jinan 250022, Shandong Province, China
-
Received:2012-09-29Revised:2012-10-31Online:2013-05-21Published:2013-05-21 -
Contact:Sun Xin-jun, Associate chief physician, Research Institute of Orthopedics Surgery, the 89th Hospital of PLA, Weifang 261021, Shandong Province, China -
About author:Zhang Chun-mei★, Master, Associate chief technician, Research Institute of Orthopedics Surgery, the 89th Hospital of PLA, Weifang 261021, Shandong Province, China 13637895821@163.com -
Supported by:the Project of Military “Eleventh Five-Year” Plan, No. 06MA096
CLC Number:
Cite this article
Zhang Chun-mei, Tian Hong-ling, Zhao Jie, Teng Yun, Yu Shao-fen, Sun Xin-jun. Vascularization of heparin-chitosan-coated acellular bone matrix combined with vascular bundles in repair of segmental bone defects[J]. Chinese Journal of Tissue Engineering Research, doi: 10.3969/j.issn.2095-4344.2013.21.020.
share this article

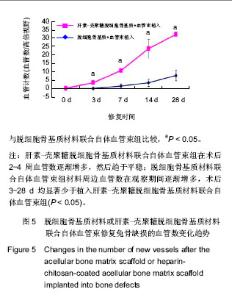
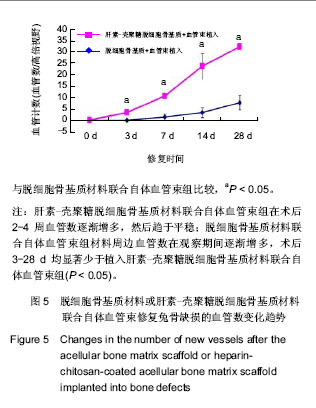
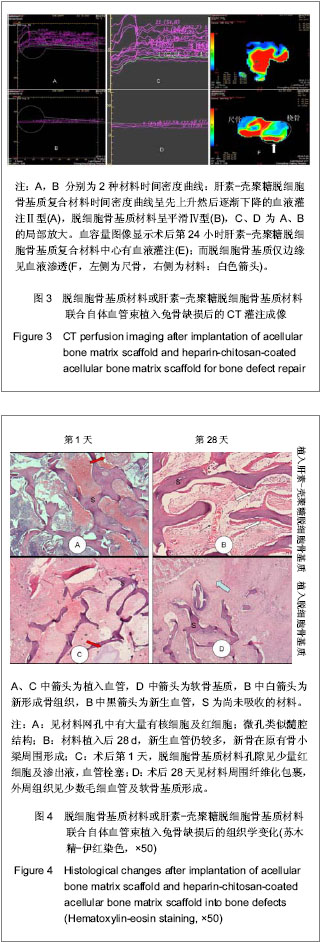
2.5 实验组与对照组CT灌注扫描成像结果 CT灌注扫描结果显示时间-密度曲线的形态明显不同,实验组显示为Ⅱ型,对照组表现为Ⅳ型,见图3A-D。24 h后实验组血容量显著高于对照组,且复合材料侧中心部位有明显的血液灌注,而对照组在植入物周围有血液渗透,血容量、血流量显著低于实验组,见图3E,F,此种趋势持续到第4周。 2.6 实验组与对照组标本组织学观察 单纯ACBM材料植入后24 h见植入血管栓塞,材料微孔中大量淡红色渗液伴少量细胞(以红细胞为主)。HC/ACBM材料侧微孔间细胞较对照侧增多,其中以有核细胞占多数伴有红细胞;术后第3天在骨小梁间可见微血管出现,之后逐渐增多。而ACBM侧植入后第7天,在材料周围软组织中见少量新生血管。术后14 d HC/ACBM复合材料组血管数进一步增多,对照组仅在周围组织中出血少量毛细血管。且HC/ACBM复合材料中血管数增多趋势较对照组快,且这一趋势持续到术后第28天。此时,ACBM材料外周有软骨基质形成,而HC/ACBM材料周围及网孔中见大量新骨形成,见图4。"
| [1] Reichert JC,Carvalho C,Mulhaupt R,et al.The challenge of establishing preclinical models for segmental bone defect research.Biomaterials.2009;30(12):2149-2163.[2] Lasanianos NG,Kanakaris NK,Giannoudis PV.Current management of long bone large segmental defects. Orthopaed Trauma.2010;24(2):149-163.[3] Ikada Y.Challenges in tissue engineering.J R Soc Interface. 2006;3(10):589-601.[4] Griffith LG,Naughton G. Tissue engineering- current challenges and expanding opportunities. Science.2002;295: 1009-1014.[5] Khetani SR,Bhatia SN. Engineering tissues for in vitro applications.Curr Opin Biotechnol.2006;17:524-531.[6] MacNeil S. Progress and opportunities for tissue-engineered skin. Nature. 2007;445:874-880.[7] Jain RK,Au P,Tam J,et al.Engineering vascularized tissue. Nat Biotechnol. 2005;23(7):821-829.[8] Rouwkema J,Rivron NC,van Blitterswijk CA.Vascularization in tissue engineering.Trends Biotechnol.2008;26:434-441.[9] Demirdogen B,Elcin AE,Elcin YM.Neovascularization by bFGF releasing hyaluronic acid-gelatin microspheres: in vitro and in vivo studies.Growth Factors.2010;28(6):426-436.[10] Laschke MW,Rucker M,Jensen G,et al.Improvement of vascularization of PLGA scaffolds by inosculation of in situ-preformed functional blood vessels with the host microvasculature. Ann Surg.2008;248(6):939-948.[11] Chen X,Aledia AS,Ghajar CM,et al.Prevascularization of a fibrin-based tissue construct accelerates the formation of functional anastomosis with host vasculature. Tissue Eng A. 2009;15:1363-1371.[12] Lokmic Z,Stillaert F,Morrison WA,et al. An arteriovenous loop in a protected space generates a permanent, highly vascular, tissue-engineered construct. J FASEB.2007;21(2):511-522.[13] Polykandriotis E,Arkudas A,Beier JP,et al. Intrinsic axial vascularization of an osteoconductive bone matrix by means of an arteriovenous vascular bundle. Plast Reconstr Surg. 2007;120:855-868.[14] Novosel EC,Kleinhans C,Kluger PJ.Vascularization is the key challenge in tissue engineering. Adv Drug Del Rev.2011;63 (4-5): 300-311.[15] Gorbet MB,Sefton MV.Biomaterial associated thrombosis: roles of coagulation factors, complement, platelets and leukocytes.Biomaterials. 2004;25(26):5681-5703.[16] Meng S,Liu ZJ,Shen L.The effect of a layer-by-layer chitosan-heparin coating on the endothelialization and coagulation properties of a coronary stent system. Biomaterials.2009;30:2276-2283.[17] Sun XJ,Peng W,Ren ML,et al.Heparin-chitosan-coated acellular bone matrix enhances perfusion of blood and vascularization in bone tissue engineering scaffolds. Tissue Eng Part A. 2011;17(19-20):2369-2378.[18] Shastri VP. Future of regenerative medicine: challenges and hurdles. Artif Organs.2006;30(10): 828-834.[19] Borselli C,Ungaro F,Oliviero O,et al.Bioactivation of collagen matrices through sustained VEGF release from PLGA microspheres. J Biomed Mater Res A. 2010;92(1):94-102.[20] Yang J,Zhou W,Zheng W,et al. Effects of myocardial transplantation of marrow mesenchymal stem cells transfected with vascular endothelial growth factor for the improvement of heart function and angiogenesis after myocardial infarction. Cardiology.2007; 107(1):17-29.[21] Sekine H,Shimizu T,Hobo K,et al.Endothelial cell coculture within tissue-engineered cardiomyocyte sheets enhances neovascularization and improves cardiac function of ischemic hearts.Circulation.2008;118: S145-S152.[22] Tanaka Y,Tsutsumi A,Crowe DM,et al.Generation of an autologous tissue (matrix) flap by combining an arteriovenous shunt loop with artificial skin in rats: preliminary report. Br J Plast Surg.2000;53(1):51-57.[23] Yang J,Yamato M,Shimizu T,et al. Reconstruction of functional tissues with cell sheet engineering. Biomaterials. 2007;28(34): 5033-5043.[24] Santos MI,Tuzlakoglu K,Fuchs S,et al.Endothelial cell colonization and angiogenic potential of combined nano- and micro-fibrous scaffolds for bone tissue engineering. Biomaterials. 2008;29(32):4306-4313.[25] Nilsson PH, Engberg AE, Bäck J,et al.The creation of an antithrombotic surface by apyrase immobilization.Biomaterials.2010;31(16):4484-4491.[26] 26.Sperling C,Salchert K,Streller U,et al.Covalently immobilized thrombomodulin inhibits coagulation and complement activation of artificial surfaces in vitro. Biomaterials.2004;25(21):5101-5113.[27] Venkatesan J,Kim SK. Chitosan composites for bone tissue engineering--an overview. Mar Drugs.2010; 8(8): 2252-2266.[28] Vogler EA,Siedlecki CA. Contact activation of blood–plasma coagulation. Biomaterials.2009;30:1857-1869.[29] Sun XJ,Wang ZG,Zhu PF,et al.Zhonghua Chuangshang Zazhi. 2005;21(11):833-837.孙新君,王正国,朱佩芳,等.脱细胞骨基质材料的特性及生物安全性观察[J].中华创伤杂志, 2005,21(11);833-837.[30] Kujawa P,Schmauch G,Viitala T,et al. Construction of viscoelastic biocompatible films via the layer-by-layer assembly of hyaluronan and phosphorylcholine-modified chitosan.Biomacromolecule.2007;8:3169-176.[31] Qiao K,Liu H,Hu N.Layer-by-layer assembly of myoglobin and nonionic poly (ethylene glycol) through iondipole interaction: an electrochemical study. Electrochim Acta.2008;53: 4654-4662.[32] Dobrucki LW,Tsutsumi Y,Kalinowski L,et al. Analysis of angiogenesis induced by local IGF-1 expression after myocardial infarction using microSPECT-CT imaging. J Mol Cell Cardiol.2010;48(6):1071-1079.[33] Kämena A, Streitparth F, Grieser C, et al. Dynamic perfusion CT: Optimizing the temporal resolution for the calculation of perfusion CT parameters in stroke patients. Eur J Radiol. 2007;64:111-118.[34] Wiest R,von Bredow F,Schindler K,et al.Detection of regional blood perfusion changes in epileptic seizures with dynamic brain perfusion CT—A pilot study. Epilepsy Res.2006;72(2-3): 102-110.[35] Aralasmak A, Karaali K, Akyuz M, et al. MR imaging and CT perfusion findings of an extraventricular neurocytoma. Eur J Radiol Extra.2009;69: e53-e56.[36] Bai K,Huang Y,Jia X, et al. Endothelium oriented differentiation of bone marrow mesenchymal stem cells under chemical and mechanical stimulations. J Biomech.2010;43(6): 1176-1181.[37] Oswald J,Boxberger S,Jorgensen B,et al.Mesenchymal stem cells can be differentiated into endothelial cells in vitro. Stem Cells.2004;22:377-384.[38] Hristov M,Erl W,Weber PC.Endothelial progenitor cells: mobilization, differentiation, and homing.Arterioscler Thromb Vasc Biol.2003;23(7):1185-1189.[39] Avci-Adali M,Ziemer G,Wendel HP.Induction of EPC homing on biofunctionalized vascular grafts for rapid in vivo self-endothelialization-A review of current strategies. Biotechnol Adv. 2010;28(1):119-129.[40] Grayson WL,Bhumiratana S,Cannizzaro C,et al. Effects of initial seeding density and fluid perfusion rate on formation of tissue-engineered bone. Tissue Eng Part A.2008;14(11): 1809-1820.[41] Oest ME,Dupont KM,Kong HJ,et al. Quantitative assessment of scaffold and growth factor-mediated repair of critically sized bone defects. J Orthop Res. 2007;25(7):941-950.[42] Dawson JI,Oreffo RO.Bridging the regeneration gap: Stem cells, biomaterials and clinical translation in bone tissue engineering. Arch Biochem Biophys. 2008;(473):124-131.[43] Reichert JC,Saifzadeh S,Wullschleger ME,et al.The challenge of establishing preclinical models for segmental bone defect research. Biomaterials.2009;30(12):2149-2163.[44] Pearce AI,Richards RG,Milz S,et al. Animal models for implant biomaterial research in bone: a review. Eur Cell Mater. 2007;13:1-10.[45] Liu F,Yu SF,Wang ZG,et al. Biomimetic construction of large engineered bone using hemoperfusion and cyto-capture in traumatic bone defect. BioResearch Open Access.2012; 1(5): 247-251.[46] Gugala Z,Lindsey RW,Gogolewski S.New approaches in the treatment of critical size segmental defects in long bones. Macromol Symp.2007;253:147-161. |
| [1] | Li Li, Ma Li. Immobilization of lactase on magnetic chitosan microspheres and its effect on enzymatic properties [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 576-581. |
| [2] | Liu Liu, Zhou Qingzhu, Gong Zhuo, Liu Boyan, Yang Bin, Zhao Xian. Characteristics and manufacturing techniques of collagen/inorganic materials for constructing tissue-engineered bone [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 607-613. |
| [3] | Li Xinping, Cui Qiuju, Zeng Shuguang, Ran Gaoying, Zhang Zhaoqiang, Liu Xianwen, Fang Wei, Xu Shuaimei. Effect of modification of β-tricalcium phosphate/chitosan hydrogel on growth and mineralization of dental pulp stem cells [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(22): 3493-3499. |
| [4] | Zhou Anqi, Tang Yufei, Wu Bingfeng, Xiang Lin. Designing of periosteum tissue engineering: combination of generality and individuality [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(22): 3551-3557. |
| [5] | Lang Limin, He Sheng, Jiang Zengyu, Hu Yiyi, Zhang Zhixing, Liang Minqian. Application progress of conductive composite materials in the field of tissue engineering treatment of myocardial infarction [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(22): 3584-3590. |
| [6] | Chen Siyu, Li Yannan, Xie Liying, Liu Siqi, Fan Yurong, Fang Changxing, Zhang Xin, Quan Jiayu, Zuo Lin. Thermosensitive chitosan-collagen composite hydrogel loaded with basic fibroblast growth factor retards ventricular remodeling after myocardial infarction in mice [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(16): 2472-2478. |
| [7] | Liu Feng, Zhang Yu, Wang Yanli, Luo Wei, Han Chaoshan, Li Yangxin. Application of temperature-sensitive chitosan hydrogel encapsulated exosomes in ischemic diseases [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(16): 2479-2487. |
| [8] | Li Jie, Xu Jianzhen, Hu Ping, Lei Qiqi, Zhang Wenning, Ao Ningjian . Preparation and performance evaluation of carboxymethyl chitosan/oxidized glucomannan/Panax notoginseng compound sponge dressing for chronic wound [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(16): 2528-2534. |
| [9] | Xie Jian, Su Jiansheng. Advantages and characteristics of electrospun aligned nanofibers as scaffolds for tissue engineering [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(16): 2575-2581. |
| [10] | Ji Qi, Yu Zhengwen, Zhang Jian. Problems and trends of technique and clinical application of metallic biomaterials prepared by three-dimensional printing technology [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(16): 2597-2604. |
| [11] | Qian Nannan, Zhang Qian, Yang Rui, Ao Jun, Zhang Tao. Mesenchymal stem cells in the treatment of spinal cord injury: cell therapy and combination of new drugs and biomaterials [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(13): 2114-2120. |
| [12] | Jia Wei, Zhang Mandong, Chen Weiyi, Wang Chenyan, Guo Yuan. Effects of femoral prosthetic materials on artificial knee arthroplasty performance [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(10): 1477-1481. |
| [13] | Wang Qian, Li Lu, Shu Jingyuan, Dong Zhiheng, Jin Youshi, Wang Qingshan. Micro-morphology and phase of zirconia-based nano-hydroxyapatite functional gradient biomaterials [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(10): 1517-1521. |
| [14] | Feng Xiaoxia, Hou Weiwei, Jin Xiaoting, Wang Xinhua. Construction of periodontal biomimetic membrane with electrospun poly(lactic-co-glycolic acid) nanofibers and electrosprayed chitosan microspheres [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(4): 511-516. |
| [15] | Li Li, Ma Li, Li He. Preparation and characterization of magnetic chitosan microspheres [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(4): 577-582. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||